Journal of
eISSN: 2373-4345


Research Article Volume 1 Issue 4
Dental Biomaterials, College of Oral and Dental Medicine, Misr University for Science & Technology, Egypt
Correspondence: Nagy Abdul-Samee Abdul-Hameed, Dental Biomaterials, College of Oral and Dental Medicine, Misr University for Science & Technology, Al-Motamayez District, P.O. Box: 77, 6th of October City, Egypt, Tel 201000000000
Received: July 04, 2014 | Published: September 6, 2014
Citation: Abdul-Hameed NAS. Argon-ion laser vs. quartz-tungsten-halogen curing of polyacid modified composite resin restorative materials. J Dent Health Oral Disord Ther. 2014;1(4):113-119. DOI: 10.15406/jdhodt.2014.01.00026
This study evaluated the differences in mechanical properties (flexural strength, surface roughness, and micro hardness) of three commercially available compomer restorative materials (Compo glass F, F2000, and Dyract AP), that were cured by argon laser (AL) and the traditional visible light quartz-tungsten-halogen (QTH) sources. Twenty eight nominally identical disc-shaped specimens, from each material, were prepared in a cylindrical split Teflon mold (6mm diameter, 2 mm thickness; to allow for one-step curing regime). Half of the specimens were cured by 40s. Exposure to a QTH curing unit and the other half by 10s. Exposure to AL on top and bottom surfaces. Fourteen samples from each material (seven for each curing type) were subjected to surface profile-measuring instrument. Samples used for surface roughness were also used to measure Knoop Hardness Number (KHN). The bi-axial flexure strength, of the remaining disc-shaped specimens was determined using the ‘piston on ball’ technique using the universal testing instrument to apply a compressive load perpendicularly through a ball indenter 4 mm in diameter at a crosshead speed of 1 mm/min. Results of the work showed that there was no statistical significant difference between the two techniques of compomer curing (P>0.05). It was concluded that the argon laser cured compomer effectively as traditional visible light but with time saving.
Keywords: compomer, Quartz-Tungsten-Halogen (QTH) curing, argon on laser curing, surface roughness, hardness, bi-axial flexure strength
QTH, quartz-tungsten-halogen; AL, argon laser; KHN, knoop hardness number; LCU, light-curing units; LED, light-emitting diode; PAC, plasma arc; VL, visible light; MMA, methyl ethacrylate
Polyacid-modified composite resins, simply known as compomers, are among the latest group of tooth colored restorative materials now available to the dental profession. Compomers demonstrated better morphologic and mechanical characteristics than other hybrid restorative materials and are comparable with ultrafine midway-filled composites.1,2 Their matrix consists of conventional composite resin monomers (bis-GMA or urethane dimethacrylate), together with novel monomers containing a small number of carboxylic acid functional groups. Their filler consists of inert silica particles, together with a small amount of acid-leachable glass, strontium aluminosilicate or barium aluminosilicate based, capable of forming glass-ionomer type structures within the material.3 They set initially by light-activated addition polymerization followed by an acid-base reaction that arises from sorption of water in situ because they do not have water in their composition.4
The role of blue light is crucial because it initiates the polymerization process. Thus far, several types of light sources have been introduced for the light curing of dental restorative materials.5,6 There are four main types of light-curing units (LCU) used by dentists to polymerize light-cured resin-based composites: quartz-tungsten-halogen (QTH), light-emitting diode (LED), Plasma Arc (PAC), and Argon-Laser units (AL).7−10
Recently, there has been an interest in using an argon laser to initiate polymerization of light-activated materials.11 The argon laser, the active medium of which is argon gas, produces light at two wavelengths. The 488 nm blue light is commonly used to initiate the polymerization of restorative composite materials. The 514nm blue green light has maximum absorbance in tissues that are composed of pigmented molecules such as hemosiderin and melanin. Both wavelengths of the argon laser are poorly absorbed by non-pigmented and hard tissues.12
Light-cured dental materials use a diketone initiator such as camphoroquinone and a reducing agent such as a tertiary amine to initiate polymerization.13 This photo initiator system is very sensitive to light in the blue region of the visible light spectrum, with the peak activity centered on 480 nm.14 The argon laser is monochromatic and emits light over a narrow band of wavelengths in the blue green spectrum (457.9 to 514.5nm), making it ideally suited to polymerize light-activated materials as well as cutting soft tissues.15
Conventional visible light curing units (VL) also emit energy centered around 480 nm, and were used to cure visible-light materials. The argon laser (AL) light has energy of more efficiency than conventional visible-light sources because
In contrast, the power density of conventional visible light decreases dramatically with distance, due to greater light divergence from the source.18−20 Finally, visible light curing units use bulbs, reflectors, and filters, which may degrade and decrease curing efficiency.21 These factors may contribute to the increased efficiency of argon laser curing of composite resins compared with visible light curing.22 In addition the QTH bulbs are being phased out in many countries.8,23,10
Several studies looked at physical properties of composite resin polymerized with argon laser versus a conventional visible light. One study24 showed that 5 seconds of argon laser exposure created a composite with higher compressive strength than 20 seconds of visible curing light. It showed also that with 75% less time the argon laser could produce equal or better results than the conventional halogen light. Other studies showed the positive effects of the argon laser, as compared with the halogen light on:
The aim of the present work was to compare biaxial flexure strength values, surface roughness and micro hardness of three commercially available compomers that were cured using the traditional visible light (QTH) and the argon laser (AL) sources.
Three light-activated compomer materials (Table 1) were used.
|
Material |
Manufacturer |
Composition |
|
Compoglass F
F 2000
Dyract AP |
Ivoclar –Vivadent.
3M Dental Products, St. Paul, Minn. Detrey, Dentsply.
|
Propxylated bis-GMA, cycloaliphatic dicarboxylic acid dimethacrylate, tetraethylene GDMA, UDMA, silanized spheroidal mixed oxide, yetrium trifloride, silanized Ba-florosilicate glass. Bis methacrylates, other light-curing co-polymers, Ca-Al-silicate glass. Florosilicat glass, acidic polymerizable monomers and other light activated polymers. |
Table 1 Materials used
Specimen preparation
Twenty eight identical disc-shaped specimens, from each material, were prepared in a cylindrical split Teflon mold (6 mm diameter, 2 mm thickness; to allow for a one-step curing regime). Half of them were cured by 40s exposure to a quartz-halogen lamp (XL3000, 3M Dental Product St. Paul, Minn.) visible-light curing unit (QTH), and the other half by 10s exposure to an argon laser (AL) (Figure 1) Argon-ion laser, Continuous mode, Fiber diameter 600, HGN, Salt Lake City, Utah, on top and bottom surfaces. The distance between the light source and specimen was standardized (Figure 2). The QTH produced the full power output of 470 mW, a 13mm spot size, and a power density of 345 mW/cm². The power output of the AL was maintained at 265 mW. Its spot size from the light tip was 6 mm diameter, resulting in a power density of 937 mW/cm².11 The light intensity of curing lights was checked regularly after every seven specimens preparation using radiometer. Specimens were stored in distilled water at 37 0C in a lightproof container for one week before testing.30

Biaxial flexure strength testing
The disc shaped test specimens were fractured biaxilly using the ‘piston on ball’ technique described by Shetty et al.,31 Specimens were concentrically supported on the three ball bearing (each 2.35mm in diameter) that were evenly spaced around a support circle with a radius of 10mm. Specimens were loaded using the universal testing instrument (Model 1193, Instron Limited, UK) to fracture by a compressive load applied perpendicularly through a ball indenter 4 mm in diameter at a crosshead speed of 1mm/min. To assist in uniform loading of the ball indenter on the specimen surface, a thin sheet of rubber was placed between the sample and the support. The bi-axial flexure strength (Table 2) was calculated according to equation:
|
Test |
Biaxial flexture strength in (MPa) |
t-value |
|
|
Curing method & time Material |
QTH (40-sec)
|
AL (10-sec)
|
|
|
Dyract AP F2000 Compo glass F
|
45.23±6.25 46.73±9.29 64.56±14.4 |
42.43±.3 47.32±11.23 68.12±8.39 |
0.90 NS 0.15 NS 0.57 NS
|
|
F-value |
8.52* |
20.28* |
|
Table 2 Means and standard deviation for biaxial flexture strength
NS: No significant difference P>0.05
*Highly significant difference P<0.01
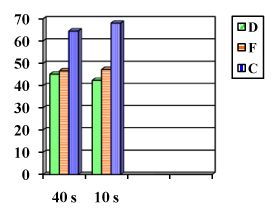
Vertical bars indicates no significant difference (P>0.05)
where σmax was the maximum tensile stress (MPa), P the measured load at fracture (N), ν the Poisson’s ratio for the material, a the radius of the support circle (mm), b the radius of disc specimen, t the thickness of disc specimen (mm) and ro* the equivalent radius of contact between the loading ball and the disc specimen, where loading can be considered uniform and given by the following equation:
Where ro the radius of the ball used as a piston on the loading surface. The Poisson’s ratio of a material is defined as the lateral contraction per unit breadth divided by the longitudinal extension per unit length and a value of 0.35 was substituted for the compomer materials tested.32,33 The sample thickness was measured at the point of fracture for each disc-shaped specimen using a micrometer screw gauge (Moore and Wright, Sheffield, England) accurate to 10 μm.
Surface roughness (Ra) testing
The specimens used for micro hardness testing were utilized for Ra investigation before conducting hardness measurement. The samples were subjected to a surface profile-measuring instrument Surteonic 3 (Rank Organization, Leicester, England). Five tracings were made at different locations on each surface using a tracing length and a cut-off value of 2-5mm. The Ra values are the mathematical mean values of the departure of the roughness profile from the mean line calculated by the machine.34
Hardness testing
The micro hardness was measured using a digital micro hardness tester HMV 2000, Shimatzu Corp. Japan (Figure 3 & Figure 4) with a Knoop indenter and a zeiss ‘Axiolab A’ metallographic microscope. A 50 gf load was applied through the indenter with a dwell time of 30s. The indentation print images were then projected to a computer monitor with a Hyper Had Sony CCD camera attached to the microscope. The indentation diagonal was measured with the aid of digital processing software. The Knoop micro hardness value is calculated from the following equation:
Where P is the indenter loading force in gf (1 gf = 0.0098 N), d is the longer diagonal of the indentation print in μm and HK is the Knoop hardness number (KHN) in Kg/mm² (1Kgf/mm²=9.81 MPa) 35. Five readings were taken for each specimen and the mean KHN was computed.
Data were collected and analyzed by student’s t-test to compare the corresponding curing techniques of the three materials tested. The data were also test showed no statically significant difference between Dyract AP and F 2000 compomer materials LSR = 17.205 (P > 0.05).
Surface roughness
Table 3 and Figure 5 summarize the mean and standard deviation of the flexural strength for the cured compomer materials by different light sources (QTH & AL). Student’s t-test showed no statistical significant difference for all compomer materials tested by either QTH or Al (P > 0.05). ANOVA test showed no statistical significant difference (P > 0.05) between compomer materials tested.
|
Test |
Surface roughness (Ra) |
t-value |
||
|
Curing method & time Material |
QTH (40-sec) |
AL (10-sec) |
||
|
Dyract AP F2000 Compo glass F
|
0.71±0.25 0.89±0.18 0.60±0.29
|
0.73±0.31 0.84±0.39 0.63±0.25
|
0.09 NS 0.31 NS 0.21 NS
|
|
|
F-value |
1.57 NS |
0.859 NS |
|
|
Table 3 Means and standard deviation for surface roughness
NS: No significant difference P>0.05
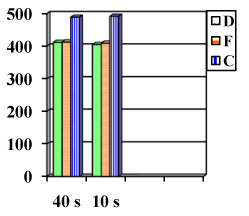
Micro hardness
Table 4 and Figure 6 summarize the mean and standard deviation of the micro hardness for the cured compomer materials by different light sources (QTH & AL). Student’s t-test showed no statistical significant difference for all compomer materials tested by either QTH or Al (P > 0.05). ANOVA test showed highly statistical significant difference (P < 0.01) between compomer materials tested. Student Newman-Keul multiple comparison test showed highly statistically significant difference between Compo glass F material and the other two compomer materials namely Dyract AP or F 2000 LSR = 29.32 and 19.08 respectively (P<0.01). The same test showed no statically significant difference between Dyract AP and F 2000 compomer materials [LSR = 25.6 (P>0.05).
Test |
Micro hardness number (KNH) (MPa) |
t-value |
|
|
Curing method & time Material |
QTH (40-sec)
|
AL (10-sec)
|
|
|
Dyract AP F2000 Compo glass F |
411.34±7.8 412.50±13.4 489.11±10.3 |
405.12±15.6 408.89±5.7 492.10±19.2 |
0.94 NS 0.67 NS 0.36 NS |
|
F-value |
140.46* |
93.56* |
|
Table 4 Means and standard deviation for micro hardness
NS: Non significant P>0.05
*Highly significant difference P<0.01
Vertical bars indicates non-significant difference P>0.05
Dentistry borrowed technology from other areas to help resolve the problem of lengthy setting time. It was noticed that the photo polymerization of inks, paints, and other coating materials was performed with acrylic monomers and ultraviolet. Thus in the late 1970s, a photo polymerized composite resin system was developed. Since then, many light sources are introduced to the dental market for polymerizing light cured restorative materials in an attempt to resolve the problem of lengthy setting time.36
The clinical performance of visible light cured restorative materials is related to their extent of cure. Quartz-tungsten-halogen light (QTH) curing is considered the scientific standard in 30-40 seconds exposure time against which new techniques of light curing should be compared. Clinicians must choose the appropriate type of light so that they can get acceptable restorations with optimal physico-mechanical properties and clinical performance.37 This is because the degree of polymerization of photo activated restorative materials depends upon the intensity and wave length of light emitted from the curing device, the curing time, the size, the location and the orientation of the light tip, shade, thickness and composition of the material being cured.
In the present work the biaxial flexure strength testing was used because it is known to be advantageous over uni-axial, diametral tensile and compressive testing methods.38−40 Disc-shaped specimens are centrally loaded at a pre-determined strain rate on an underlying support. The support may vary from a three ball bearing configuration arranged symmetrically 40 to a continuous knife-edge ring.38,40 The maximum tensile stresses occur within the central loading area, eliminating spurious edge failures associated with three-point flexure testing41 and samples are insensitive to specimen geometry and independent of flaw direction.
The smaller disc specimens (6mm diameter and 2mm thickness) utilized in the current work for bi-axial testing because of the improved representation of the volume and dimension of clinical restorations. The dimensions of the disc samples allow for complete and reproducible curing of the material, without the need for an overlapping irradiation procedure that is needed for three points loading. It has also been suggested that varying the type of support system, from a series of point supports to a complete knife-edge ring does not produce a significant difference in results,39 providing increased reliability of flexure strength data between different operators and across different test centers.
In the present study, argon laser used at a powers of 250 mW + 50 mW for 10 seconds per increment. This is because the argon laser with the same power intensity provided good curing of light-activated composite restorative materials in a shorter period of time with equal or better physical properties as compared to the conventional halogen curing light.15 Kelsey et al.16 showed that optimal results of composite curing could be accomplished with only 25 to 350 mW of argon laser power in 10 to 12 seconds of curing time. Studies continue to support the ability of the argon laser to cure composite fast and effectively.11,42,43,44 Vergas et al.11 reported adequately polymerized composite resin in 30% to 50% less time. Christensen and Christensen44 reported efficient polymerization in 10 seconds or less for five different resins.
Knoop indenter was used to study the hardness of different compomer materials cured by either AL or VL, since it produces low depth indentation with a low load. This indenter produces a reasonable print that would, otherwise, be measurable if for example a Vickers indenter was used under the same load.45
Regarding the effect of light source, the present work showed that the difference in flexural strength or hardness was not significant (P>0.05) for composers that were cured by either LA for 40 seconds or AL for 10 seconds. This could be attributed to the ability of argon laser to convert greater amount of monomer to polymer leaving minimal amount of residual monomer than if quartz halogen tungsten light is used in the final hardened compomer. Blankenau et al.17 showed that laser curing converted a greater amount of monomer to polymerized resin, leaving less unreactive monomer in the set composite than that cured with a visible light, and Losche27 reported a greater conversion rate of camphoroquinone with the argon laser while Kelsey et al.19 proved that argon laser curing results in superior characteristics of cured composite than QTH light sources. They attributed this to the narrower bandwidth (~40nm) generated by the argon laser than that generated by the QTH light sources. The camphoroquinone photo activated resins have their peak activity for conversion between 470 and 480 nm (13, 14). The argon laser is effective and beneficial in polymerizing these resins because the argon laser’s wavelengths of 476 nm and 488 nm are in this peak activity range.
Regarding the effect of compomer type, the present study proved that compo glass F showed the highest flexural strength and hardness and there was a significant difference between it and the other two types of composers used. The cause for this difference may be attributed to the degree to which each compomer has been modified, by the manufacturers, with resin-like components or polyacid like components. Manufacturers could replace only low percentage of the carboxylic acid (COOH) groups on the polyacrylic acid by methyl ethacrylate (MMA) groups resulting in a fewer covalent (resin like) cross linking in polymerization. Such material would consist of a matrix predominantly cross-linked by ionic bonding and would posse properties near that of conventional glass ionomers. In cases where more percentage of COOH groups were replaced by MMA groups, the material would polymerize largely as a resin by the formation of free radicals and subsequent cross linking by the formation of covalent bonds.46 The matrix of Compo glass F compomer materials contains propoxylated Bown’s resins (Bis-GMA) with other methacrylates. The matrix of F 2000 compomer materials contains Bis methacrylate. Dyract AP contains acidic polymerizable monomers and other light-curing polymers. The addition of these resins may be the cause of this difference in Flexural strength and hardness between the studied compomers.47 Another factor that may explain the difference in flexural strength and hardness between Compo glass F in one side and the other compomer materials used is the difference in silanization of their fillers. Compo glass F fillers are completely silanized but those of Dyract AP and F 2000 compomer materials are partially silanized. The partly silane treated filler particles do not provide optimal resin-filler bonding ability during polymerization.48
In this study there was no significant difference in the calculated Ra values of Compo glass F, F 2000, and Dyract AP which were between 0.60-0.89 μm whether they cured by AL or QTH. This could be attributed to the fact that the present study was designed to investigate the Ra of the compomer materials without the effect of finishing. Fortunately, this reported value was equivalent to Ra at the occlusal enamel contact (0.64±0.25μm), which is considered the standard with which to compare the Ra value for a restorative material.49,50
Within the limits of this work, the following conclusions were drawn. Argon ion laser curing light device cured photo-activated compomer restorative materials as efficient as conventional quartz-halogen-tungsten light curing devices but with shorter time. Argon ion laser curing light device reduced the time of curing for photo-activated compomer restorative materials to 1/4th of that of conventional quartz-halogen-tungsten light curing devices. Compo glass F compomer had the highest Flexural strength and hardness among the investigated compomer materials. Surface roughness of the three-compomer materials tested did not differ whether cured by AL or QTH.
Laser photo curing of compomer might possibly allow the reduction of irradiation periods and thus saves time for both clinicians as well as patients which are very critical especially in pediatric one.
None.
The author declares that there is no conflict of interest.

©2014 Abdul-Hameed. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.