Journal of
eISSN: 2574-9943


Short Communication Volume 6 Issue 2
1Consultant, Sparsh Clinic, Deshmukh Road, 1st gate, Tilakwadi, Belagavi 590006, India
2Resident, Belagavi Institute of Medical Sciences, BR Ambedkar Road, Belagavi 590001, India
Correspondence: Naveen Manohar, Resident, Department of Dermatology, Room No. 24, Belagavi, Institute of Medical Sciences, BR Ambedkar Road, Belagavi 590001, Karnataka, Tel 9902929077
Received: April 30, 2022 | Published: May 17, 2022
Citation: Kamoji S, Manohar N. Thinker’s plaque: a sign of boredom or wisdom? J Dermat Cosmetol. 2022;6(2):29-30. DOI: 10.15406/jdc.2022.06.00203
Acquired hypermelanosis of the skin is a common condition that can develop secondary to various causes, such as topical application of irritants, repeated friction, ultraviolet radiation, and aging. The submental area is generally spared from environmental insults, such as exposure to ultraviolet radiation, due to its anatomical location. However, hypermelanosis of the submental area is a common complaint that brings patients to a dermatologist. In recent times, the number of patients presenting with this problem has increased probably due to the practice of wearing masks during the COVID-19 pandemic. Usually, the typical patient is a young woman who is cosmetically conscious and is distressed with this peculiar lesion under the chin. The lesion is generally asymptomatic except for the distress that it causes the patient. However, in some cases, the patient may complain of itching or thickened or rough skin. Inspection reveals a triangular area of hypermelanosis confined to the approximately lateral half of the submental area. Sometimes the area may present discrete horny follicular prominences. Additionally, the skin may demonstrate lichenification or plaque-like thickening without any particularly distinct patterns (Figure 1). Dermoscopy of the affected area reveals well-defined follicular prominences over a background of mildly hyperpigmented skin. Some areas may demonstrate fine scales as well (Figure 2). However, signs of inflammation are absent in these lesions. The lack of symptoms and the benign dermoscopic findings suggest that a biopsy is not required in such cases.

Figure 1 The submental area in a 20-year-old female shows a hypermelanotic plaque, interspersed with horny papules confined to one half of chin.
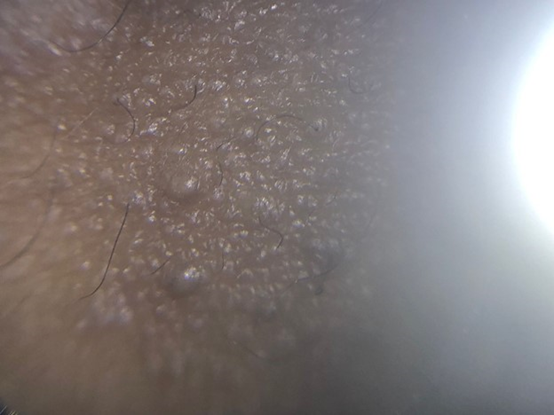
Figure 2 Dermoscopy shows papules over a blanket of hyperpigmentation, slightly increased skin markings and fine scaling in some parts of affected area.
An interesting observation is that such hypermelanosis is generally predominant on the non-dominant side—it is right-sided in a left-handed person and left-sided in a right-handed person. It is common for a person to rest their face on the non-dominant open palm while sitting upright and performing a task with the dominant hand. For example, when one is lost deep in thought, they may assume a similar posture unconsciously as it is easy to rest the face in this manner. Similarly, while attending a lecture, right-handed students may rest their chin on their left palms while taking notes since it can be a monotonous, and rather boring, activity. Akin to the posture of the fist and face in the famous sculpture “The Thinker” by Auguste Rodin, one may be lost deep in thought and not realize the frequent pressure and friction impacting the submental area. We have named this benign and harmless entity the ‘Thinker’s Plaque’. It is commonly seen in daydreamers, such as students. Continuous application of friction and pressure over the submental area results in a form of frictional dermatitis,1 which can become exacerbated due to additional friction from facemasks over the area while speaking or turning the head. This is especially true in cases of surgical masks and N95 masks that include rigid margins that are applied tightly over the nose and mouth using adjustable straps.2
The differential diagnosis for such presentations includes keratosis pilaris, phrynoderma, lichen spinulosus, and frictional dermatitis. Due to the unique location of the presenting lesion and the lack of other features, such as inflammation, alopecia, and associated features of rare genodermatoses, the most likely diagnosis is frictional dermatitis. A limitation in our observations is the lack of histopathological examination of the tissue. These patients presented to a private clinic and refused to undergo an invasive procedure, such as a biopsy, before a trial of topical formulations. Since it is primarily a cosmetic condition of keratosis and hyperpigmentation, topical triple combination therapy with 2% hydroxyquinone, 0.01% fluocinolone acetonide, and 0.025% tretinoin3 along with abstinence from the habit of resting the chin over the palm typically reverses the condition in a few weeks. In rare cases of advanced lesions of the ‘Thinker’s Plaque’, the lichenified skin may require mild topical steroids to revert it to normal skin.
None.
None.

©2022 Kamoji, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.