Journal of
eISSN: 2574-9943


Case Report Volume 2 Issue 1
Department of Dermatolgy, Dermatology Center Dona Lib
Correspondence: Larissa Karine Leite Portocarrero, Department of Dermatolgy, Dermatology Center Dona Lib
Received: May 26, 2017 | Published: February 19, 2018
Citation: Quental KN, Sousa ARDD, Pontes MADA, et al. Non-invasive diagnosis of Netherton syndrome. J Dermat Cosmetol. 2018;2(1):72-74. DOI: 10.15406/jdc.2018.02.00045
Netherton syndrome is a rare autosomal recessive genodermatosis characterized by diffuse erythema, specific hair shaft abnormality, such as invaginata trichorrhexis or bamboo hair, and atopic manifestations. The incidence of Netherton syndrome is estimated at approximately 1 in 200.000 and is considered a cause of up to 18% of congenital erythroderma. During childhood, the diagnosis becomes challenging because of the wide clinical overlap with other ichthyosis and atopic dermatitis. We report a case of a female patient referred as severe atopic dermatitis, whose clinical findings of ichthyosis linearis circumflexa and trichorrhexis invaginata determined the suspicion of Netherton syndrome and the tricoscopic evaluation, associated with electron microscopy, allowed the visualization of trichorrhexis invaginata and determined the diagnostic confirmation.
Keywords: Netherton syndrome, trichorrhexis invaginate, ichthyosis linearis circumflex, LEKT1, Pili torti
A 13-year-old female patient had erythematous pruritic lesions, disseminated since birth. She reported episodes of asthma and rhinitis. Her consanguineous parents denied similar family history. Initially the patient was diagnosed as severe atopic dermatitis, and achieved significant improvement during use of Cyclosporine and moderate but temporary with methotrexate. She had high serum immunoglobulin E and hypereosinophilia. Histopathological findings revealed subcorneal cleavage, spongiosis and neutrophilic dermal infiltrates. Despite treatment, patient presents desquamation and pruritus unchanged, then new hypotheses as congenital ichthyosiform erythroderma, Dermatitis herpetiformis and Pemphigus herpetiformis were made. During clinical follow-up, the patient developed multiple erythematous lesions, serpiginous and polycyclic plaques in upper limbs. The lesions were bordered by a distinct “double-edged” scale (Figure 1), diffuse xerosis, lichenification in flexures, and dry and brittle hair. The new histological examination revealed hyperkeratosis, hypogranulosis and psoriasiform acanthosis. To the tricoscopy, optical and electron microscopy, the hair shaft presented torsion and distal invagination on proximal (Figures 2-4), a specific finding that allowed the diagnosis of Netherton Syndrome.

Figure 1 Multiple erythematous, serpiginous and polycyclic plaques. The lesions were bordered by a distinct “double-edged” scale, clinical findings of ichthyosis linearis circumflexa.
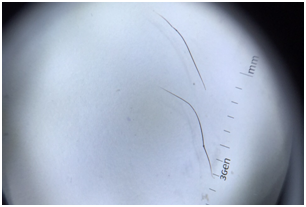
Figure 2 Hair shaft presenting torsion and distal invagination on proximal, a specific finding of trichorrhexis invaginata or “bamboo hair” (Dermatoscopy under polarized light, Dermlite, 3Gen LLC, 10x).
Netherton Syndrome is caused by mutations located on chromosome 5q3132 in both copies of the SPINK5 gene, which encodes the lymphoepithelial Kazal type-related inhibitor (LEKT1). Loss of LEKT1 activity causes increased proteolysis, which impairs lipid balance in the corneal layer and favors the formation of surface cracks.1,2
Hair analysis shows reduced numbers of bisulfidic bonds and poor cortical cell coherence. This focal softening of the hair allows intussusception of the distal end within a proximal dilation in a chalice, resulting in trichorrhexis invaginata or “bamboo hair.2” Theses abnormalities usually develop during childhood and improve over the years. Other hair findings found include pili torti and trichorrhexis nodosa.1,3
Associated with erythroderma and atopy, hair shaft abnormality comprises the classical triad of manifestations, being the most specific and should always be investigated in erythrodermic children, especially in the eyebrows, where the finding is up to 10 times more frequent.2 Erythroderma may be present in the moment or soon after birth, however, in the majority of patients, ichthyosis gradually appear in areas of polycyclic and migratory erythematous patches with double-edged scales, called ichthyosis linearis circumflexa.1,4
The diagnosis of Netherton Syndrome is difficult, since the family history of the disease may not be present, hypotrichia and stigmas of atopy are found in many erythrodermic newborns with other diseases and not all hair is affected.2
Trichocopy is a non-invasive and rapid diagnostic method that allows the visualization of invaginated areas at various points along the capillary axis, typical of bamboo hair, as well as on a golf tee hair, seen as nodular thickening of the distal end of yarn of hair, corresponding to the breaking of the hair in bamboo at the height of the knot.5,6
In the case reported, the clinical hypothesis of Netherton Syndrome was suspected by clinical history of atopy associated with cutaneous lesions corresponding to ichthyosis linearis circumflexa. Trichoscopy showed trichorrhexis invaginata, confirmed by electron microscopy, proving to be useful as non-invasive evaluations to establish the diagnosis of this syndrome. Histological finding are severe hyper parasqueratosis, with granulosa reduction or absence, acanthosis and papillomatosis. Subcorneal cleavage, spongiosis, exocytosis and Munro microabscesses can be observed.3
It is possible to perform molecular tests (DNA-based) that facilitate prenatal diagnosis in families with known SPINK5 mutations or locus 5q31-32.4 In clinical practice, however, genetic testing becomes infeasible for diagnostic confirmation. The specific finding of trichorrhexis invaginata makes the non-invasive dermatological evaluation through tricoscopy, optical microscopy, electron microscopy or confocal microscopy sufficient to confirm the diagnosis of Netherton syndrome.6,7
Several therapeutic options have been used in the syndrome with variable success and unsatisfactory therapeutic response. Eczematous plaques can be controlled with topical corticosteroids and antihistamines. Systemic and topical retinoids are restricted by the risk of worsening the skin lesion, but there are reports of lesion and hair improvement with low doses of Acitretin 5mg/day or Isotretinoin. Other options include topical calcipotriol, PUVA, Cyclosporine and 12% ammonium lactate.3
Regarding treatment, we avoid the use of topical corticosteroids, due to the extent of cutaneous involvement and the possibility of local and systemic adverse effects. Also due to the extension of the skin disease, the use of topical immunomodulators became infeasible due to the difficulty in evaluating the serum levels of Pimecrolimus or Tacrolimus, necessary to ensure and eliminate its systemic absorption. Phototherapy was not an option because the patient lives away from the referral service. We chose to initiate Isotretinoin at a dose of 0.3mg/kg/day, associated with emollients, based on reports of skin lesion control and improvement of hair with low doses of oral retinoid.3,8 However, the improvement presented was not significant and the oral treatment was discontinued, with only emollients remaining.
None.
The author declares no conflicts of interest.

©2018 Quental, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.