Journal of
eISSN: 2373-633X


Case Report Volume 3 Issue 1
1Department of Oral and Maxillofacial Radiology, Ahvaz Jundishapur University of Medical Sciences, Iran
2Department of Oral and Maxillofacial Radiology, Ahvaz Jundishapur University of Medical Sciences, Iran
3Department of oral and maxillofacial surgery Oral and maxillofacial surgery, Hormozgan University of Medical Sciences, Iran
Correspondence: Ali Habibi Kia, Postgraduate Student of Oral and Maxillofacial Radiology, Faculty of dentistry, Ahvaz Jundishapur University of Medical Sciences. Ahvaz, khouzestan, Iran, Tel 9169015391
Received: January 25, 2015 | Published: July 28, 2015
Citation: Abbassi S, Kia AH, Hemmat S. Nasopalatine duct cyst: a case report. J Cancer Prev Curr Res. 2015;3(1):201-203. DOI: 10.15406/jcpcr.2015.03.00066
Nasopalatine duct cysts are the most common of developmental non-odontogenic cysts in the oral cavity and represent 10% of maxillary cysts. The cyst arises from epithelial remnants from the nasopalatine duct. These cysts are usually asymptomatic, but the most commonly reported clinical symptom is swelling in the anterior part of the palate, just behind the palatal papilla. This swelling is not always on midline. The recurrence of this is rare (2%). In this report, a 21-year-old man from Ahvaz, with the chief complaints of numbness, anterior teeth mobility, intraoral swelling and facial asymmetry, is reported. On clinical examination, a non tender swelling on the midline of hard palate and buccal vestibule, covered by normal mucosa was seen. The crown of central incisors was displaced medially. In panoramic, maxillary occlusal cross sectional, anterior maxillary periapical and computed tomography views, well-defined unilacular radiolucency with corticated margins was seen in the anterior region of maxilla. Biopsy of the lesion was planned and final pathologic diagnosis was “nasopalatine duct cyst”. Therefore, nasopalatine duct cyst, is one of the differential diagnoses of unilacular radiolucencies in the anterior region of maxilla. Histopathologic examinations help us to reach the correct diagnosis and disburden us from unnecessary treatments.
Keywords: nasopalatine duct cyst, non-odontogenic cyst, developmental cyst
KOT, keratocyst odontogenic tumour; CGCG, central giant-cell granuloma; RCT, root canal therapy; CT, computed tomography
Nasopalatine duct cyst was described by Meyer for the first time in 1914.1,2 This cyst is the most common non-odontogenic, developmental-evolutionary cyst of the oral cavity3 and is also known as the incisive canal cyst, anterior palatine cyst and the median anterior maxillary cyst.4 It is believed that this cyst can be originated from the epithelial remains of the nasopalatine duct.3,5 This cyst includes 10% of jaw cysts4 and involves 1% of the total population.3,6 Its age distribution is broad and discovered in most cases in the fourth and sixth decades of life4,7 and in a wide study of 334 cases of nasopalatine duct cyst on the average age was 42.5 years.8,9 The prevalence of these cysts in women is three times the men.4,10,11 Etiology of this cyst is unknown,1,10,12 although factors such as trauma, infection of the duct, and commonly spontaneous cystic degeneration have been considered as possible factors in the remains of the nasopalatine duct.3,12
Most of these cysts are asymptomatic4,8 or create mild symptoms that are tolerable for a long time.4 If any symptoms, the most common symptom is a small swelling with well defined border in the posterior of palatal papillae4,8–12 that is not always symmetrical to the midline.4 The pressure exerted by the cyst to nasopalatine nerves in the vicinity of the cyst can cause a sensation of burning or numbness of mucus.4
The occlusal and periapical radiography view of the maxillary central incisors teeth show a cyst-like radiolucency with a well defined and cortical border in the shape of a circle or ellipse; sometimes due to being superimposed nasal spine shadow on the cyst, lesion appears to be heart-shaped.4,12–14 This cyst mostly causes divergence of the roots of the central teeth from each other and sometimes root resorption happens.4 The most common differential diagnosis is a large foramen incisive;4 in total, other differential diagnosis includes radicular cyst,4,8,14 keratocyst odontogenic tumour (KOT),8,12 central giant-cell granuloma (CGCG).5,9,14
In terms of histopathology the epithelium of cysts is very diverse12 and includes a combination of stratified, squamous, non-keratinized epithelium, false stratified columnar epithelium, stratified columnar epithelium and simple cubic epithelium.8,12 The connective wall of cyst may contain nasopalatine vessels and nerves as well as the glandular structures.15
The appropriate treatment for these cysts can be enucleation4,12 and in order to prevent damage to the nasopalatine nerve the enucleation is done from the side of the palate.4 If the cyst is large and there is a risk of loss of teeth vitality or creation of a nasal fistula in the mouth and sinus, the surgeon may choose the marsupialization method.4,7 The rate of recurrence of this lesion has been reported 2-30%9,14,16 and malignant changes have also rarely been reported.3,12
The current case is now a nasopalatine duct cyst in a 21-year old person that the lesion is notable in terms of the age range and can be mistakenly diagnosed as a periapical lesion.
The patient was a 21- year old man, who complained of a swelling inside the mouth,facial asymmetry,numbness and looseness of the anterior teeth and referred to the Maxillofacial Radiology Department. The patient had been noticed the swelling about a year ago and he had no a complaint of pain and no a history of the trauma. In the extra-oral examination the asymmetry and swelling in the maxillary anterior region and right nasolabial fold was seen (Figure 1). Any evidence of lymphadenopathy was observed. Inflation was firm, painless, non - fluctuate and without the presence of a pulse .

Figure 1 The asymmetry and swelling in the maxillary anterior region and right nasolabial fold is seen.
In the intra-oral examination, the swelling covered with the normal mucosa was seen in the buccal vestibule of central and lateral teeth of the right incisor that was extended to the hard palate. The mesial deviation of tooth crown of the central incisor and anterior teeth mobility was observed (Figure 2). Panoramic radiography, occlusal cross-sectional of the maxillary and periapical of the maxillary anterior teeth showed a single radiolucency, unilacular, heart shaped with a well defined, regular, and cortical border in the anterior and in the midline that was approximately extended to the periapical region of the second premolar tooth on both sides. The lesion had been extended to left and right nasal cavities. In the intra-oral images lamina dura is not seen around the anterior teeth, and apex resorption of the lateral tooth root of the right incisor is evident. The central tooth of right incisor underwent the root canal therapy (RCT) (Figure 3). In computed tomography (CT) images, in axial and coronal view, a radiolucent lesion in the anterior of maxilla was seen that has caused swelling in the lateral walls of the nasal cavities and the anterior of maxillary alveolar process. Erosion is observed on the hard Palate, the floor of nasal cavity and anterior of maxilla. Nasal septum deviation to the right is evident (Figure 4).

Figure 2(A,B) the swelling covered with the normal mucosa and the mesial deviation of tooth crown of the central incisor is observed.
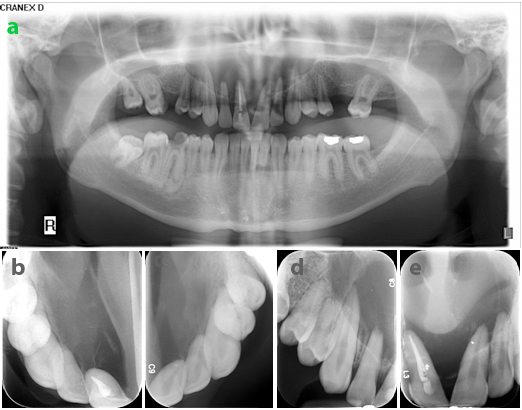
Figure 3(A,B) Panoramic radiography, occlusal cross-sectional radiographic view show a single radiolucency, unilacular, heart shaped with a well defined, regular, and cortical border that was approximately extended to the periapical region of the second premolar tooth on both sides. The lesion had been extended to left and right nasal cavities. (C,D) The lamina dura is not seen around the anterior teeth, and apex resorption of the lateral tooth root of the right incisor is evident. (White arrow).
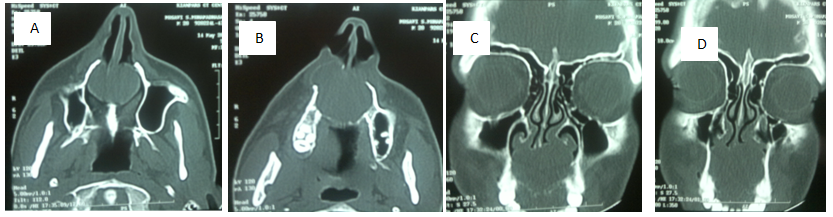
Figure 4 CT images. (A ,B) axial view shows the swelling in the lateral walls of the nasal cavities and the anterior of maxillary alveolar process. (C ,D) coronal view, erosion is observed on the hard Palate, the floor of nasal cavity and anterior of maxilla. Nasal septum deviation to the right is evident.
Based on clinical (apart from the looseness of tooth) and radiographic findings, the primary differential diagnosis included radicular cyst, nasopalatine duct cyst and central giant cell granuloma (CGCG). After performing biopsies and ultimately surgery, a histopathological examination was performed on the lesion .In a microscopic examination, cyst epithelium can be seen from stratified, squamous to simple cubic. In the lower connective wall the average Infiltrates of the chronic inflammatory cells of lymphocyte, plasma cell, and histiocyte and some acute neutrophilic inflammatory cells as well as nervous bundle sections, arteriole and vein are visible. The final diagnosis was a nasopalatine duct cyst (Figure 5).
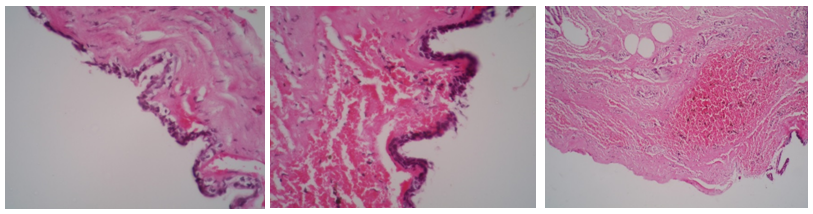
Figure 5 Microscopic examination, cyst epithelium can be seen from stratified, squamous to simple cubic. Infiltration of the chronic inflammatory cells of lymphocyte, plasma cell, and histiocyte and some acute neutrophilic inflammatory cells as well as nervous bundle sections, arteriole and vein are visible. (H&E 4x).
One year after surgery the patient referred for follow-up. Intra-oral examination showed the absence of anterior teeth looseness and mucosal anaesthesia had been removed completely. Panoramic radiography and photography were performed for patients. Panoramic radiography showed healing of the surgical area and photography of the patient's face showed a lack of asymmetry (Figure 6).
The nasopalatine duct cyst was described by Meyer for the first time in 1914.1–2 This cyst is the most common non-odontogenic developmental-evolutionary cyst of oral cavity.3 It is believed that this cyst is originated from the remains of nasopalatine duct epithelium.3,5 This cyst includes 10% of the jaw cysts4 and involves 1% of the total population.3,6 The age distribution is broad and in most cases it can be discovered in the fourth and sixth decades of life.4 ,7 The current case is a nasopalatine duct cyst in a 21-year old person that the lesion can be notable in terms of age range. Most of these cysts are asymptomatic.4,8 The most common symptom is a small swelling with well defined border in the posterior of palatal papillae.4,6–9,12 The case reported was complaining of swelling, asymmetry, numbness and the anterior teeth mobility. There was not a history of orthodontic treatment and evidence of periodontal disease as well as traumatic occlusion. Teeth looseness can be a clinical sign of malignant lesions;2 so far teeth looseness along with nasopalatine duct cyst has been reported. Hence the existence of teeth mobility along with nasopalatine duct cyst can be a rare case. Most studies showed that the nasopalatine duct cyst is radiolucency with a well defined border, rounded, oval or heart shape.4,12–14 In the examination of the current patient also there was a lesion with the same features. Considering that factors such as trauma, duct infection, and commonly spontaneous cystic degeneration have been considered as possible factors in the nasopalatine duct remains3,12 as well as a lack of history of trauma, inflammation caused by the central tooth pulp involvement of right incisor or spontaneous cystic degeneration in nasopalatine remains can be considered as possible causes. As can be seen in this report, presence of evidence of the root treatment (RCT) in cases of the presence of the nasopalatine duct cysts is common because this lesion may be commonly mistaken for pulp lesion and periapical.13 The invasive nature of these cysts should not be ignored because they can cause wide destruction.8 In the differential diagnosis of the lesion we can refer to radicular cyst,4,8,14 keratocyst odontogenic tumour (KOT),8,12 and central giant cell granuloma (CGCG).5,9,14 In terms of histopathology the epithelium of cysts is very diverse12 and includes a combination of stratified, squamous, non-keratinized epithelium, false stratified columnar epithelium, stratified columnar epithelium, and simple cubic epithelium.8,12 Microscopic examination of the current lesion is also consistent with these findings. Surgery of the lesion was performed using enucleation method.4,12
Nasopalatine duct cyst is the most common non - odontogenic,developmental - evolutionary cyst of the oral cavity3 and should be differentiated from other radiolucencies in the anterior of maxilla. The final diagnosis can be confirmed after pathological examination. Clinician’s awareness of clinical and radiographic characteristics of the nasopalatine duct cyst is important.
None.
The authors have no financial conflicts of interest to declare.
None.

©2015 Abbassi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.