Journal of
eISSN: 2373-4396


Case Report Volume 9 Issue 1
1Pauls Stradins Clinical University Hospital, Latvia
2University of Latvia, Latvia
Correspondence: Andrejs Erglis, Pauls Stradins Clinical University Hospital, Latvian Cardiology Cetnre, Pilsonu Street 12, Riga, Latvia -1002
Received: June 12, 2017 | Published: June 13, 2017
Citation: Briede I, Erglis A (2017) Vessel Restoration Therapy during Percutaneous Coronary Intervention with Bioresorbable Scaffold. J Cardiol Curr Res 9(1): 00313. DOI: 10.15406/jccr.2017.09.00313
Permanent caging of the vessel with metal is still perceived as a limitation of drug eluting stents, in that it prevents late luminal enlargement, adaptive shear stress and late expansive remodeling.1 Transient bioresorbable scaffolding prevents vessel acute closure and recoil, drug elution counteracts neointimal proliferation, and complete bioresorption after two to four years, together with vessel lumen enlargement, plaque/media reduction and vasomotion restoration, finally realises the paradigm of vascular restoration therapy.2
Keywords: percutaneous coronary intervention, bioresorbable scaffold
Bioresorbable scaffolds (BRS) are a novel approach to treat coronary artery stenosis by providing transient scaffolding and local drug delivery. The potential of this technology, such as return of vasomotion, cyclic strain, and shear stress, has been shown in some observations at up to 3years follow-up using multiple imaging modalities obtained in the ABSORB trials.3 Still the outcomes of BRS remain to be determined with respect to safety and efficacy in routine clinical practice.4
A 57-year-old man presented with stable angina grade III was admitted to hospital for elective percutaneous coronary intervention (PCI) for right coronary artery (RCA). From cardiovascular risk factors patient have non-insulin depended diabetes, arterial hypertension, dyslipidemia and previous PCI. Echocardiography revealed normal left ventricle function with no signs of valve dysfunction.
Coronary angiography revealed long, calcified > 40mm length lesion in right coronary artery proximal and middle part (Figure 1). Our decision was to treat this coronary lesion with BRS (Absorb BRS; Abbott Vascular, Santa Clara, CA, USA), following our centre plaque modification strategy, which is plaque modification before scaffold implantation using cutting or scoring balloon. In this case we used cutting balloon pre-dilatation 3.5x15mm 13 bars for each segment three times. Vessel dimensions were pre-analyzed with imaging methods to choose appropriate pre-dilatation balloon size. “PSP (Predilatation, Sizing, Post-dilatation) technique” that improves Absorb implantation is now widely described. Our centre following updated technique which is “IPSP (Imaging, Predilatation, Sizing, Postdilatation” technique. After plaque modification three BRS were implanted with total length 68mm. All scaffolds were implanted with small overlap to avoid uncovered gap which can provoke flow disturbances and possible future problems. Scaffold diameter was 3.5mm. An optimal scaffold apposition to vessel wall was achieved with non-compliant balloon 4.0x20mm. Post-dilatation was done with 15 bars in each segment. Mandatory for this intervention are imaging methods – intravascular ultrasound (IVUS) and optical coherence tomography (OCT). IVUS was performed before PCI, after plaque modification and after BRS implantation (Figure 2). OCT was performed after BRS implantation (Figure 3). Final angiography showed good result of procedure (Figure 4). Patient discharged next day on dual anti-platelet therapy for two years. Now patient reached six-month clinical follow-up with no cardiovascular events or bleeding.
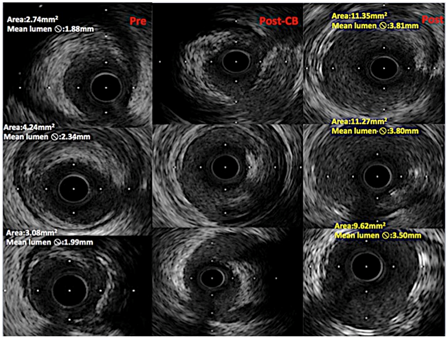
Figure 2 IVUS cross-sectional images from pre-intervention (first colon from left), after plaque modification with cutting balloon (middle colon), after scaffold implantation (left side colon). In middle colon can seen vessel lumen dissections, made by cutting balloon. Lumen changes in diameters can be seen from left to right colons.
“Real-world” BRS outcomes showed scaffold thrombosis in 1.5% of patients at 30days and 2.1% at six months were noted that exceed the incidences typically reported in contemporary all-comers registries and trials of second-generation drug eluting stents (DES).5 Our single center BRS registry data showed 0.5% scaffold thrombosis in two-year follow up for 187 patients (96% reached two-year follow-up). We strongly believe that with PCI technique, with good plaque preparation, correct vessel sizing and optimal scaffold apposition, using imaging techniques, can reach better results in terms of scaffold thrombosis.
This case report was supported in part by Latvian National Research Program "Biomedicine for Public Health" (BIOMEDICINE) and by grant from corporation „ Sistemu Inovacijas”.
None.
Erglis have received consultancy fees, research grant to the institution from Abbott Vascular, Boston Scientific, Biosensors, Cordis J&J, Medtronic.

©2017 Briede, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.