Journal of
eISSN: 2574-9943


Research Article Volume 4 Issue 5
Department of Dermatology, Venereology & Leprosy, Hassan Institute of Medical Sciences, India
Correspondence: Deepak Jadhav,Department of Dermatology, Venereology & Leprosy, Hassan Institute of Medical Sciences, India
Received: September 21, 2020 | Published: October 29, 2020
Citation: Ittigi V, Jadhav D. Comparative study of fractional Co2 laser with salicylic–mandelic acid peel v/s dermaroller with salicylic–mandelic acid peel for treatment of post acne atrophic scars. J Dermat Cosmetol. 2020;4(5):139-143. DOI: 10.15406/jdc.2020.04.00165
Introduction: Scarring in acne is a major concern cosmetically disfiguring the face , so treatment of acne scar is challenging.
Methodology: Aims and Objectives: 1. To compare the effectiveness of fractional Co2 laser with salicylic mandelic acid (SM) peel versus Dermaroller with salicylic mandelic acid (SM) peel in treatment of post acne atrophic scars. 2. To evaluate complications and demographic details.
Method: 30 patients were recruited and randomly divided into 2 groups. Each group contains 15 patients. In GROUP 1: fractional Co2 laser (Fr.Co2) done followed by SM peel 15 days later for 6 settings each. GROUP 2: Microneedling with dermaroller followed by SM peel 15 days laterfor 6 settings each. Photographs were taken pretreatment & at each visit and the improvement was graded using global assessment score by both treating physician and the patient. Results were evaluated and statistical analysis done using SPSS version 20.
Results: On comparison, both the groups showed improvement in scars, but the percentage of scar grade improvement was more in group B (38.89%) than group A (33.89%).
Conclusion: This study concludes both treatment modalities are effective but more scar grade improvement was seen with DERMAROLLER+SMP (38.89%) than FCO2+SMP (33.89%) and shows a future treatment for acne scar patients.
Acne is a very common problem affecting more than 90% of adolescent population, and it continues into adulthood in 12–14% of cases. Acne scarring is permanent disfiguring sequel which can take varied morphological forms. Many therapeutic approaches have been used to treat acne scarring (invasive & noninvasive methods), but even with the most expensive techniques it is difficult to achieve the goal of complete improvement. Thus, there is an ever increasing demand of less invasive, highly effective and affordable therapeutic procedures to treat acne scars.
To compare the effectiveness of fractional Co2 laser with salicylic-mandelic acid peel (SMP) versus Dermaroller with salicylic-mandelic acid peel (SMP) in treatment of post acne atrophic scars. To evaluate complications and demographic details.
A comparative prospective study was conducted on 30 patients with post acne atrophic scars, attending our outpatient department. Duration of the study was for 8 months, conducted from September 2017 to April 2018.
Inclusion criteria
Patients with acne scars.(Goodman and Baron Grade II, III, IV atrophic acne scars). Patients above 18yrs and Patients willing for procedure.
Exclusion criteria
Patients with active acne. Predisposition to keloid formation, history of bleeding disorder and anticoagulant therapy and oral steroid therapy. Patients with HIV, HBV infections. Active skin infection like warts, herpes. Pregnancy and lactation and Photosensitivity should be excluded from the study.
First the patient was explained about the procedure, duration of the treatment, side effects, prognosis of treatment and consent was taken. Then the patient was thoroughly evaluated by objective and subjective parameters were estimated at baseline and at the end of 6 months using Goodman’s qualitative global acne scarring grading system and 5 point visual analog scale. Out of 30 patients, randomly divided into 2 groups. Each group contains 15 patients.
In GROUP A: Fr.Co2 laser done followed by SMP after 15 days for 6 sittings each.
GROUP B: Microneedling with dermaroller followed by SMP after 15 days for 6 sittings each. A total of 6 sessions done at an interval of 4 weeks each.
Preparations prior to procedure
Common for both groups –Digital photographs of were taken before and after procedure. Treatment area is gently cleansed and a topical anaesthetic cream (mixture of lidocaine and prilocaine) is applied for 45 minutes and washed off with sterile water. General protective measures for eyes were taken.
Group A- Patients are treated with a single pass of fractional CO2 laser.
FCO2 laser specifications
Power: 15W ( Energy 45mj), Duration: 3.0ms, Interval: 3.0ms and Scan mode: Normal
Pre and post cooling with ice cubes was done to prevent post procedure burning and pigmentation. After 14 days patient is treated with SMP (after test peel). Standard pre peels procedure is followed. Patients experienced a stinging sensation that lasted for 3 to 5 minutes. After the cessation of this stinging sensation, most patients developed a uniform white crystalline precipitate, ‘‘pseudofrost,’’ in the peeled areas. After peels all patients were instructed to wear sunscreen and to avoid sun exposure.
Group B-Microneedles with 1.5mm length and 192 needles on roller drum is used. Pre procedure preparations is followed as mentioned earlier. The skin is stretched and microneedling is carried out in vertical, horizontal and both diagonal directions for about 4-5 times till pin point bleeding occurs from the site and this will be considered as end point of treatment. The treated area is cleaned with sterile gauze soaked with normal saline. Ice packs applied over the treated areas. Post procedure, topical antibiotic medication for 2-3days, sun protection and regular usage of sunscreens is advised. The patients are reviewed after 1 week for any side effects. After 14 days of dermaroller treatment, patient are treated with SMP. After peels patients are instructed to wear sunscreen and to avoid sun exposure. (Figure 1-5)
A total of 30 patients of acne scars were enrolled in the study. In both groups–majority (73.3%) between ages of 20-25 years. Both groups- 8 (53%) patients males & 7 (47%) patients females. Majority of patients were Students in group 1 (60%); in group 2, (46.7%) & employee (40%). In Group A-66.7% and in Group B- 80.0% were graduates. Fitzpatrics Skin Type was Type 4 and 5 in all the patients.
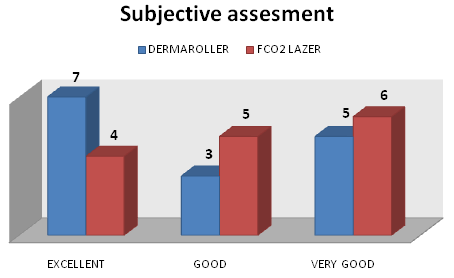
Figure 7 In group B: On comparison percentage of subjective improvement is more in group B than group A.
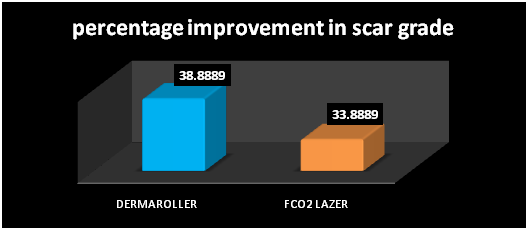
Figure 8 On comparison, both groups showed improvement of scars, but the percentage scar grade improvement was more in group B. The p value is 0.494.
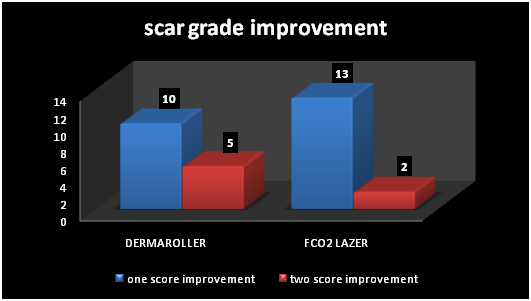
Figure 9 Erythema, edema, pain and pigmentation are some of the complications seen. Pain was recorded on a 4 point scale as 0=absent,1=mild, 2=moderate, 3=severe). In group A- 9(60%) patients experienced mild pain; 6(40%) patients, moderate pain. In group B- 2(13%) patients mild pain, 9(60%)experienced moderate pain, and 4(27%) experienced severe pain. In overall comparison group B patients experienced more pain than group A. Pigmentation was recorded on a 2 point scale i.e (0=absent, 1=present). In group A- 3 Patients (20%) developed hypo-pigmentation. In Group B- 4 patients (27%) developed hyperpigmentation. the study shows pigmentation is less common in both groups.
|
Grade |
Improvement |
|
Nil |
No improvement |
|
Satisfactory |
upto 25% improvement in score |
|
Good |
26–50%improvement |
|
Very Good |
51-75%improvement |
|
Excellent |
>75%improvement |
Table 1 Objective assessment
Evaluation of patient
Objective assessment: It was done using Goodman’s qualitative global acne scarring grading system7
|
Grade |
Points |
Improvemnt |
|
Nil |
0 |
No Impovement |
|
Satisfactory |
1 |
Upto 25% |
|
Good |
2 |
26-50% |
|
Very Good |
3 |
51-75% |
|
Excellent |
4 |
>75% |
Table 2 Subjective assessment
Subjective assessment: It is done using 5 point visual analog scale by patient himself. Grading is given in the table
|
N (%) |
Improvement |
|
2 (13.2%) |
Satisfactory <25% |
|
6 (40%) |
Good 26-50 % |
|
6 (40% ) |
Very good 51-75% |
|
1 (6.7%) |
Excellent >75 % |
Table 3 Objective assessment of group A as per Goodman’s qualitative global scoring system
|
N (%) |
Improvement |
|
1 (6.7%) |
Satisfactory <25% |
|
5 (33.3%) |
Good 26-50 % |
|
5 (33.3% ) |
Very good 51-75% |
|
4 (26.7%) |
Excellent >75 % |
Table 4 Objective assessment of group B as per Goodman’s qualitative global scoring system
|
N (%) |
Improvement |
|
0 |
Satisfactory <25% |
|
5 (33.3%) |
Good 26-50 % |
|
6 (40% ) |
Very good 51-75% |
|
4 (26.7%) |
Excellent >75 % |
Table 5 Subjective assessment of group A
|
N (%) |
Improvement |
|
0 |
Satisfactory <25% |
|
3 (20%) |
Good 26-50 % |
|
5 (33.3% ) |
Very good 51-75% |
|
7 (46.7%) |
Excellent >75 % |
Table 6 Subjective assessment of group B
FCO2 and Dermaroller are known treatment modalities for treatment of acne scar. SMP are newer superficial peels, they serve only to resurface the upper layers of the epidermis. Through an indirect, as-yet-unknown mechanism, they stimulate the dermal fibroblasts to deposit more collagen, elastin, and glycosaminogly cans in the papillary dermis. A more orderly and parallel arrangement of the fibers is also seen with this agent. Thus, a gradual and slight decrease in the number of superficial atrophic scars and a decrease in the depth of deeper atrophic scars is observed. In a study conducted by Manuskiatti et al.8 with FCO2 on acne scars at 6 month follow up , 85% patients reported 25-50% improvement and mild PIH as most common side effect. Garg et al.11 study showed percentage improvement in ice pick scars (week 0 to week 24) was 13.2% with SMP. Improvement in boxcar scars was 23.3%. In a study conducted by Imran Majid,12 out of 36 patients, 34(94%) achieved a reduction in the severity of their scarring by 1 or 2 grades. More than 80% of patients assessed their treatment as excellent response. In present study, on comparison, both groups showed decrease in all types of scars, but the percentage reduction i.e improvement was more in group B.
No single treatment modality can treat all types of scar’s. SMP newer superficial peel, serve only to resurface the upper layers of the epidermis with slight decrease in the number of superficial scars and a decrease in the depth of deeper scars can be used as adjuvant in acne scar treatment. This study concludes both treatment modalities are effective but more scar grade improvement was seen with DERMAROLLER+SMP (38.89%) than FCO2+SMP (33.89%) and shows a future treatment for acne scar patients.
None.
We declare no conflict of interest.
None.

©2020 Ittigi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.