Journal of
eISSN: 2574-9943


Case Report Volume 2 Issue 1
1Physiotherapist, Professor in Pontifícia Universidade Católica de Minas Gerais, Brazil
2Master student, Bioengineering in Universidade Federal de Minas Gerais, Brazil
3Nutritionist, PhD in Food Science, Brazil
3Specialist in Dermatofunctional Physiotherapy, Brazil
Correspondence: Angélica R Araújo, Physiotherapist, PhD in bioengineering, Professor in Pontifícia Universidade Católica de Minas Gerais, Brazil
Received: February 10, 2018 | Published: February 20, 2018
Citation: Araújo AR, Moreira NV, Parreiras PR, et al. Effectiveness of ultra cavitation in reducing abdominal fat: a case study. J Dermat Cosmetol. 2018;2(1):76-81. DOI: 10.15406/jdc.2018.02.00046
Introduction: The localized abdominal adiposity is the accumulation of fat in the abdominal region. This fact contributes so that the loss of measurements in the abdominal region does not always happen in a satisfactory way, compromising both the health and the esthetics of the individual. This, together with the current appreciation of low levels of body fat, leads people to dissatisfaction with their body's appearance and low self-esteem.
Objective: To evaluate the effects of high intensity ultrasound (ultracavitation) on the reduction of abdominal adiposity in humans.
Method: Case study, performed in a 22-year-old female, with a diagnosis of abdominal adiposity. An ultrasound examination of the bilateral abdominal wall was performed before and after treatment with ultracavitation to evaluate the efficacy of the procedure. The treatment was performed only in the left hemi abdomen; the right hemi abdomen was used for control. Three ultracavitation sessions were performed at a frequency of once per week. The parameters used were: continuous mode ultrasound, 30Watts intensity, for 85 minutes per session, in an area of 100cm2. Before and after each session we performed plicometry of the skin folds in the abdominal and suprailiac regions and also the perimetry of the abdominal circumference and the right and left hemi abdomen. For the study, the volunteer also did an alimentary record and answered the International Questionnaire on Physical Activity (version 6). Results: According to ultrasonography of the abdominal wall, there was a reduction of 9.5% in the thickness of the treated nodulated hypodermic layer and 8.1% of the untreated side. Regarding the plicometry, there was a mean reduction in skin fold size of 15.7% on the treated side and 6.8% on the untreated side. In the abdominal circumference, there was a mean decrease of 3.7% in the total circumference; of 1.4% in the circumference of the left hemi abdomen (treated side) and 1.9% on the right side (control).
Conclusion: High-intensity ultrasound has been shown to be effective in reducing abdominal adiposity in the treated subject. The effects of ultracavitation on the reduction of abdominal circumference, cutaneous pleural size and thickness of the hypodermic layer were satisfactory, and this feature may be an important adjunct in the treatment of abdominal adiposity.
Keywords: cavitation, abdominal adiposity, ultrasound therapy, liposuction, physical activity questionnaire
Obesity is defined as a generalized increase in body fat due to a positive energy balance in which caloric intake exceeds energy expenditure1 and is one of the biggest public health problems in the world. According to the Brazilian Institute of Geography and Statistics (IBGE), 56.9% of the Brazilian population (most of them women, 58.2%) is overweight and, among them, 21.5% are obese individuals.2 Overweight is a risk factor for cardiovascular diseases, diabetes, dyslipidemia and metabolic syndrome.3–5
Currently, it is demonstrated that not only total fat deposition of the body, but also fat distribution exerts an important influence on the levels of risks posed by obesity.6 According to McArdle et al.,7 obesity may present as type 1, in which there is an excess of fat located proportionally throughout the body; type 2, where the excess localized fat occurs essentially in the subcutaneous region of the trunk; type 3, where localized excess fat essentially occurs in the subcutaneous region of the lower body and type 4, where there is excess fat located essentially in the intra-abdominal region.7
The localized abdominal adiposity is the accumulation of fat in the abdominal region.3 The fat cells located in this region have the slowest metabolism and, because of this, are more resistant to weight loss.8 This fact contributes so that the loss of measurements in the abdominal region does not always happen in a satisfactory way, compromising both the health and the esthetics of the individual. This, together with the current appreciation of low levels of body fat, leads people to dissatisfaction with their body's appearance and low self-esteem.1
In order to improve body appearance, there is a wide range of procedures that are available to sculpt the body, including the traditional diet2 and surgical interventions (liposuction, abdominoplasty and bariatric surgery).9 The latter, although producing good results in relation to the improvement of the corporal aesthetic, has as disadvantages the intercurrences, as for example: nutritional implications due to the bariatric surgery;9 lymphoedema, which can progress to fibro sclerosis and alter tissue mobility and body contour;10 and the presence of hematomas and seromas in the abdominoplasty.11
Currently, the physiotherapy has several treatments, such as manual massage,12 radiofrequency,13 carboxytherapy14 and ultrasound high (ultracavitation) and low-intensity8,15 to aid in the treatment of body fat.
The selective effects of ultracavitation in the human body16,17 are responsible for highlighting this modality of treatment that, according to some authors, is able to safely remove and remodel deposits of abdominal subcutaneous adipose tissue, which is the most commonly used method for detecting adipose tissue. However, the literature is still controversial on this issue.
Despite the increasing clinical use of ultracavitation in esthetics, there are few studies on the subject, most of them being performed on animals. In view of this, this study aimed to evaluate the effects of high intensity US (ultracavitation) on the reduction of abdominal adiposity in humans. We specifically sought to analyze the effects of high-intensity US on the reduction of abdominal circumference, skin fold size (suprailiac and abdominal), and thickness of the hypodermic layer.
This is a case study, performed in a 22-year-old female, 1.64m tall, with a diagnosis of abdominal adiposity. The volunteer was recruited at the Minas Day Spa clinic, located in the city of Belo Horizonte/MG, where the data collection was conducted. A blood test was previously requested from the volunteer in order to confirm the absence of pregnancy and hypercholesterolemia, situations that would indicate the accomplishment of the treatment with high intensity US.
The procedures to be performed in the research were previously clarified to the volunteer, who signed the Term of Free and Informed Consent, giving their consent to participate in the study. After the term was signed, it was submitted to a physical therapy evaluation, which consisted of anamnesis, collection of anthropometric data (body mass, waist-hip ratio (WHR) and body mass index (BMI)) and guidelines for the need of performing a food and physical activity record.
The food registry was performed for 5 weeks (3 records per week, totaling 15 records), with the first 6 records being taken two weeks before the start of treatment and the remaining ones during the intervention period. Information was collected regarding the time and type of food eaten throughout the day. This information was used to evaluate the volunteer's dietary pattern in the weeks prior to the study and during the study.
In order to record physical activity, the International Physical Activity Questionnaire-version 618 (Appendix) was used, applied to each week of treatment. The information related to the food registry and the International Physical Activity Questionnaire provided subsidies to evaluate the impact of feeding and physical activity factors on the study results.
Intervention
The volunteer underwent ultracavitation treatment using the Liposonic® device of the Meditea brand (Buenos Aires, Argentina). Three ultracavitation sessions were performed, one per week, with the following parameters: intensity 30Watts and 100% emission. The procedure was performed for 85minutes in the left abdomen (treated side), in a rectangular area of 100cm2. The area was obtained starting from the umbilical scar as the starting point, from which a 5cm long straight line was drawn in the caudal direction, and from this point another straight line was drawn with a 20cm extension in the left lateral direction, forming a rectangle. The right hemi abdomen (untreated side) was used as control.
Outcomes
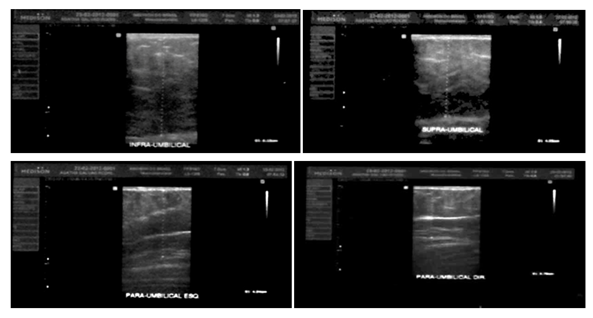
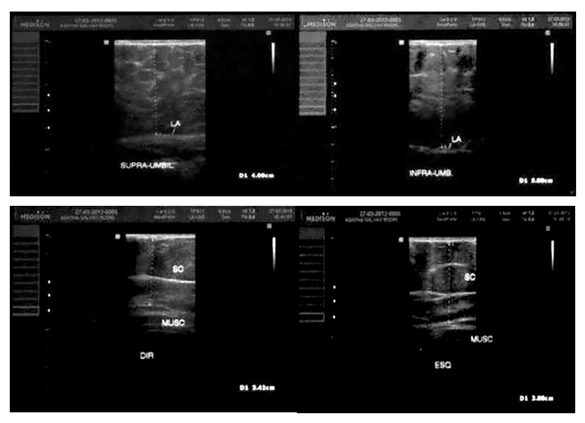
Thickness of the hypodermic layer: the thickness of the hypodermic layer of the abdominal region was determined by ultrasound examination of the abdominal wall, performed separately in the right and left abdomen. The examination was performed by a radiologist, the day before the start of treatment (pre-treatment) and the first day immediately after the last session of the study.
Skin fold: the skin folds of the abdominal and suprailiac regions were measured using an adipometer (Innovare from the Cescorf brand-Porto Alegre, Brazil). The measurements were performed in the right and left hemi abdomen at the beginning and end of each study session, always by the same evaluator. For each fold, three measurements and the arithmetic mean considered for the analysis were made.
Abdominal circumference: Measurement of abdominal circumference (abdominal perimetry) was performed using a tape measure. Two measures were taken: one considering the umbilical scar as a reference point and another whose reference was a point located 4cm below the umbilical scar. At each reference point, the total circumference of the abdomen (total abdominal perimetry) and the circumference of the hemi abdomen (region between the umbilical scar and the spinal process L1 of the spine) on the right and left sides (perimetrial partial abdominal and left partial abdominal perimetrial, respectively) measured. Measurements were performed at each treatment session, immediately before and after the intervention. In each measurement were made 3 measures and the average considered for the analysis.
For the characterization of the sample, a descriptive analysis of the collected variables was performed, with measures of central tendency and variability of the beginning and the end of treatment for each of the evaluated outcomes.
The data presented in Table 1 refer to the initial and final anthropometric characteristics of the study participant. It is possible to observe that the volunteer presented a gain of body mass of 2kg, passing from the first to the second degree of obesity. The WHR presented by the volunteer both at the beginning and at the end of the study was high (ideal WHR for women is less than 0.7).
Anthropometric data |
Initial |
Final |
Body Mass |
93.4kg |
95.6kg |
Height |
1,65m |
1,65m |
BMI |
34.7kg/cm2 |
35.3kg / cm2 |
RCQ |
0.805 |
0.813 |
Table 1 Anthropometric characteristics of the participant at the beginning and at the end of the study
The volunteer maintained the same level of physical activity during the treatment, showing her sedentary profile, as identified by the International Questionnaire of Physical Activity. In the nutritional analysis of the food registry, no qualitative changes were observed in the diet of the volunteer before and during the study.
Table 2 shows the results of abdominal ultrasonography performed before and after the three ultracavitation sessions. It is possible to observe that in the region evaluated in the left abdomen (treated area) there was a reduction of 9.5% in the thickness of the hypodermic layer and in the right hemi abdomen (control area), the reduction of hypodermic layer thickness was 8.1% (Figure 1) (Figure 2).
Hemi-abdomen circumference |
Initial value |
Final value |
Percentage reduction |
Infra umbilical |
6,1cm |
5,8cm |
4,9% |
Left umbilical |
4.2cm |
3.8cm |
9.50% |
Right umbilical |
3,7cm |
3,4cm |
8,1% |
Table 2 Results of abdominal ultrasound examinations performed before and after three ultracavitation sessions
The values of the skin folds of the right and left abdominal and suprailiac regions in the 1st, 2nd and 3rd treatment sessions with the high intensity US and the reduction percentage at the end of the three treatment sessions can be visualized in Table 3. It is possible to observe that, except for the right abdominal region, there was reduction in the values of the folds in all the regions. However, the percentage of reduction in skin fold values was higher on the side where the intervention was performed (left abdominal region=10%, left suprailiac region=21.4%).
Hemi-abdomen circumference |
1st session |
2nd session |
3rd session |
% reduction |
|||
Skin folds |
Initial value |
Final value |
Initial value |
Final value |
Initial value |
Final value |
|
Abdominal left |
30±0,5* |
25±0 |
26±2,64 |
25±2 |
27±1 |
27±2 |
10% |
Suprailiac left |
28±2* |
27±3,6 |
26±1,8 |
23±2 |
25±2,64 |
22±1,73 |
21,4% |
Abdominal right |
30±1* |
30±3,6 |
29±1,73 |
29±2,64 |
30±2,64 |
30±2,64 |
0% |
Suprailiac right |
22±3* |
22±2,64 |
24±0 |
24±1,32 |
25±0 |
25±1 |
+13,6% |
Table 3 Skin fold values of the abdominal and suprailiac regions in the 1st, 2nd and 3rd treatment sessions with high intensity ultrasound
* Mean±standard deviation.
Table 4 shows the results of abdominal circumference measurements obtained before and after each session with high intensity ultrasound. It is possible to observe that there was a reduction in the values of the circumferences after the treatment.
Hemi-abdomen circumference |
1st Session |
2nd Session |
3rd Session |
% Reduction |
|||
Abdominal circumference |
Initial value |
Final value |
Initial value |
Final value |
Initial value |
Final value |
|
Umbilical scar |
108±4,6* |
105,5±0,5 |
106±1,3 |
104,5±2,8 |
106±2,6 |
103,5±1,4 |
4% |
4cm below umbilical scar |
116,5±2* |
115,5±2,2 |
115±1,7 |
114,5 ±1 |
114±1 |
112,5±2,2 |
3,4% |
Table 4 Total abdominal circumference values in the 1st, 2nd and 3rd treatment sessions with ultracavitation
* Mean± standard deviation.
The left and right hemi abdomen circumferences in the 1st, 2nd and 3rd treatment sessions with the high intensity US and the reduction percentage at the end of the three treatment sessions can be visualized in Table 5. It can be noted that in all regions (except in the region "4cm below the left navel") the hemi abdomen circumference values decreased, with the highest reduction percentage (2.9%) occurring in the circumference of the hemi abdomen measured from the left umbilical scar.
Hemi-abdomen circumference |
1st session |
2nd session |
3rd session |
% reduction |
|||
Initial value |
Final value |
Initial value |
Final value |
Initial value |
Final value |
||
Left umbilical scar |
52±0* |
51±1,5 |
49±1,7 |
48±0,9 |
52±0,5 |
50,5±0 |
2,9% |
4 cm below belly button |
55,5±1,3* |
55±1,7 |
56,5±0 |
55±0,64 |
57±1 |
55,5±1,8 |
0% |
Right umbilical scar |
51±1* |
51±0,5 |
51±2,6 |
51±0 |
50±2,6 |
50±2,6 |
1,9% |
4cm below navel right |
56±2* |
56±1 |
55±1 |
55±2,6 |
55±0,9 |
55±1,7 |
1,8% |
Table 5 Circumferences of left and right hemi abdomen before and after each session of high intensity ultrasound treatment
*Mean±standard deviation.
The device that contains the kinetic or mechanical oscillations produced by a vibrating transducer that is applied to the skin for therapeutic purposes, crossing it and penetrating the organism at different depths is denominated US,19,20 which provides a safe way to remove and remodel unwanted abdominal subcutaneous adipose tissue deposits.20
There are two mechanisms that result in the extraction of adipose tissue through the use of the US. The first is through the conversion of mechanical energy into heat and the second through cavitation.21 Cavitation can be of two types: stable and transient (better known as ultracavitation).21 In stable cavitation there is a cellular necrosis that is induced by a combination of mechanical stresses and thermal injury that causes tissue vibration.22 The molecular structure is subjected to compression and rarefaction alternately.21 During rarefaction the gases absorbed in the liquids around the cavity or in the interface evaporate, resulting in cavity expansion.19 In this process bubbles are formed and oscillate in size or collapse rapidly.21,23
In transient cavitation or ultracavitation, using a certain frequency of vibration with a certain power24 the resonance of the molecules of a specific structure occurs,21 generating micro bubbles that collapse and implode. In this study, we evaluated the relationship between the structure of the structure and the structure of the structure. In ultracavitation, the wave vibrates at the same frequency as the adipocyte membrane, thus breaking this cell.19
In this study, treatment with ultracavitation resulted in a greater decrease of subcutaneous fat in the left peri-umbilical region and also a greater reduction in the value of the skin folds on the treated side. As far as the circumference of the hemi abdomen in the region of the left umbilical scar, there was also a greater decrease in the treated side. Similar results to those observed in the present study have also been reported by other authors.25–27
Fatemi25 carried out a study with the objective of verifying the effectiveness of the Liposonix device in the reduction of localized fat. The author used the device in the abdomen, waist and hip regions. However, he did not mention the number of sessions performed. The equipment was applied for 45-60minutes, with a dose of 140J/cm2. The evaluation of the efficacy of high intensity US was made by comparing the variable abdominal circumference. The authors observed that after the treatment there was an average reduction of 4.7cm in the treated areas.
The study by Teitelbaum et al.26 aimed to evaluate the efficacy and safety of the Contour I TM (high intensity US) device in the abdominal, waist or flank regions. It was observed that after the treatment there was a mean decrease of the circumference of 1.9cm in the areas mentioned above. However, the authors do not cite the parameters used for treatment.
Moreno-Moraga et al.27 also performed a study with the Contour ITM with the same objectives of the study of Teitelbaum et al.26 The authors used the device in several unspecified areas, performing 3 sessions. The equipment was used with the parameters: frequency of 200±30kHz and intensity of 17.5W/cm2. After treatment, there was a mean reduction of 3.9cm in the circumference of the treated regions.28–30
The results found in the literature and those observed in the present study suggest that high intensity US is an effective therapeutic resource in reducing abdominal adiposity.
High-intensity US showed to be effective in reducing abdominal adiposity in the subject treated in this study. The effects of ultracavitation on the reduction of waist circumference were relatively satisfactory, as well as on the reduction of the value of the skin folds and the thickness of the hypodermic layer.
None.
The author declares no conflicts of interest.

©2018 Araújo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.