Journal of
eISSN: 2574-9943


Research Article Volume 7 Issue 3
Faculdade de Medicina do ABC
Correspondence: Luciana Cirillo Maluf Azevedo, Faculdade de Medicina do ABC, Address Rua Dardanelos, 411 apt 121 - Alto da Lapa, São Paulo, Brazil 05468-010, Tel +55 11 99274-1841
Received: August 02, 2023 | Published: August 14, 2023
Citation: Azevedo LCM, Valim CS, Pardi BJ. Finding the main facial aging vector force to reverse the impact of soft tissues and weak ligaments to the original youthful face. J Dermat Cosmetol. 2023;7(3):85-89. DOI: 10.15406/jdc.2023.07.00242
Background: In order to reverse a flabby face, we need to be aware of where the main vectorial aging face force, which is the sum of the descendent forces like gravity, attenuated ligaments and facial fat deflation, is placed. Main soft tissues promote medial inferior deflation and fat compartment shape changes.
Aims: We propose a new method to find the angle of the main vectorial facial aging without the need to visualize the zygomaticus major muscle directly, but instead by doing a finger test by pulling the skin upwards and laterally with the patient’s head in the upright position.
Patients/ Methods: We collected facial measures from 73 female subjects within the Brazilian population, aged between 30 to 69 years old. Then, the main aging vector angle was measured on each participant sitting in the upright position guided by a standardized protocol.
Results: The median aging vector angle was made and the patients were divided into age-groups from 30 to 39 years old (52.5o), from 40 to 49 (51o); 50 to 59 (55o) and 60 to 69 (51o).
Conclusions: According to our study and statistical analysis we could find the main facial aging vector angle between 30 and 69 years old didn’t vary significantly and was around 51°to 55°. Our aim was to propose guidance to a better natural surgical or nonsurgical lifting strategy that focuses on the reversal of flabby tissues (inferomedially) by counteracting the main facial aging vector force toward the superior-lateral facial area.
Keywords: vector, ligaments, facial aging, soft-tissue descent, volume loss, supine position
According to mathematical and physical rules and in order to reverse a flabby face, we need to be aware of where the main vectorial aging face force - which is the sum of the descendent forces like gravity, attenuated ligaments and facial fat deflation1 is placed. Based on Newton’s third law of motion of classical mechanics that states that every action is accompanied by a reaction of an equal magnitude but opposite direction, such deflation forces are represented by vectorial forces.2 Vectors are used to represent any quantity that has direction and magnitude. Gravity induces a soft tissue downward force and, as we age, the attenuation of the ligaments exerts a vector medially and downwards. One of the basic vectorial properties is the rule of vector addition. The sum of these two vectors results in a main diagonal downward and medially force by using the triangular rule or the parallelogram rule1 (Figure 1). Then, such vectorial force needs to be counteracted by an opposite one (an upward and lateral vector – towards the upper part of the helix) due to the reposition of the soft tis-sues descent1 (Figure 2).
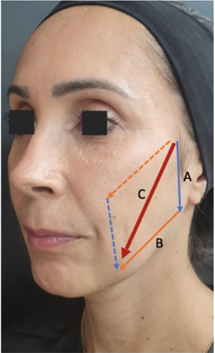
Figure 1 Triangular rule or the parallelogram rule: A) Gravity force vector; B) Flattened retained ligaments and fat pads force vector: C) The sum of the facial ageing vector.
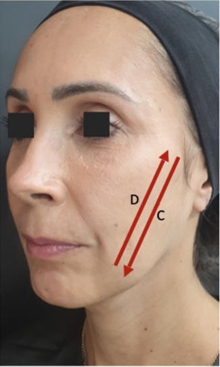
Figure 2 By Newton’s third law, vector D equal to vector C both in force and magnitude, but in the opposite direction. Vector D may guide the lifting procedures.
After reviewing PubMed literature, we can see how the main soft tissues promote medial inferior deflation and fat compartment shape changes. Besides, we propose a new method to find the angle of the main vectorial facial aging without the need to visualize the zygomaticus major muscle directly (by cutting the layers on top of it), but instead by doing a finger test slightly and gently pulling the skin and soft tissues upwards and laterally with the patient’s head in the upright position. In addition, the Body Mass Index (BMI) was collected and analyzed for statistically significant changes.
This is a prospective, transversal, comparative study made in São Paulo/ Brazil, from July 2022 to August 2022. The study was approved by the Research Ethics Committee (REC) before participants were enrolled. Informed consent was obtained for each participant in accordance with the REC protocol. Three board certified dermatologists were trained with the same mathematical instruments (a goniometer, a protractor and a cosmetic white pencil) and the same face drawing process. We collected random data from 73 female subjects within the mixed Brazilian population, with or without facial sagginess and aged between 30 to 69 years old. Age was divided into four age groups: 30-39; 40-49; 50-59 and 60-69.
Subjects were excluded in case of having undergone any cosmetic procedures on the face over the last 12 months, having scars or infections on the target site, significant facial asymmetry, autoimmune diseases or pregnancy. Then, the main aging vector angle was measured on each participant sitting in the upright position.
According to our following protocol (Figure 3A and 3B) & Figure 4 (4.A to 4.J):
Based on volunteer’s demographic data age-groups, weight, BMI and nutritional status were measured. (Table 1)
|
Variables |
Descriptive measures |
|
Age, years |
(N=73) |
|
Median (standard deviation) |
49,8 (10,5) |
|
Minimum – maximum |
30 – 69 |
|
Age range |
(N=73) |
|
30 a 39 years old |
14 (19, 2%) |
|
40 a 49 years old |
20 (27, 4%) |
|
50 a 59 years old |
21 (28, 8%) |
|
60 a 69 years old |
18 (24, 6%) |
|
Weight, Kg |
(N=64) |
|
Median (standard deviation) |
71,5 (12,2) |
|
Mínimo – máximo |
50 – 126 |
|
BMI, Kg/m2 |
(N=64) |
|
Median (standard deviation) |
27,9 (4,2) |
|
Minimum – maximum |
20,1 – 41,1 |
|
Nutritional status |
(N=64) |
|
Eutrophy |
17 (26, 6%) |
|
Overweight |
29 (45, 3%) |
|
Obesity |
18 (28, 1%) |
Table 1 Demographic data about patients
According to the age-groups, the median aging vector angle was made in the upright position and the patients were divided into age-groups from 30 to 39 years old (52.5o), from 40 to 49 (51o); 50 to 59 (55o) and 60 to 69 (51o). The median mandibular angle remains at 120° as they aged. And the median distance between PX (the mandible line A and the mandible ligament crossing point) and P2 was 2.0 cm.
According to BMI and nutritional status, the median aging vector angle was 52°, the median mandibular angle remains at 120° and the median distance between PX and P2 was 2.0cm. BMI and to the nutritional status did not show significative variations for those angles.
The sagginess and laxity of skin aging are partially due to the flatness of the retaining ligaments that secure facial tissues into the anatomic position of youth.1,3 The fibrous septa which divide the face into fat compartments are made of retaining ligaments and their ramifications to the surface.4,5 As we age, bone alterations end up promoting changes in the adhesion points of the ligaments and condensations of the face. This leads to a change in the path of these ligaments, which probably promotes the lengthen septa and the fibers bend in its own course, and the fall of the compartments of the fat pads.6,7 In addition, there are two types of SMAS to be known: preparotideal SMAS which interconnects fibrous chambers enfolding fat tissue compartments that amortizes the space between the skin and mimic muscles. Fibrous septa sectorizes the mimic muscles surrounding the muscular bundles. Above the mimic muscular plane, SMAS septa go up into the skin, by passing through the subcutaneous fat layer with several irregularly arranged collagen fibers. The other type, parotideal SMAS, has its fibrous septa arranged parallel to the skin level, docking the cutaneous layer to the parotid fibrous fascia. This SMAS envelops the fat tissue pads.8
In this context, some important anatomic knowledge is critical: zygomatic cutaneous ligament (ZCL), masseteric cutaneous ligament (MCL), orbital retaining ligament (ORT), nasolabial fold (NLF) and facial jowl.1
The ZCL supports gravitational changes3,9 and sustains the malar soft tissue over the zygomatic eminence.1 As this ligament weakens with age, it is unable to preserve soft tissues in the original youthful position.10,11,12 As a result, facial fat pads flatten and plump in a layer between the superficial and deep facial fascia.4,11,12 In addition, as the ZCL support fades progressively, the NLF deepens.1
The MCL sustains the cheek above the mandibular line. The bended MCL results in downward and medial deflation of the lower facial fat pads crossing below the mandibular border. The counteracting vector points upwards and laterally towards the root of the helix by pulling this skin area, thus, improving jawline definition and facial jowl.1 Loss of ORT support permits anatomical facial changes which worsen the inferomedial tissue sagginess and the loss of the youthful facial contours.1 By mobilizing the preauricular skin region and the lateral cheek malar area, the counteracting vector force should be pointed in a superolateral direction to smoothen the mid-facial tissues and thereafter soften the NLF prominence.1
Other studies support that facial fat roll and inferior descent serve as key factors for determining a square aged facial shape.7,9 Although rhitidectomy needs to identify the zygomaticus major muscle orientation to lift the SMAS, it varies significantly as we age depending on bony changes and soft tissue descent.13
Jacono et al.,13 described its muscle angle was measured in relation to the Frankfort horizontal plane with the patient in supine position during the surgeries.13 Moreover, Mally et al.,14 showed that when subjects were altered from upright to supine position, many anatomic parameters - such as nasolabial folds, cheeck volume, malar bags/festoons, etc - smoothen and the facial appearance became younger, therefore concluding that gravity plays the major role in facial aging.14 And, interestingly, Jacono et al.,13 found the maximal rejuvenation angle average between age groups during rhytidectomies and showed it was more superior than posterior in all cases.15
This vectorial facial lifting method above the SMAS will provide physicians another way to clinically find the principal anti-aging vector force to man-age surgical or nonsurgical facial aesthetic procedures (threads, fillers, biostim-ulators, etc) aiming for natural rejuvenation and the restoration of youthful face contours. (Figure 1 & Figures 2)
Usually, patients who request a face lift would like to correct sagging jowls, deep NLF, prominent neck bands and double chins.16
In this study, we could find the median facial aging angle between different age-groups by math and physics principles, although there are significant biological factors and particular characteristics of each ethnicity17,18 that play a role. In our research the angle behaviour between 30 and 69 years old didn’t vary significantly and was around 51°to 55°. The median aging angle in the 50-59 year old group was somewhat unexpected. Maybe it´s because as they are independent outcomes, the end result may vary since the data was collected in different locations - despite the masks having been done using the same procedure. Another point to note is that all subjects were female since males were more reluctant to allow the drawing process on their faces.
Contrary to our expectations, based on BMI and nutritional status the outcomes didn´t show significant angle variations. It might probably be because of the small number of subjects in each age-group for the stratification between eutrophic, overweight and obese.
According to Avelar et al.,16 as we age we have changes all over the facial layers. The mandible bone angle becomes more obtuse throughout the years and the facial remodeling depends fully on growth, development and overlying soft tissue functions. Moreover, one of the factors that leads to soft tissue excess and sagging is the mandible volume loss over the years.19 In our study, the mandible angle didn’t change significantly. It could be because the measurement was done on top of all the facial layers in this area and perhaps the goniometer (a mathematical instrument) couldn’t find a precise angulation due to all skin layers above the mandible bone.
Facial aging refers to complex additive and subtractive modifications acting on a three-dimensional geometric entanglement.1 There are many factors to be considered – flatten fat pads, the loss of the support ligaments, gravitational descent, skin quality, laxity, volume restoration, repeat shearing forces1 but the main facial vector aging force in each individual skull should be a significant tool. Because of all these variants, we suggest that the procedures should be customized to the individual patient, as supported by other studies.13,20
Considering the movement and the modification of all soft tissues on the aging face and despite the number of subjects, our aim was to propose a better natural surgical or nonsurgical lifting strategy that focuses on the reversal of flabby tissues (inferomedially) by counteracting the main facial aging vector force toward the superior-lateral facial area - which is considered the fixed part of the face compared to the mobile anterior part.1
In order to give more relevant math and physics statistical data, our study could be considered one more tool to give consistent measures of a strip vectorial facial angles finding the main facial anti-aging vector force into the age-groups (including the anatomy and all the changes in the layers) to better restore youthful facial natural lifting and contours.
None.
Authors declare there is no conflict of interest.

©2023 Azevedo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.