Journal of
eISSN: 2574-9943


Case Report Volume 5 Issue 5
Dermatologist, Clinic of Dermatology, University of Belgrade, Serbia
Correspondence: Jelica Vukicevic, dermatologist, Clinic of Dermatology, School of Medicine, University of Belgrade, Clinical Center of Serbia, Serbia, Tel +381112682648
Received: December 10, 2021 | Published: December 24, 2021
Citation: Vukicevic J. Autosomal –dominant epidermodysplasia verruciformisun satisfactorily treated with ingenol mebutate: a case report. J Dermat Cosmetol. 2021;5(5):127-128. DOI: 10.15406/jdc.2021.05.00196
Background: Epidermodysplasia verruciformis (EV) is a rare, usually autosomal-recessive inherited disorder characterised by development of flat wartsortinea versicolor-like lesions on sun exposed area caused byspecific human papillomavirusis (HPVs). Several nonsurgical treatment modalities were tried with temporary results, but successful treatment of EV with ingenol mebutate (Picato) has been reported recently. In this case, autosomal-dominant EV unsatisfactorily treated with ingenol mebutate is shown.
Case: A 58-year-old woman with EV was unsuccessfully treated with traditional therapeutical modalities. Ingenol mebutate (0,5%) was administered for 2 days and a significant improvement in lesion reduction was achieved. However, after 2 months there was a recurrence with the appearance of new lesions and an increase of existing ones.
Conclusion: This report is another confirmation that EV remains a therapeutic challenge.
Keywords: epidermodysplasia verruciformis, human papilloma viruses, ingenol mebutate
Epidermodysplasia verruciformis (EV) is an extremely rare genodermatos is characterized by a unique susceptibility to specific strains of humanpapilomaviruses (HPVs).This HPV cutaneous infection is manifested as flat verrucous papules, or pityriasis versicolor-likemacules locatedpredominantly on sun-exposed areas and associated with a high risk of nonmelanotic skin cancer.1 EV is a lifelong disorder and several therapeutic strategies have been unsatisfactory. Recently, treatment with ingenol mebutate has been presented asa successful therapeutic approach.2 Here a rare case of autosomal- dominant EV unsuccessfully treated with ingenol mebutate is presented.
A 58-year-old woman presented on the Clinic of Dermatovenereology, Clinical center of Serbia, Belgrade, with lesionson the forearms and hands that lasted for several years. The patient noticed that her lesions became red and pruritic after sun exposure. She did not seek medical help until recently; however she protected the lesions from sun exposure. Her 81-year-old father had the same lesions on the dorsum of the hands which were, according to the medical record, histologically diagnosed as EV. She reported thather father,s lesions gradually resolved over time.
On examination, flat skin-colored or bright-red, asymptomatic, verrucae-planae-like papules were widespread on the extensor of the forearms and dorsum of hands (Figure 1A). There was no history of consanguinity.All routine blood analyses were within normal limits, and she deniedhaving any other associated disease. Signs of malignant alterations of the lesions were not observed. Human immunodeficiency virus (HIV) titers were also negative.
Biopsy of the skin lesions and HP analysis showed orthokeratotic type of hyperkeratosis with a basket weave-like pattern and increased granulous and spinous layers. The cells of these layers were large and the nests of the cellswith prominent perinuclear zone and grayish-blue cytoplasm (vacuolated cells) were present (Figure 2).
Liquid nitrogen was administered three times a week for 10 weeks, and 5% 5-fluorouracil were consequently given. No significant improvement was observed. Then 5% imiquimod cream and liquid nitrogen were alternately administered three times a week for 16 weeks. Rapid regression was noticed only in the beginning of the therapy, and then, stagnation was obvious. The papulae became slightly flattened, but the therapy was discontinued due to irritation of the surrounding skin. Aftera short period of anti- allergic therapy, thetreatment was continued with 0,05% tazarotene cream for 8 weeks. After the treatment interruption, new lesions and thickening of previously regressed lesions occurred.
Ingenol mebutate 0,05% gel was applied once daily for 2 days.The gel was applied on the lesions and were not washed or touched for 6h. Then, thetreated area was gently washed. Intensive desquamation, regression of the lesion and surrounding erythema was observed. Complete healing was not achieved (Figure 1B). During the control examination- after 2 months, new lesions appeared and preexisting lesions worsened (Figure 1C).
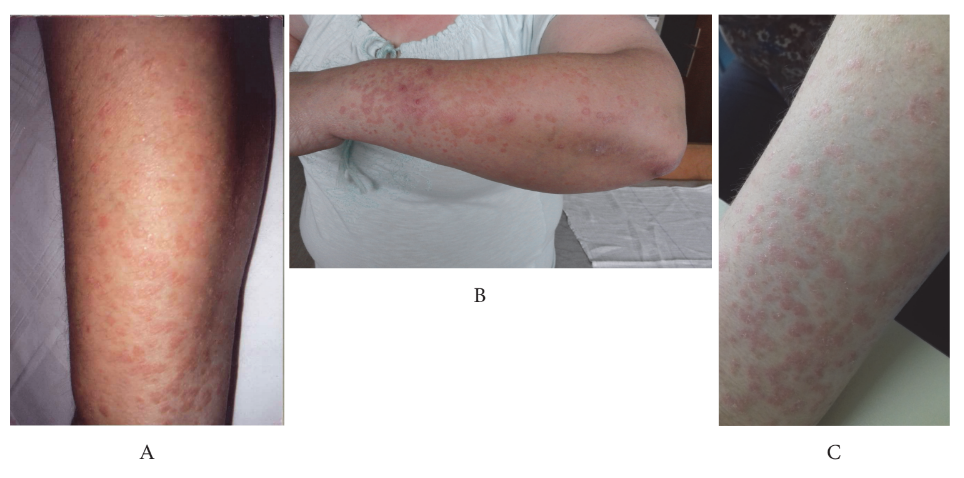
Figure 1 Verrucae-planae-like lesions on the forearm before treatment (A) After treatment with 0,05% ingenol mebutate, a significant volume reduction of papules with surrounding erythema is observed (B) Relaps on the first follow- up ( after 2 months) - the papules were more numerous and thickened (C).
Epidermodysplasia verruciformis, first described by Lewandowski and Lutz in 1922, is a genetically heterogeneous disorder characterizedby disseminated infection with EV-HPVs, immunologic abnormalities, and development of nonmelanoma skin tumors. It is a rare autosomal recessive genodermatosis, with cases linked to chromosome X. Only sporadic cases of autosomal- dominant inheritance of EV are described.3 Recently, acquired EV was observed in patients with impaired cell-mediated immunity.4
The lesions start to appear in early childhood, without gender or race preferences. The presentations are heterogeneous. The first lesions usually appearas flat warts on the back of hands. Pityriasis versicolor-like macules on the face and neck may also be present. The lesions of actinic keratoses appear after the third decade of life on the trunk, upper limbs and face.
More than 100 species of HPV have been identified in lesions of EV (the most commonly 3, 5, 8, 9, 10, 12, 14, 17, 19-25, 28 and 29). The malignant potential is most commonly shown in types 5 and 8.
If EV is present only with flat warts, it is considered to be associated with “benign“ nonocogenic HPV 3 or HPV 10. However, polymorphic lesions (“malignant forms“), are associated with some oncogenic HPVs, most commonly HPV 5 andHPV 8. EV cancers (Mb. Bowen, squamous cell cancer), which usually occurred on sun- exposed areas, show low metastatic potential. However, they may be very aggressive.5
This patient, as well as her father, clinicallypresented with flat warts only, without a malignant tendency. There is no specific therapy for EV. Some authors divided EV treatment into nonsurgical and surgical and stressed surgical treatment as considerably more effective.1 Several nonsurgical treatment modalities have already been tried for EV owing to stimulate the immune response and slowing the development and progression of cancers. At first, this patient was treated with liquid nitrogen and shortly after with 5-fluorouracil. Only slight depression of the lesions was achieved. In an attempt to decrease recurrence rates, combined therapy with imiquimod cream, immunomodulator, and liquid nitrogen were used. Rapid regression of the lesions was observed in the beginning of this therapy. Further, stagnation was obvious and worsening occurred immediately after therapy completion. Based on our literature review, Heratizadeh A. et al.,6 and Berthelot C. et al.7 reported the use of imiquimod as a successful treatment for EV.6,7 However, this case presented unsuccessful treatment of EV with imiquimod which is in accordance with the recently published results.2 Anecdotal efficiency of oral zinc and topical squaric acid dibutyl ester in EV were also described.8,9 Surgical excision is the treatment of choice for squamous cell cancer.
Recently, successful treatment of EV with ingenol mebutate reported.2 It seems that ingenol mebutate has a dual mechanism of action rapid lesion necrosis and specific neutrophil-mediated, antibody-dependent cellular cytotoxicity. In the presented patient, the use ingenol mebutate was significantly effective with moderate irritation of the surrounding skin. However, a relapse with significant deterioration was observed on the first follow-up.
Unfortunately, this case is another confirmation of EV,s resistance to the therapy.
The authors declare no conflict of interest.
None.
None.

©2021 Vukicevic. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.