Journal of
eISSN: 2574-9943


Research Article Volume 7 Issue 2
LCMA Dermatology Clinic, Dermatology, Brazil
Correspondence: Luciana Cirillo Maluf Azevedo, LCMA Dermatology Clinic, Dermatology, Brazil, Tel +55 11 99274-1841
Received: May 11, 2023 | Published: June 5, 2023
Citation: Azevedo LCM,Valim CS. A novel technique for repositioning facial soft tissues with barbed polydioxanone threads based on the main aging vector force of rejuvenation. J Dermat Cosmetol. 2023;7(2):57-61. DOI: 10.15406/jdc.2023.07.00235
Background: With the evolution of facial rejuvenation procedures, thread lifts have gained space among western patients who seek cosmetic improvement without undergo to surgeries. Absorbable wedge-shaped polydioxanone (PDO) sutures are currently available, and in mid-lower face and mandibular jowl lift, threads are most often implanted in a diagonal vector force from medial-inferior up to lateral-superior site, near the temple. Herein, the authors introduce a new technique based on this oblique sum of anti-aging vector force to reposition and anchorage facial soft tissues, aimed for natural youth rejuvenation.
Objective: Describe a novel technique for counteracting the facial ptosis and laxity skin, as well as the duration of clinical lifting result and of skin quality improvement.
Methods: More than 84 patients were underwent in this thread technique once. The outcomes were assessed objectively using serial photography and subjectively based on the patients’ spontaneous satisfaction through over these 4 years. Complications were also reported.
Results: Most patients considered the results satisfactory. The incidence of complications was low, and most of them were minor and temporary.
Conclusion: Wedge-shaped PDO thread repositioning and anchorage soft tissue is safe and effective method for rejuvenation.
Keywords: nonsurgical lift, threads, rejuvenation, youth face, facial anti-aging vector force
From birth throughout life, the aging process keeps going unabated. The face has all structures affected: skin, fat compartments, muscles, retaining ligaments and skeleton.1 In addition, age might change not only the skin quality and quantity (hydration, wrinkles, sagginess), but also reduce the skin collagen synthesis.1 It may also compromise the deeper facial layers. The volume loss of deep and superficial fat pads leads to skin laxity, prominent nasal labial and labial mentual folds, jowls formation and the descent of the periorbital site.1,2 Also, facial bone aging changes and, consequently it compromises the position and the stability of ligaments that bend along each of their courses, affecting the subcutaneous compartments and the adhesions up to the skin.3
Furthermore, by the Newton’s parallelogram or triangular rules,4 the main aging facial vector force has to be found. Gravity and the descent facial soft tissues - skin, retaining ligaments, fat compartments, loose muscles and facial fascias - play a role sliding onto the deep facial structures medially and downwards. If every action is accompanied by a reaction of an equal magnitude but opposite direction, the main anti-aging vector force (AAVF) plays an upward and lateral vector counteraction, repositioning all the drop of the superficial mobile layers.5 (Figure 1, Figure 2).
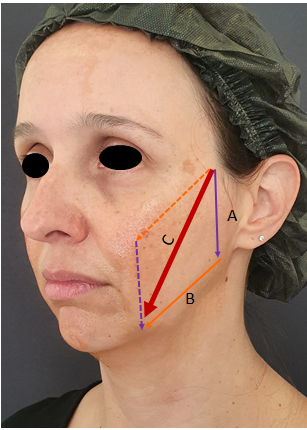
Figure 1 Triangular rule or the parallelogram rule: A) Gravity force vector; B) Flattened retained ligaments and fad pads force vector; C) The sum facial age force vector.
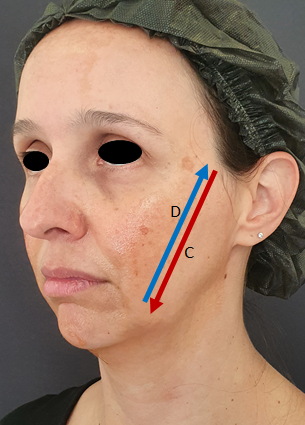
Figure 2 By Newton’s third law, vector D is equal vector C in force and magnitude, but in the opposite direction. Vector D may guide non-surgical procedures.
We propose a novel conceptual absorbable barbed polydioxanone (PDO) thread application based on these vectorial forces rules and the connection between the soft tissues to the depth. With all subjects in an upright position - not to alter the gravity vector force - four crucial pulling points were pinpointed over the lower face. And, by making a slight finger test onto the skin, the major AAVF could be found, which not only might guide and lead to a better natural and phisiologycal nonsurgical beauty rejuvenation, but also can soften the jowls and both folds – nasolabial e labiomentual ones.
For that, some important anatomy concepts have to be known: midface has two different SMAS areas that histologically show fibrous septa, which in turn, build fat compartments. In the preparotideal site, connections of fibrous septa between the skin and the mimic muscles were showed. And, in the parotideal one, there is parallel alignment of the fibrous septa, anchoring the skin to the parotid fascia.6
Furthermore, the retaining ligaments of the cheek must be kept in mind at all times: the zygomatic ligament and the mandibular ligaments tether the facial bone up to the skin. The platysma auricular ligament and the anterior platysma cutaneous ligament are condensations of platysma fascia that extend up to the dermis. And in the anterior border of the masseter muscle there is a vertical septum that links the masseteric fascia to the overlying muscular aponeurotic system (SMAS).7 The SMAS superficial facial fascia is dense and wraps the platysma muscle within the cheek. Thus, in some locations the superficial and deep facial fascias are toughly adherent to each other: through the anterior border of the masseter muscle and overlying the parotid gland.8 In addition, there is a line of ligaments that separates the mobile (anterior) face from the relatively fixed (posterior) face.9 Other ligaments are the temporal ligamentous adhesion (TLA), lateral orbital thickening (LOT) both considered triangular fibrous condensations,10 zygomatic, masseteric and mandibular ligaments.9 (Figure 3)

Figure 3 A vertical line of retaining ligament. From the top of skull down to the mandible/mandibular bone, the ligaments are: temporal ligamentous adhesion (TLA), lateral orbital thickening (LOT), zygomatic cutaneous ligament (ZCL), masseteric ligaments (MaL) and mandibular ligaments (ML).
The facial ligament supports, tethers and keeps skin and SMAS stabilized and settled to the bone and together - with the retinacula cutis – and it might create adhesion sites to divide the face into superficial and deep fat pads.9,11 The zones between the ligaments are potential spaces and compartments which facial movements can be made.9,12,13 At the same time, there is growing evidence that skin aging is not only and solely connected with its structure modification, but also it’s significantly depending on the properties of the underlying subcutaneous white adipose tissue.14
Most of the alterations might happen into the finer superficial retinacula cutis branches - from the SMAS through the subcutaneous fat layer up to the dermis -, which lose strength over the years because of repetitive movements.9,15 Facial ligaments are fully involved with both fat compartments and mimetic muscles giving that fascia an ongoing extension. Superficial fat layers tend to move and are subject to both the resting and dynamic strains of the mimetic muscles.9 Mimetic muscles are one of those responsible for changing the facial volume and contour by inserting themselves into the dermis and thereby playing a role in both the suspension and structural integrity of the soft tissue envelope.9,16,17
Based on anatomy and the main mid-inferior facial aging vector force (AVF) in every patient, this new technique is being conducted at LCMA Dermatology Clinic, São Paulo/Brazil for four years (more than 84 cases). For these cases, at least 4 barbed threads (I-Thread, barbed PDO thread 19G/100mm/160mm, Hyundae Meditech Co./ Korea) on each side, from middle to lower face are being suggested, in order to make the main physiological soft tissue suspension and anchorage.
The patient must be outlined in the upright position:
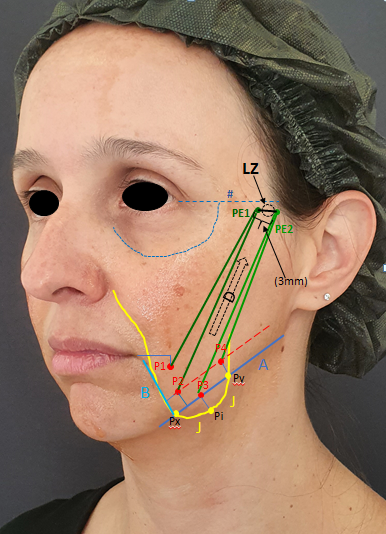
Figure 4 The draw marks. A) mandible body line; B) labialmentual fold down to mandibular ligament; J) the jowl; Px and Py) jowl’s draw points that cross the line A; Pi) The lowest point of the jowl; P1, P2, P3, P4) the main pulling points. P3 is the transposition of Pi into the line A. The main anti-aging force vector (D) that was found by making the slight finger test and looking for the easiest narrow zone (Luciana-Zone; LZ) to pull P1-P4 up; PE1 and PE2) the entrance points of the barbed threads. The distance between PE1 and PE2 is 3mm, to soften the inflammation (instead of only one entrance point).

Figure 5 The draw measures (in cm) and positions of the barbed end points P1, P2, P3, P4.
A) Mandible body line. Pi is the lowest point of the jowl (J) clinically demarcated. P3 is the transposition of Pi into the line A.
LZ (Luciana-Zone) narrow strip zone was found by making the slightly finger test. PE1 and PE2 the entrance points of the barbed threads and were 3.0mm separated.
The procedure was well tolerated and caused minimal discomfort under topical and local intradermal anesthetics for most patients, and none of them asked for further sedation. It was considered a relatively fast procedure (around 50 minutes).
This technique can naturally smoothen the traits of age without losing the peculiarities of each and every patient by repositioning the soft tissues. It can also alleviate the jowls and both folds - nasolabial e labiomentual ones. (Figure 6 & Figure 7)

Figure 7 Pulling the barbed threads to smoothen the jowls, the nasolabial and the labiomentual folds.
Based on spontaneous reports, most patients could clinically notice a softer aging face right after the procedure and mainly around 3-4 months. They were very satisfied with the results and all of them (100%) could feel skin quality improvement becoming gradually better, with the greatest firmness skin texture around 9-11 months. And, based on pre-treatment, and 3 and 5 month pictures, we can observe skin quality improvement and long lasting soft tissue repositioning results. (Figure 8 A, B, C & Figure 9 A, B, C).
On monthly follow-up visits some side effects were pointed out: mostly minimal bruises (and two large ones maybe owing to previous rhytidoplasty, which might have altered the anatomy), minor to moderate swelling and pain or sensitivity, some dimples and one foreign body granuloma due to an implantation of a hair along with the thread knot into the skin. Significant adverse events such as nerve or muscle damages, lip rhyme deviation or transfixation of the parotid duct were not observed.
According to the Facial Laxity Rating Scale (Classes 1–9: mild, moderate, and severe laxity),18 we could observe at LCMA Dermatology Clinic that patients who were selected from class 1 up to class 5 for the treatment present better results, agreeing with another study that confirms the thread procedure is indicated for those who are relatively young and have a modest degree of facial soft tissue laxity,19 and for patients who want to improve the jowls with up to moderate sagginess without plastic surgery.20
We could soften the jowls and the nasolabial and labialmentual folds pulling the mobile tissues within the main AAVF - a diagonal from medialinferior toward the temple area -, implanting only four barbed threads per hemiface (total of 8 threads) into the subcutaneous layer around the zigomatic bone area near the hair implantation line (LZ) - found by the slight finger test. An interesting article identified the angle of maximal rejuvenation during rhytidectomy saying it was more superior than posterior.21 In our methodology, we could reinforce it with the “finger test”, even though it was done with patients in the upright position. The most important limitation of this technique is that it is not indicated for moderate to severe facial soft tissue laxity. Skin quality is essential in order to grab the barbed threads and fix them into the subcutaneous layer so to obtain better and longer lasting results.
Furthermore, all patients who underwent this thread procedure, reported the improvement of skin quality (better texture, brightness and firmness). Some histological articles revealed that, upon collagen formation, the dermal collagen fibers thickened and the elastic punctform fibers became longer, persisting for up to twelve months.22,23 And, some collagen fibers that grew around the thread started to connect and merge with the pre-existing fibrous connective tissue. Through this process, thick fibrous bridges are formed and link the dermis toward the fascia, enhancing the quality of the superficial connective area down to depth.22
Side effects might occur in every cosmetic procedure. In our clinic, bruises, minimal swelling, minimal to moderate pain or sensitivity are common. It is sorted out with pain medication. Foreign body granuloma could be possible if a hair implantation happens along with the thread knots. It is resolved by incision and hair removal from the skin, and massage with corticosteroid cream. Dimples were adjusted with massage and, in the minority of cases, subcision with local anestesia was needed. Significant adverse events were not observed due to the correct thread technique, which is into the superficial subcutaneous layer. In addition, any previous facial surgery or rhythidectomy must be informed prior to thread procedures, since the anatomy might be altered.
Although the mid-lower face improvement, for those with heavy face or significant jawl line, may require more threads or other skin techniques for better contour and results.19 From this point, not only it’s demanded individualizing treatment depending on particular issues and needs, but also detailed anatomical understanding and attention to the degree of skin laxity.21
Nevertheless, each and every patient is unique, given the huge variability in facial physiognomy between genders and races as well as the differing ethnic ability to produce collagen and elastin. So that, there is no single diagram for occurrence and development of facial true retaining ligaments7 In addition, in the same ethnicity, there is variation in density, shape, and distribution of these retaining ligaments. Everyone has their own particular ligamentous anatomy and topography. Consequently, the onset and outcome of aging varies,7 high cheekbones are attractive and a beauty pattern for westerners, although not appreciated by the Asian culture.19 So, we must pay attention to all these issues. Overall, spontaneous data about the efficacy of AAVF wedge-shaped PDO thread implantation for soft tissue suspension and repositioning was favorable, the clinic outcome satisfaction rate ranges around 6 months, and the skin quality improvement rate, around 12 months.
None.
Authors declare there is no conflict of interest.

©2023 Azevedo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.