Journal of
eISSN: 2574-9943


Case Report Volume 5 Issue 4
1Department of Dermatology,Venereology and Allergology, Mohammed The VIth University Hospital
2Laboratory of epidemiology, clinical research and public health, Faculty of Medicine and Pharmacy, Mohammed the First University, Morocco
Correspondence: Sara Bouadella, Department of Dermatology, Mohammed The VIth University Hospital, Medical School, Mohammed the First University of Oujda, Morocco, Tel +212 662879202
Received: June 16, 2021 | Published: July 1, 2021
Citation: Bouabdella S, Saddouk H, Zizi N, et al. Grover’s disease: a rare bullous dermatosis spontaneously regressing. J Dermat Cosmetol. 2021;5(4):75-77. DOI: 10.15406/jdc.2021.05.00187
Grover's diseaseis an itchy acantholytic disorder occurring on the trunk of middle-aged men. It is a transient dermatosis of unknown cause manifesting clinically as a papular skin eruption located usually on the anterior chest and abdomen and histologically with dyskeratosis and acantholysis. This disease has occasionally been reported in patients with chronic renal failure, some infections, hematological malignancies, and many other anomalies. We report herein a new case of Grover's disease that developed in a female patient after a fever episode.
Keywords transient acantholys, Grover’s disease, bullous dermatosis
Grover's disease (GD), also known as “transient acantholytic dermatosis,” is an unusual disease that mostly affects middle-aged and elderly men; its etiology is still largely unknown.1 This affection is characterized clinically by pruritus, papulovesicular lesions and small nodules, mainly on the chest, back, lumbar area, and extremities. Herein, we report a new case of Grover’s disease with a brief review.
A 54-year-old female, with past medical history of urinary infection and fever treated with multiple antibiotics, presented with diffuse pruritus and papulovesicular rash on her chest involving since one-month. The patient used topical antibiotics and corticosteroids for her lesions with transient improvements. Clinical evaluation revealed multiple pruritic papules, excoriations, erosions, pustules and crusts with some erythematous plaques localized on the trunk and limbs (Figure 1). We also noted alarge erosive lesion in the axillary, inguinal and sub mammary folds. Dermoscopic examination revealed yellow scales, reddish areas surrounded by a thin whitish halo, pustules and dotted vessels (Figure 2).The patient has not any cutaneous or mucosal involvement. Histopathological examination from a skin biopsy revealed acantholysis, neutrophils and eosinophils cells, subcorneal pustules and intraepidermal detachment (Figure 3). ELISA testing of anti-desmoglein 1 and 3 antibodies were negative. The clinical and histological examinations was compatible with a diagnosis of GD, pemphigus or Hailey-Hailey disease. The clinical evolution and the results of ELISA led to final diagnosis of GD. The patient was treated by topical antibiotics and healing cream with favorable response: regression of the lesions after 2 weeks (Figure 4).
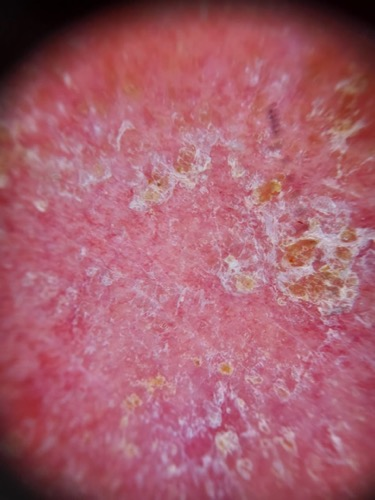
Figure 2 Dermoscopic examination: yellow scales, reddish areassurrounded by a thin whitish halo, pustules and dotted vessls.
GD, also known as persistent or transient acantholytic dermatosis, is a rare condition characterised bypapular, papulovesicular, or papularkeratosic formations that can vary from 1 to 10mm. Vesiculopustular, bullous, follicular, herpetiformis, and erythematous forms have already been described.1,2 The most common locations of eruptions are the chest and root of members, while scalp, face, and neck are less affected. In an exacerbation, the erythematous papules may converge, forming erythematous plaques as it is the case of our patient. The itching is a frequent complaint, and its intensity is variable. The age group most affected by GD includes individuals over the fifth decade in age, with predominance of the Caucasian ethnicity, and with a men to women ratio of 3:1.2 The etiology of GD is still unclear, but many factors have been associated with the development of the disease.1 Fever or prolonged bed rest, sweating or excessive heat, exposure to UV radiation, treatment with ionizing radiations, xerosis and some drugs have been associated with this disease.3 This affection is due to sweat ducts obstruction and from the leakage of products that induce acantholysis. However, the possibility still exists that smaller molecules may seep through the ductal epithelium and cause epidermal acantholysis. In addition, heat may directly cause acantholysis through the release of an unknown enzymatic factor after mild thermal injury.1 Infections (Malassezia furfur or Demodexfolliculorum) and severe dermatosis (atopic dermatitis, allergic contact dermatitis, and asteatotic eczema) are also associated with GD.4 GD has been reported in patients with renal failure, immunodeficiency conditions, including HIV infection, haematologic malignancies, and solid carcinomas. Also, the onset of GD after, kidney, liver heart and bone marrow transplantation has been described.4 The GD is an under-diagnosed disease, probably due to the large number of oligosymptomatic cases and/or transient or due to the fact that the disease clinically co-exists or is confused with other illnesses making diagnosis difficult.2 The clinical differential diagnosis of Grover’s disease includes a variety of skin disorders such as pemphigus foliaceus, pemphigus vulgaris, impetigo, dermatitis herpetiformis, Hailey-Hailey disease and Darier’s disease. Four histological patterns have been identified: Darier type, Haley–Haley type, pemphigus and spongiotic type.5 In the case of our patient, the biopsy and histopathological examination of two skin segments showed findings compatible with pemphigus like forms, and Hailey-Hailey-simile.2 Histopathology examination represents the gold standard for the diagnosis. In the Darier-like variety, which represents the most frequent pattern seen in Grover’s disease. The histopathological aspect is similar to Darier’s disease, consisting of acantholysis mainly involving suprabasal layers, dyskeratosis (with presence of grains and corps ronds), hyperkeratosis, acanthosis, and parakeratosis.5 Dermoscopic examination of Grover’s disease has been described showing polygonal, star-like shaped yellowish/brownish areas that histopathologically correspond to marked hyperparakeratosis and acanthosis, and a peripheral whitish halo that correlates with orthokeratosis and hypergranulosis.5 Although GD is generally self-limited and resolves within weeks or months even in immunocompromised patients, in some cases it may persist or recur.1 Measures to prevent excessive sweating should be introduced early such as avoiding exposure to the sun, heat, and intense physical activity. It is important, also, to minimize skin irritation by using mild soaps, light-colored cotton fabrics, and adequate hydration.2 Topical therapy consists of steroids, tretinoin, and calcipotriol. Systemic therapy includes oral vitamine A, corticosteroids and lactic acid.1 Systemic therapy is recommended in the most extensive and persistent lesions. The literature describes the use of retinoids and methotrexate besides steroids for the remission of lesions. Some studies show that the use of phototherapy with psoralen and ultraviolet A may be a useful resource.2
GD is a transient acantholytic dermatosis. Its etiology is unknown. It is an under-diagnosed disease because it’s clinically and histologically indistinguishable from pemphigus, Darier's disease and Hailey-Hailey disease.
The authors declare no conflict of interest.
None.
None.

©2021 Bouabdella, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.