Journal of
eISSN: 2574-9943


Case Report Volume 2 Issue 1
Department of Dermatology, University Hospital Hassan II, Morocco
Correspondence: Senhaji Ghita, Doctor, Department of Dermatology, University hospital Hassan II, Fes, Morocco, Tel +212 600075857
Received: August 18, 2017 | Published: January 23, 2018
Citation: Senhaji G, Gallouj S, Assenhaji I, et al. Giant plexiform neurofibroma of the pelvic region: unusual presentation in an uncommon location (about a case). J Dermat Cosmetol. 2018;2(1):20-23. DOI: 10.15406/jdc.2018.02.00030
Plexiform neurofibroma is a rare benign tumor of the peripheral tissue cells developed in the perineurium, generally associated with neurofibromatosis type 1 (NF1). These entities consist of multiple, twisted masses that grow along the axis of a large nerve, infiltrating and separating normal nerve fascicles. The diagnosis is essentially pathological and treatment is primarily surgical to avoid malignant degeneration. Giant neurofibromas are very difficult to manage surgically as they are extensively infiltrative and highly vascularized. This report describes a case of an advanced plexiform neurofibroma of the right lower back and pelvic region in a 25-year-old female with neurofibromatosis type 1, discovered in early childhood, with limited normal living due to the severe disfigurement as the result of progression of the disease.
Keywords: plexiform neurofibroma, neurofibromatosis, tumor, pelvic, von recklinghausen
NF1, neurofibromatosis type 1; PNF, plexiform neurofibroma
Plexiform neurofibroma is a rare benign tumor of the peripheral tissue cells developed in the perineurium. Often considered pathognomonic of neurofibromatosis type 1 (NF1 or von Recklinghausen disease), it can be solitary, especially in children.1 These entities consist of multiple, twisted masses that grow along the axis of a large nerve, infiltrating and separating normal nerve fascicles.2 It rarely grows to be larger than 5cm; however, neurofibromas can undergo continuous enlargement and eventually become giant lesions.3 Thus, it constitutes a significant source of structural and functional morbidity.4 The diagnosis is essentially pathological1 and malignant transformation is the main associated complication.2 Surgery is frequently reserved until PNs have progressed to the point of causing functional compromise, esthetic deformity or pain.2 We report here a case of a giant PNF of the lower back and pelvic region, with presentation of the clinical and radiological findings.
A 25 year-old female patient was referred to our dermatology department for evaluation of a progressive large mass of the right buttock, the lower lumbar region and the right thigh, that began in early childhood (at around 4 years of age). The mass was initially painless and had gradually enlarged during this time. However, it became painful since a year, which motivated her consultation to an orthopedic department, where radiological examinations with biopsy were performed objectifying neurofibroma, and then she was referred to our department for support. Her medical history was unremarkable and none of the relatives was known to be affected. No prior attempts at resection or tumor debulking were undertaken.
Physical examination revealed a large, firm, infiltrated, dark brown lesion, well limited with irregular contours measuring 60 cm, at the right thigh, lower half of the abdomen and pubis, with the presence, next to it, of an amorphous fluctuant soft tumor, taking all the right buttock and the right inguinal region. Multiple café au lait spots were seen on the patient’s body (36 lesions) and cutaneous and subcutaneous neurofibromas were seen over the trunk and the extremities, consistent with a diagnosis of NF1 (Figure 1). There were some lesions with located hypertrichosis, producing a nevoid aspect. Neurological examination was normal.
Routine laboratory tests were normal. In X-ray, the pelvic region showed a deformation with an extensive osteolytic process in the right iliac bone and osteo-condensation areas. Abdominal pelvic CT scan demonstrated a remodeled bone frame at the right hip bone and sacroiliac joint, with an important fibro-fatty pseudotumoral infiltration interesting the right buttock and blank. An incisional biopsy of the bone was performed and the histological findings were consistent with neurofibroma. There was no evidence of malignancy in the tissue sample. Ophthalmological examination was normal. Magnetic resonance imaging (MRI) of the abdomino-pelvic area with the thigh was solicited and revealed a tissular homogeneous process of the right gluteal area, measuring 20x6x19 centimeters, that infiltrate the surrounding soft tissue structures, the underlying gluteal musculature (medial and large gluteal muscles), the fascia and the greasy subcutaneous plane, cross by branches of the internal iliac artery that remain permeable. There were no signal abnormalities of the bone structures. The mass exhibited iso intense signal on T1 and increased signal intensity on T2 and STIR weighted images, with low endovenous contrast enhancement.
Findings on physical exam and imaging were consistent with a diagnosis of a large plexiform neurofibroma of the pelvic region.
The case was reviewed at a multidisciplinary committee, including orthopedic and plastic surgeons. Considering the vascularity and size of the lesion, the treatment consensus opted for conservative management with clinical follow-up every 6 months. It was not feasible to widely excise the lesion as it was infiltrating almost circumferentially around the patient.
Plexiform neurofibromas occur in up to 30% of cases of NF-1, most frequently in the craniomaxillofacial region.5 They can be present at birth, but often appear between the ages of 2 and 5.6 It occurs frequently in the head and neck region due to the rich nerve innervations; however, it also appears on rare occasions in the extremities.7 In the present case, plexiform neurofibroma arises from the right buttock, the lower lumbar region and the right thigh which are very rare locations (Figure 2).
There are two types of plexiform neurofibromas, nodular and diffuse.8 Nodular plexiform neurofibromas occur less frequently and present with multiple discrete nodular tumors. On the other hand, diffuse plexiform neurofibromas are generally large, infiltrative tumors, without defined borders. They entail pigmented, overlying skin with an angiomatous aspect; hypertrichosis may also be located in the lesion, producing a nevoid aspect, also seen in our patient. Two main features stand out: hyper extensibility with a lack of elasticity.6 They arise as a diffuse mass from nerve trunk and lead to overgrowth of cutis and sub cutis structure and give a characteristic appearance of “Bag of worm”.9 Masses can lead to disfigurement, erosion of adjacent bone, and scoliosis.10 They are generally diagnosed clinically with appreciation of the typical features, and histopathology is useful to exclude malignant transformation.5
A diffuse plexiform neurofibroma form, also known as elephantiasis neurofibromatosis, is characterized by an overgrowth of epidermal and subcutaneous tissue associated with a wrinkled and pendulous appearance.8 This patient presented with a giant diffuse plexiform neurofibroma associated with NF1 that had been growing for more than 20 years. Although there was most unilateral soft tissue hypertrophy with limb length asymmetry due to the tumor, it did not exhibit cutaneous signs associated with elephantiasis neurofibromatosis.
There is a significant discrepancy in the size of tumors that are described as “giant” neurofibromas. Some authors reserve this term for tumors weighing more than 20 kg, even though no clear consensus has been reached. These tumors present complex management issues of wound closure, intra-compartmental fluid shifts, and lymphedema.3
Neurofibromas may present on ultrasound as numerous hypoechoic masses along the distribution of peripheral nerves.10 Ultrasounds can still rule out a tumor or a high flow vascular malformation.11 Non enhanced computed tomography scans typically show low-attenuation masses, measuring approximately 15 to 30 Hounsfield units, due to the high water content of the mucinous matrix, cystic degeneration, and lipid components of neurofibromas.10 In our case, it showed a remodeled bone frame with an important fibro-fatty pseudotumoral infiltration interesting the right buttock and blank. MRI is the method of choice for the diagnosis and follow-up of neurofibromas.2 Thus, it was also chosen for our patient. It can be used to determine the diagnosis, morphology, type and size of lesion and extent of disease and to differentiate superficial PNFs from other very similar lesions, such as lymphatic or venous malformations and hemangiomas. Especially, MRI helps to differentiate a PNF from a malignant peripheral nerve sheath tumor.7 In T1 weighted image, a PN is iso intense in relation to muscle tissue. In T2 weighted sequence, a PN is seen as a hyper intense, homogeneous image with “target sign”, owing to the central fibrous tissue surrounded by myxoid tissue.2 They are best seen on fat-suppressed T2 as multinodular confluent masses along the distribution of peripheral nerves.10 Our patient’s MRI revealed a tissular homogeneous process infiltrating the surrounding soft tissue structures, the underlying musculature, the fascia and the greasy subcutaneous plane, with an iso intense signal on T1, increased signal intensity on T2 and STIR weighted images, with low endovenous contrast enhancement (Figures 3A-3C).
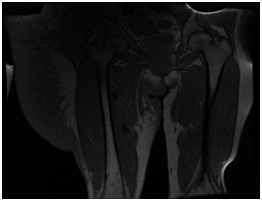
(A) A tissular homogeneous mass of the right gluteal area, infiltrating the soft tissue structures, the gluteal musculature, the fascia and the greasy subcutaneous plane, with an iso intense signal on T1.

(B) Increased signal intensity on T2 and STIR weighted images.

(C) Low endovenous contrast enhancement.
Figure 3 Abdominopelvic MRI.
PNF is histologically characterized with proliferation of the Schwann cells in the nerve sheath, involving multiple fascicles and multiple nerves throughout the nerve involved.7 It consists of a proliferation of Schwann cells arranged in a myxoid variable abundance tissue with many fibroblasts and collagen fibers with an aspect-called "grated carrots." The presence of anti-neurofilament antibodies in the proliferation may help the diagnosis. The cell shape may mimic schwannoma but in immune-histochemistry, S100 protein is less expressed than in schwannoma.11
Clinical management for the PNF requires a multidisciplinary approach.3 Surgical treatment still remains the mainstream, aiming at improving functional and aesthetic effect.12 Traditional indications for surgical treatment have focused on symptomatic relief of neuropathic pain and/or compressive neuropathy through limited resection and internal neurolysis or conservative tumor debulking. Results with this approach, however, are often limited by a strong tendency toward recurrence and a propensity for malignant degeneration.4 In addition to this, a complete resection is often difficult due to the extensive growths of the tumors and invasion of the surrounding tissues, and re-growth after surgery is common. 7Moreover, the tumor contains thickened cord of nerves along with abundant abnormal vessels; therefore, excessive hemorrhage during the operation is also a brainteaser. Furthermore, if the nerve roots of neurofibromas are from major nerves, surgical resection may result in functional impairment.12 Some authors propose regular follow-up examinations involving serial physical evaluations and neuroimaging studies.10 This was the conduct used in the present case.
Growth of a PNF can occur at any time in life, and a PNF has an unpredictable pattern of growth. PNFs tend to grow during times of hormonal change, such as early childhood, puberty, or pregnancy, and then, in some cases, stop entirely. 7Our patient’s tumor gradually increased in size from childhood to adulthood, but manifests a rapid growth pattern during puberty.
Malignant transformation is the leading complication of PN. The lifetime risk of this transformation is estimated at 15 to 20% in patients with NF-1,2 most commonly presenting during adulthood at approximately 20 to 50 years old. Findings which favor malignant over benign peripheral nerve sheath tumors include: enlarging mass, size greater than 5 cm, ill-defined margins, perilesional edema, peripheral enhancement pattern, lack of central hypo intense “target” on T2 sequences, and heterogeneity with central necrosis.10 These signs must force us to realize a radiological examination (MRI), as in our patient, and consider an early surgical revision.11
In this case, normal living was limited due to the severe disfigurement as the result of progression of the disease. After multidisciplinary review, the approach was to avoid surgery and to undergo clinical follow-up every 6 months.
To sum up, we present the rare case of an advanced PNF of the pelvis with associated muscular and skeletal destruction. Through in this case we highlight the importance of early consultation to avoid occurrence of such giant tumor, difficult to be managed. We also brought into side the need of clinical and radiological examinations with multidisciplinary approach in the management of this type of tumors. Finally, we insist on the need of a regular clinical and radiological monitoring of these patients to assess malignant transformation.
To the staff of the dermatological department of the Moroccan University Hospital Hassan II.
The authors declare no financial or any conflict of interest.
Patient consent related case report take the permission from concerned patient.

©2018 Senhaji, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.