Journal of
eISSN: 2373-4396


Research Article Volume 2 Issue 1
1Nine wells Hospital and Medical School, University of Dundee, United Kingdom
2St Helens and Knowsley Teaching hospitals, United Kingdom
Correspondence: Kenneth Wong, Senior Lecturer in Cardiology (Imaging and Heart Failure) & Honorary Consultant Cardiologist, Department of Academic Cardiology, Castle Hill Hospital, Hull, United Kingdom, Tel 44-7988 796306
Received: January 08, 2015 | Published: January 14, 2015
Citation: Wong KYK, Velavan P, Wong SYS, et al. Towards understanding the clinical significance of qt peak prolongation- a novel marker of myocardial ischemia independently demonstrated in two prospective studies. J Cardiol Curr Res. 2015;2(1):9‒13. DOI: 10.15406/jccr.2015.02.00046
Background: QT peak prolongation identified patients at risk of death or non-fatal MI. We tested the hypothesis that QT peak prolongation might be associated with significant myocardial ischaemia in two separate cohorts to see how widely applicable the concept was.
Methods and Results: In the first study, 134 stroke survivors were prospectively recruited and had 12-lead ECGs and Nuclear myocardial perfusion scanning. QT peak was measured in lead I of a 12-lead ECG and heart rate corrected by Bazett’s formula (QTpc). QTpc prolongation to 360ms or more was 92% specific at diagnosing severe myocardial ischaemia. This hypothesis-generating study led us to perform a second prospective study in a different cohort of patients who were referred for dobutamine stress echocardiography. 13 of 102 patients had significant myocardial ischaemia. Significant myocardial ischaemia was associated with QT peak prolongation at rest (mean 354ms, 95% CI 341-367ms, compared with mean 332ms, 95% CI 327-337ms in those without significant ischaemia; p=0.002). QT peak prolongation to 360ms or more was 88% specific at diagnosing significant myocardial ischaemia in the stress echocardiography study. QT peak prolongation to 360ms or more was associated with over 4-fold increase odds ratio of significant myocardial ischaemia. The Mantel-Haenszel Common Odds Ratio Estimate=4.4, 95% CI=1.2-16.0, p=0.023.
Conclusion: QT peak (QTpc) prolongation to 360ms or more should make us suspect the presence of significant myocardial ischaemia. Such patients merit further investigations for potentially treatable ischaemic heart disease to reduce their risk of subsequent death or non-fatal MI.
Keywords: ischaemia, stress echocardiography, nuclear cardiology, imaging, electrocardiology
Preventing cardiac deaths remains one of the greatest challenges in medicine in the 21st Century. There is evidence to suggest QT peak prolongation identifies patients who are at risk of death or non-fatal myocardial infarction (MI).1 The next step to reduce the risk of these patients would be to find out whether there are potentially treatable conditions associated with QT peak prolongation. A potential mechanism by which QT peak prolongation might predict death or non-fatal MI might be that QT peak prolongation is associated with myocardial ischaemia. In this paper, we will test the hypothesis that QT peak prolongation is associated with myocardial ischaemia.
Study design
Patients: We aimed to test the two hypotheses by studying two cohorts of patients to see how widely applicable this concept was. The first study included only stroke survivors in a University Teaching Hospital since there is evidence to suggest stroke survivors with a long QT peak are at high risk of cardiac death.2 The second study examined patients referred for exclusion of ischaemia and viability by stress echocardiography in a District General Hospital. The studies conformed to the principles outlined in the Declaration of Helsinki. Ethics approval was obtained from the respective institutional review committees (local research ethics committees). The study also had ARSAC approval (for nuclear myocardial perfusion scanning). Written consent was obtained from all patients.
First study
Patients: We recruited 202 patients who made a good recovery and were at least one month after a recently documented CVA or TIA. The patients who had atrial fibrillation or flutter, big eminy, paced rhythm or bundle branch block on their ECG were excluded for QT interval analysis. These ECG changes would make the QT interval difficult to measure reliably. Other exclusion criteria were as follows:
Patients were also excluded from the study if they had moderate to severe asthma which contraindicated the use of dipyridamole without steroid cover. (Dipyridamole was the stressing agent for the nuclear stress scan). Moreover, patients with severe chronic obstructive pulmonary disease on theophylline medication were also excluded.
ECG: Resting supine 12-lead ECGs (Marquette Medical Systems, USA) were recorded at 25mm/second.
QT peak measurements: QT peak was defined as the onset of QRS to the peak of the T wave in lead I. The T peak was defined as the point where the T wave had the maximum amplitude. This applied to inverted T waves too. If the T wave was biphasic, then the deflection with the higher amplitude was used. However, if the upward and the downward deflection were of equal amplitude, then the measurement would be omitted. QT peak was “heart rate corrected” using Bazett’s formula
A single observer who was blinded to the nuclear myocardial perfusion study results digitized all the ECGs.
Nuclear Stress myocardial perfusion study for myocardial ischaemia: The myocardial perfusion studies were carried out using dipyridamole as the stressing agent. All theophylline medications were withheld for 36hours and caffeinated beverages for 12hours before the study. The patient was attached to a cardiac monitor before administration of dipyridamole. Dipyridamole was slowly infused at 0.56mg/kg over about 4minutes. This was followed by simple arm exercise for around 2minutes. The patient was then injected with 400MBq of 99m-Technetium tetrofosmin. This gives a radiation dose of 4 mSv /scan which is equivalent to 2years natural background and is much less than the dose received from a study using 201-Thallium.
10minutes after the injection of the radiopharmaceutical, the patient was given a small cup of water; a large cup of water was given 10minutes prior to the start of imaging. This was to try to reduce the activity in the stomach and small bowel which might interfere with the reconstruction of the tomographic images. At 45minutes post injection a 180 degree tomographic acquisition was begun acquiring data from right anterior oblique to left posterior oblique using a dual head Philips Axis gamma camera fitted with high resolution collimators. The system was also fitted with a Beacon attenuation correction system. If the stress scan was abnormal, images obtained after an injection at rest, approximately 1week later, were used to differentiate between infarction and ischaemia.
The scans were assessed quantitatively. Each scan was scored out of 64, by dividing the left ventricle into 16 regions (4 apical, 3 anterior, 3 lateral, 3 inferior, and 3 septal) and giving each region a score out of 4, indicating the degree of perfusion. The inducible ischaemia score was defined as the difference between the score obtained from the stress scan and that of the rest scan (i.e. Rest scan score-stress scan score). An inducible ischaemia score of greater than or equal to 12 was regarded as evidence of severe myocardial ischaemia.
Second study
166 consecutive consenting patients referred for stress echocardiography for exclusion of ischaemia/viability were recruited.
Resting ECG: Resting 12-lead ECGs were again recorded at 25mm/second, with the subject lying supine.
QT peak measurements: The definition of QT peak was as discussed above (same as First Study). QTpc was measured by a single observer (with ruler and callipers), again blinded to the clinical features of the patients as well as the outcome of the stress test.
Echocardiography
In all cases, transthoracic echocardiography was undertaken using the GE Vingmed System Five (General Electric Company, USA).
Stress Echocardiography
Resting images were first recorded in four standard views-para sternal long axis, para sternal short axis, apical 4 chamber and apical 2 chamber views (PLX, PSX, AP4C and AP2C). Then IV Dobutamine infusion was started at 5 mcg/kg/min and the dose was increased every 3 minutes (to 10, 20, 30 and 40mcg/kg/min). If the patient’s heart rate failed to increase adequately [i.e. to at least 85% maximum age predicted heart rate (220 minus age)], then Atropine IV was administered at a dose of 0.3 to 0.6mg. All four views were recorded during the study at each stage (resting, low dose, intermediate and peak dose) after myocardial border enhancement with administration of 0.5 ml IV contrast agent [Sonovue® or Optison®] just prior to recording. The images were then analysed using the Echopac® software (General Electric Company, USA).
In the stress echocardiography study, the cut-off for significant ischaemia was defined as a difference of 0.18 or more between the Wall Motion Score Index during stress compared with that at rest. This would be compatible with disease in all 3 coronary artery territories or significant disease in at least 1 territory.
Statistical methods
SPSS was used for statistical analysis: In the Nuclear myocardial perfusion study on stroke survivors, Spearman Non-parametric tests were used to test the relationship between QTpc and the inducible ischaemia score (rest score-stress score). UNIANOVA was used to assess if there was a significant difference in QT peak and between patients who did and those who did not have myocardial ischaemia respectively, provided that the residuals were normally distributed (i.e. one-way Kolmogorov-Smirnov test 2-tailed p > 0.05). A p value of < 0.05 was regarded as statistically significant.
ROC curves enabled us to determine sensitivity and specificity of different cut-off values of QT peak at diagnosing the presence of myocardial ischaemia. In the Stress Echocardiography study, UNIANOVA was employed where appropriate (i.e. if residuals of QT peak were normally distributed) to test the hypothesis generated by the study on stroke survivors. Again, ROC curves helped determine sensitivity and specificity of QT peak at diagnosing myocardial ischaemia. By cross-tabulating the presence of significant myocardial ischaemia with the cut-off value of QTpc suggested by the first study, we were able to perform Chi-square and correlation testing. A Fisher’s Exact test 2-tailed p < 0.05 would be regarded as statistically significant. Further, the Mantel-Haenszel common odds ratio was also computed to help us quantify the odds ratio estimate (with 95% confidence intervals).
Nuclear myocardial perfusion Study Results
Baseline characteristics of the patients are summarised in (Table 1).
|
Nuclear |
Stress Echocardiography Cohort |
Age |
66 ± 9.4 |
57 ± 10.7 |
Sex, % female |
40 |
52 |
Systolic blood pressure (BP), mmHg |
144 ± 21.2 |
152 ± 24.5 |
Diastolic BP, mmHg |
80 ± 11.0 |
89 ± 13.5 |
Total cholesterol, mmol/L |
4.9 ± 0.91 |
5.3 ± 1.29 |
HDL cholesterol, mmol/L |
1.3 ± 0.41 |
1.3 ± 0.55 |
Glucose, mmol/L |
6.2 ± 2.60 |
5.6 ± 1.14 |
% diabetic |
12 |
11 |
Smoking habit, % current (or ex-smokers) |
23 (51) |
20 (34) |
QT peak (QTpc), ms |
325 ± 23.2 |
337 ± 29.5 |
Table 1 Patient characteristics
Data given are means ± SD
QTpc and myocardial ischaemia
QTpc correlated very weakly with inducible ischaemia on dipyridamole myocardial perfusion scan. (Spearman r=0.2, 2-tailed p =0.041). N=134. Severe myocardial ischaemia (inducible ischaemia score 12 or more) was found in 4 patients. The mean QTpc of these patients with severe myocardial ischaemia was 354 (95% CI=331-377ms), compared with 325ms (95% CI 321-329ms) in those patients with lesser degrees of ischaemia or no ischaemia. (p=0.016). Figure 1 showed QTpc prolongation to 360ms or more had 92% specificity at diagnosing severe myocardial ischaemia.
|
Cut-off value of QTpc I (ms) |
|
Sensitivity (%) |
|
Specificity (%) |
|
320 |
|
100 |
|
45 |
|
350 |
|
75 |
|
85 |
|
360 |
|
50 |
|
92 |
|
Cut-off value of QTpc I (ms) |
Sensitivity (%) |
Specificity (%) |
|
320 |
100 |
34 |
|
350 |
54 |
78 |
|
360 |
39 |
88 |
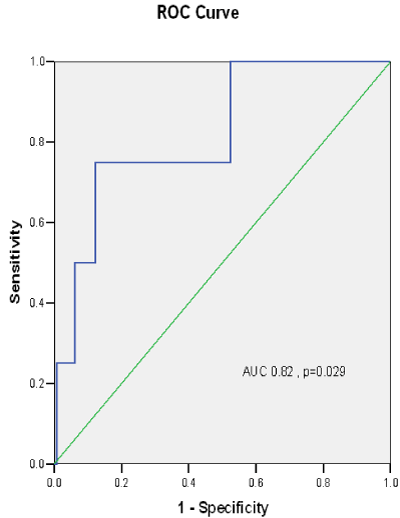
Figure 1 ROC curve demonstrating the sensitivities and specificities of different cut-off values of heart rate corrected QT peak (QTpc) at predicting severe myocardial ischaemia on nuclear scan in stroke survivors.
Reliability test
Covariance matrix was used for analysis of reliability or intra observer reproducibility of QTpc measurements (N=12). Alpha was 0.97, indicating highly reproducible results. Further, inter-observer reproducibility was tested in 17 cases, yielding an alpha of 0.94 (digitizing method).
Results of the stress echocardiography study
Patients: 166 patients were referred for stress echocardiography to exclude myocardial ischaemia/viability. 14% had a history of MI. The patient characteristics are summarised in (Table 1).
Significant myocardial ischaemia demonstrated on stress echocardiography was associated with QT peak prolongation at rest
QTpc was measured in 102 patients with research-quality stress echocardiography. Of these, 13 had significant myocardial ischaemia. Significant myocardial ischaemia was associated with QT peak prolongation at rest (mean 354ms, 95% CI 341-367ms, compared with mean 332ms, 95% CI 327-337ms in those without significant ischaemia; p=0.002). Figure 2 QT peak prolongation to 360ms or more was 88% specific at diagnosing significant myocardial ischaemia in the stress echocardiography study. Figure 3 QT peak prolongation to 360ms or more was associated with over 4-fold increase in the odds ratio of significant myocardial ischaemia. The Mantel-Haenszel Common Odds Ratio Estimate=4.4, 95% CI=1.2-16.0, p=0.023.
We have shown the value of using QT peak prolongation as a marker of significant myocardial ischaemia in two independent cohorts of patients. This might explain why patients with QT peak prolongation are at higher risk of death or non-fatal MI.1
Choice of cut-off value of abnormal QT peak
If QTpc was prolonged to 360ms or more in stroke survivors, the specificity at diagnosing severe myocardial ischaemia was 92%. This cut-off value (360ms) was chosen to be validated in the second study. It can be argued that a lower cut-off value might be chosen to increase the sensitivity of the disease marker. For instance, 320ms had 100% sensitivity in both studies. Nevertheless, it should be noted that lesser degrees of ischaemia might be missed. QT peak prolongation to 360ms or above was associated with a several fold increase in the odds ratio of significant myocardial ischaemia in our stress echocardiography study. This finding may explain why QTpc of 360ms or above predicted cardiac death within 5years of a stroke with a specificity of 76%.2
Possible mechanism
In 1999, Festa reported the relationship of heart rate corrected QT interval with subclinical atherosclerosis, as determined by carotid intima media thickness, in non-diabetic subjects in the Insulin Resistance Atherosclerosis Study.3 Intima media thickness of the common carotid artery was measured by ultrasound and correlated significantly albeit weakly with QTc. This study raised the suspicion that the QT interval may serve as a marker for silent or subclinical i.e. clinically undetected atherosclerotic disease. More recently, an elegant study published electronically 2 months ago demonstrated how controlled (1 minute) occlusion of the left coronary artery led to QT prolongation. The authors observed the phenomenon that QT prolongation was inversely related to collateral function.4 This might suggest a protective mechanism of human coronary collaterals against cardiac death. On the other hand, intriguingly, a small study of 68 patients who underwent CABG had longer QT intervals and QT peak intervals (QT/RR slope) after revascularization.5
Why QT peak?
QT is traditionally defined as the interval between the start of the QRS complex and the end of the T wave. In measuring a QT interval, the beginning of the Q wave is usually identifiable. On the other hand, the end of the T wave is not always easily identifiable. This is because commonly, the T wave is flat. A flat T wave is seen normally in lead V1 as well as in certain pathological conditions such as myocardial ischaemia or hypocalcaemia. If the patient’s potassium is less than 2.7, a U wave occurring after the T wave may exceed the T wave amplitude in the same lead.6 The U wave adds to the difficulty in deciding where the T wave ends. This has led to a number of different definitions of T wave measurement, which inevitably causes a degree of confusion. Thus, the end of the T-wave has been variously defined as the point at the return of the T-wave to the isoelectric line, or at the nadir between the T- and the U-waves, or at the intersection of an extrapolated line of the downward slope to the isoelectric line. The former two T-wave end definitions are most commonly used in practice.
An attractive alternative way to obviate the confusion engendered by the difficulties in defining the end of the T wave is to measure the Q-T peak which is defined as the interval between the onset of the QRS complex and the peak of the T wave. Clearly, the start of the Q wave and the peak of the T wave are nearly always easily identifiable. Another reason why the use of QT peak measurements may be superior to the more commonly used QT end measurement is that some would argue that the onset of repolarisation is nearer to the T-wave peak.7 There is some evidence to suggest that QT peak dispersion (maximum minus minimum QT peak), but not QT end dispersion, was longer in patients with myocardial ischaemia.8 Measuring QT peak from all 12 leads of the ECG undoubtedly poses practical difficulties for the busy clinician. In the present paper, we have reported in two cohorts of patients that QT peak measured from a single lead of the ECG was associated with ischaemic heart disease.
Clinical Implications
QT peak prolongation at rest identifies myocardial ischaemia, and may be used to risk-stratify patients for stress echocardiography or other non-invasive test for ischaemia. To expedite care of patients with suspected ischaemia who could not undergo treadmill testing for a variety of reasons e.g. walking with a stick, they should be triaged urgently for other non-invasive tests, especially if the patient has QTpc of 360ms or longer. If such non-invasive tests are not available in a timely fashion, coronary angiography should seriously be considered, as QTpc of 360ms or longer might indicate severe myocardial ischaemia in one territory or significant myocardial ischaemia in all 3coronary artery territories. These patients might benefit prognostically from coronary artery revascularisation. In the meantime, aspirin, high-dose statin, and beta-blocker therapy should be considered as part of the overall cardiovascular risk assessment and anti-ischaemic therapy.
We have examined the value of QT peak as a marker of myocardial ischaemia in two different cohorts of patients to test how widely applicable the hypotheses were. Whilst this could be regarded as strength of the study, we would like to emphasize the fact that the present study should not be regarded as a “derivation-validation” study in the strictest sense. There are significant differences in the two studies. The first study recruited only stroke survivors, many of whom did not have symptoms or past history of ischaemic heart disease. The second study investigated patients who were referred for stress echocardiography for exclusion of ischaemia/viability. Very few patients had severe myocardial ischaemia in the first hypothesis-generating study on stroke survivors whilst in the second study, 13% of the patients had significant myocardial ischaemia. The first study took place in a University Teaching Hospital and the second study was performed in a district general hospital. The first study used nuclear scans with dipyridamole as stressor to rule out ischaemia whilst the second study used dobutamine stress echocardiography.
It can be argued that the use of 16 segment models might underestimate the degree of myocardial ischaemia from the true apex of the heart. i.e. 4 instead of 5 apical areas were interrogated. No anatomical data was obtained from cardiac catheterisation as part of the research studies.
Non-invasive coronary angiography using 320-row CT has now been shown to accurately diagnose significant coronary stenoses with near 100% sensitivity and > 90% specificity. These advanced scanners can now obtain all the necessary information in < 0.4 second, capturing up to 16cm of information, i.e. the whole heart, and therefore avoid over-scanning and over-ranging. This remarkable technological advance meant the radiation exposure of 320-row CT is now less than that of conventional cardiac catheterization.9 It would be of interest to see if QT peak prolongation might be associated with significant stenoses on CT coronary angiography.
QT peak (QTpc) prolongation to 360ms or more should make us suspect the presence of significant myocardial ischaemia. Such patients merit further investigations for potentially treatable ischaemic heart disease to reduce their risk of subsequent death or non-fatal MI.
None.
None.
British Heart Foundation.

©2015 Wong, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.