Journal of
eISSN: 2373-633X


Case Report Volume 14 Issue 2
Depatment of Urology, CHU de Fès, Morocco
Correspondence: N Alaoui Mhammedi, Depatment of Urology, CHU de Fès, 21 Rue Agadir, Meknès, Morocco, Tel 0629211712
Received: April 03, 2023 | Published: April 13, 2023
Citation: Mhammedi NA, Ouaddane RA, Ahssaini M, et al. Case report of a very rare testicular tumor. J Cancer Prev Curr Res. 2023;14(2):52-53. DOI: 10.15406/jcpcr.2023.14.00518
Myoid tumor of the testis is a rare neoplasm that originates from the smooth muscle cells of the tunica albuginea. It is usually benign and presents as a painless testicular mass. The diagnosis is confirmed by histopathological examination. The treatment of choice is radical orchiectomy. Recurrence is uncommon, and long-term follow-up is recommended. In this abstract, we review the clinical presentation, diagnosis, treatment, and prognosis of myoid tumor of the testis based on current literature.
A myoid tumor of the testis, also known as a testicular leiomyoma or leiomyosarcoma, is a rare type of tumor that develops in the smooth muscle cells of the testis. These tumors are typically benign, meaning they do not spread to other parts of the body, but in some cases they may be malignant, meaning they have the potential to metastasize and invade surrounding tissues.
Myoid tumors of the testis can occur in men of any age, but they are most commonly diagnosed in middle-aged or older men. They often present as painless testicular masses, which can be detected through a physical examination or imaging studies such as ultrasound.
The exact cause of myoid tumors of the testis is unknown, but some researchers believe they may be related to hormonal imbalances or exposure to environmental toxins. Treatment typically involves surgical removal of the tumor, and in some cases, radiation therapy or chemotherapy may be used to prevent recurrence.
It is about a young patient aged 27 years, married, without particular pathological history, who consulted for the appearance since 4 months of a left testicular mass without other associated signs, his physical appearance was normal, without dysmorphism or signs of feminization.
The clinical examination showed a left testicular mass, hard, not too painful to palpation, the lymph nodes were free. The result of the hormonal balance (LDH, FP, HCG) was normal Doppler ultrasound noted a hypoechoic, heterogeneous, very well limited left testicular mass measuring 40/35 mm (Figure 1), contralateral testicle of normal size with no abnormality, CT scan as an extension assessment came back without secondary lesions. The patient benefited from a total orchidectomy of the left side by inguinal way (Figure 2), the postoperative continuations were simple, the patient left the hospital the same day.
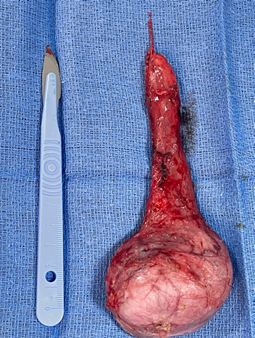
Figure 2 Operative image of the left testicle after orchiectomy (Department of urology CHU HASSAN II FES).
Anatomopathological and immunohistochemical study showed tumor cells expressing AML and PS100 and not expressing DESMINE, H-caldesmone, CALRETININE, INHIBIN or CK, KI67 was estimated to be 10%, which was compatible with a gonadal myoid stromal tumor (Figure 3).
Myoid tumors of the testis, also known as Leydig cell tumors, are rare testicular neoplasms that arise from the interstitial Leydig cells within the testis. These tumors account for less than 1% of all testicular tumors and are typically unilateral, solitary masses. While myoid tumors of the testis are typically benign, they have the potential to become malignant and metastasize to other organs. Due to their rarity, limited knowledge exists regarding the optimal management of these tumors, and further research is needed to better understand their pathogenesis and clinical behavior.1,2
Leydig cell tumors are believed to originate from the Leydig cells, which are responsible for the production of testosterone in the testes. These tumors are often asymptomatic and are discovered incidentally during a routine physical exam or ultrasound.3 However, they can present with symptoms such as pain, swelling, or a mass in the testicle.4 The diagnosis of myoid tumors of the testis is typically made through a combination of physical examination, imaging studies, and histological analysis of a biopsy or excision specimen.5
The optimal management of myoid tumors of the testis is still a matter of debate, given the rarity of these tumors and the lack of robust data on their clinical behavior. However, current guidelines recommend surgical excision of the affected testis, with the extent of surgical resection dependent on the tumor size, location, and presence of malignancy.6,7
According to a case report by Ceballos-Quintal et al.,8 myoid tumors of the testis can present as a large testicular mass with infiltrative features and may be associated with reactive lymphoid follicles. Histologically, the tumors show fascicles of spindle cells with eosinophilic cytoplasm and elongated nuclei, arranged in a whorled or storiform pattern. Immunohistochemistry is essential to confirm the diagnosis, with positive staining for smooth muscle markers, such as desmin and smooth muscle actin.
Myoid tumors of the testis are considered low-grade malignancies, and the prognosis is generally favorable. However, there have been rare cases of metastasis, as reported by Patel et al.,9 who described a case of myoid tumor of the testis that metastasized to the lungs. Therefore, long-term follow-up is recommended, with imaging studies to monitor for recurrence or metastasis.
Treatment for myoid tumors of the testis is orchidectomy, which is usually curative for benign tumors. However, for malignant tumors, adjuvant therapy, such as chemotherapy or radiotherapy, may be necessary. According to a retrospective study by Kim et al.,10 patients with malignant myoid tumors of the testis had a higher risk of recurrence and metastasis, and adjuvant therapy was associated with a better prognosis.
In conclusion, myoid tumors of the testis are rare neoplasms that require histologic examination for definitive diagnosis. They are generally considered low-grade malignancies, but metastasis and recurrence can occur. Orchidectomy is the treatment of choice for benign and malignant tumors, with adjuvant therapy reserved for malignant tumors with high-risk features. Long-term follow-up is recommended to monitor for recurrence and metastasis.
Myoid tumors of the testis are rare tumors that require careful diagnosis and management. Although they are typically benign, radical orchiectomy is the treatment of choice due to the potential for malignant transformation. Ongoing research is needed to better understand the biology of these tumors and identify potential targeted therapies for more aggressive or recurrent cases.
None.
Authors declare that there is no conflict of interest.

©2023 Mhammedi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.