Journal of
eISSN: 2373-4396


Research Article Volume 1 Issue 6
1Cardiology department, Benha University, Egypt
2National Heart Institute, Cairo, Egypt
Correspondence: Hesham Khalid Rashid Mousa, Cardiology Department, Benha University, Egypt, Tel 201014977666
Received: November 13, 2014 | Published: November 28, 2014
Citation: Rashid H, El-Enien HA, Ibraheem M. The predictive value of tissue Doppler for left ventricular recovery and remodeling after primary percutaneous coronary intervention. J Cardiol Curr Res. 2014;1(6):159-164. DOI: 10.15406/jccr.2014.01.00032
Background: The main goal in the management of ST segment elevation myocardial infarction (STEMI) is an early restoration of coronary artery flow in order to preserve viable myocardium. Doppler tissue imaging (DTI) is a simple modality that measures tissue velocity during cardiac cycle.
Objective: To assess the role of DTIine valuation of LV recovery after PCI.
Methods: Fifty patients were included in this study with STEMI, and were candidate for primary PCI. Cardiac enzymes and ECG were done during admission and 12 hours after PCI for assessment of noninvasive criteria for reperfusion. Echocardiography with DTI was performed for all patients to assess LV recovery and remodeling at baseline and one month after PCI. Primary PCI was performed and patients were divided into two groups: Group A with good reperfusion, and group B with poor reperfusion.
Results: In patients of group A (78%), there was a statistically significant improvement of the LV EF more than 5% one month after primary PCI (LV recovery) (p<0.001), while in group B, there was a statistically significant increase in LVED volume more than 20% (LV remodeling) (P<0.01). The mean systolic (S) velocity showed a cutoff value of 4.83cm/sec or more for prediction of recovery of global systolic function with a sensitivity and specificity of 100% and 90% respectively. Out of 11 patients in group B, 3 patients (27.27%) developed MACE and admitted to CCU, 2 of them with heart failure, while other one needed revascularization.
Conclusion: LV recovery occurs in STEMI patients treated with primary PCI and it is an important for favorable outcome.
Keywords: LV remodeling after primary PCI, tissue doppler imaging, myocardial infarction, preservation of left ventricular
Áa, late diastolic velocity; Éa, early diastolic velocity; Š, main positive systolic velocity; PTCA, percutaneous transluminal coronary angiography; PW-DTI, pulsed wave doppler tissue imaging; MBG, myocardial brush grade; MACE, major advanced cardiac events
The main goal in the management of acute myocardial infarction (AMI) is an early restoration of coronary artery flow in order to preserve viable myocardium. Primary percutaneous coronary intervention (PCI) has proven to be superior to other reperfusion strategies in terms of mortality reduction and preservation of left ventricular (LV) function.1 Despite improvements in the treatment of MI, 30% of patients show LV remodeling post-MI, moreover, it is expected that almost 30% will have an LV ejection fraction (LVEF) below 40% at 6 months post-MI.2 Doppler tissue imaging is a modality developed in last years that measures tissue velocity during cardiac cycle. It has been previously demonstrated that there is a significant relationship between successful reperfusion after thrombolytic therapy in acute myocardial infarction as indicated by the conventional noninvasive reperfusion criteria and pulsed wave tissue Doppler (PTD) parameters.3 The study aimed to assess the role of pulsed wave tissue Doppler in evaluation of left ventricular recovery and remodeling after primary PCI in relation to other invasive and non invasive reperfusion criteria.
The study included 50 consecutive patients selected randomly and admitted at CCU of Benha University Hospital and National Heart Institute by acute ST–elevated myocardial infarction and were candidate for PCI. Patients with past history of IHD, patients received thrombolytic therapy, patients with valvular disease, cardiomyopathy, significant left ventricular hypertrophy, pericardial disease, or patients with abnormal ECG as, BBB, pre-excitation, AF, atrial flutter, or complete AV block, or patients underwent coronary artery bypass surgery were excluded from the study.
Study design: All patients were subjected to the following:
Informed consent from all participants was obtained. Full history taking with especial attention on the risk factors e.g., age, gender, smoking, presence of Diabetes Mellitus, dyslipidaemia, hypertension, family history of IHD, and previous myocardial infarctions.
Full clinical examination
Electrocardiographic analysis: serial S-T segment analysis before and at the end of the coronary intervention was done by one observer blinded to clinical data. The sum of S-T segment elevations was measured manually 20 milliseconds after the end of the QRS complex. Adequate resolution of S-T segment elevation after successful re-canalization was expressed as a percentage of the initial S-T segment elevation. S-T segment resolution<50% was defined as a marker of impaired microvascular reperfusion. On the other hand, S-T segment resolution greater than 50% indicated good myocardial reperfusion.4
Biochemical markers: creatine phosphokinase (CK)-MB and total CK were done as biochemical markers of myocardial reperfusion every 6 hours for 24 hours, then daily after PCI. Serum CK peaking within the first 12 hours of PCI was considered a noninvasive marker of reperfusion.5
Routine laboratory investigations: Including CBC, liver functions, kidney functions and coagulation profile were done for each patient during hospitalization.
Coronary intervention
a) All patients received 600 mg loading dose of clopidogrel before PCI.
b) After informed consent, Coronary angiography (trans-femoral approach) was performed as soon as possible starting by catheterization of the artery of the non-infarct region, followed by the culprit one. PTCA±stenting of the culprit lesion(s) was done with 10,000 units of heparin (UFH) given intravenously just prior to the intervention.
c) The decision to use glycoprotein IIb/IIIa receptor inhibitors was taken when indicated.
Invasive reperfusion criteria: Gibson et al.6
TIMI flow grades (TFGs): It is an angiographic marker for successful reperfusion. Myocardial perfusion was described using myocardial blush grades (MBG). Patients with MBG 0 or 1 indicate poor reperfusion while patients with MBG 2 or 3, were considered to be angiography successfully re-perfused.7 TIMI flow and MBG were visually assessed on the angiogram and described immediately after the primary PCI by the performing cardiologist. According to the non-invasive reperfusion criteria (ECG analysis and cardiac markers) and the invasive reperfusion criteria (TIMI flow grades and MBG), all patients were divided into two groups:
Echocardiography and Pulsed tissue Doppler examination
All patients were evaluated using Philips echocardiography machines within 2 days of AMI, and one month later using the same protocol and all parameters were blinded to the results of the primary PCI.
Follow up the patients
All patients discharged after PCI with the same anti-ischemic drugs, ACEI, beta blocker and regularly observed at outpatient clinic and contacted with his family by telephone for development of any major adverse cardiac events (MACE) as recurrent chest pain, needs for hospitalization, or reperfusion and lastly for death.
All data analyses were performed with software (Statistical Package for Social Sciences SPSS for Windows 12.0, SPSS Inc, and Chicago IL). Continuous variables between groups were compared by the Student test. The correlation between changes in systolic PTD parameters and global EF were calculated using Pearson’s correlation coefficient. Receiver operating characteristic curves were constructed to detect the best cut-off value for a change in mean S-wave velocity to detect LV functional recovery. The sensitivities, specificities, and positive and negative predictive values for the various markers of reperfusion in detecting LV functional recovery were calculated. A probability value (P-value<0.05), (2-tailed) was considered significant results are expressed as mean±SD, unless otherwise specified.9
Patients enrolled in this study were divided into two groups:
Demographic data of the studied groups (Table 1) There was no significant difference between the two groups as regard age distribution. The Mean age ±SD was 50.4±9.8years in group A and 51.7±14.2years in group B (P >0.05), out of thirty nine patients within group A, twenty five patients (64.1%) were males and fourteen patients (35.9%) were females versus three males (27.2%) and eight females (72.7%) in group B with a significant difference between the studied groups. Clinical examination, history taking and laboratory investigations revealed that presence of risk factors of CAD has been almost a constant finding in all patients. There is significant higher incidence of DM (100%), HTN (72.7%), and positive family history of CAD (72.7%) in group B compared to group A (p value<0.05). Coronary Angiography and Primary PCI Data (Table 2) Fifty percent of patients were presented with anterior MI, while the other fifty were diagnosed as inferior MI. Fifty percent of patients had LAD lesion, while the RCA was occluded in38% of patients and the LCX was the culprit in 12%of patients with no significant difference between both groups as regard distribution of the culprit vessel. Fourteen patients (35.9%) in group A had single vessel disease versus 5 patients (45.46%) in group B, also 14 patients (35.9%) in group A had 2-vessel disease versus 4 patients (36.36%) in group B, and only 11 patients (28.28%) in group A had 3-vessel disease versus two patients in group B.
|
Group A |
Group B |
P value |
|
|
N=39 |
N=11 |
||
|
Mean Age ±SD |
50.4±9.8 |
51.7±14.2 |
>0.05 |
|
Female |
14(35.9%) |
8(72.7%) |
<0.05* |
|
Male |
25(64.1%) |
3(27.3%) |
|
|
DM |
19 (48.72%) |
11 (100 %) |
<0.001* |
|
HTN |
19 (48.72%) |
8 (72.73 %) |
<0.05* |
|
dyslipidemia |
23 (58.97%) |
6 (54.55 %) |
>0.05 |
|
Smoking |
14 (35.90%) |
2 (18.18 %) |
>0.05 |
|
Family history |
15 (38.46%) |
8 (72.73%) |
<0.05* |
Table 1 Demographic data among the studied groups
|
Group A |
Group B |
Chi-Square |
|||
|
N=39 (78%) |
N=11 (22%) |
X2 |
P-value |
||
|
Culprit vessel |
LAD |
20 (51.28) |
5 (45.45) |
3.972 |
0.137 |
|
LCX |
6 (15.38) |
0 (00) |
|||
|
RCA |
13 (33.33) |
6 (54.55) |
|||
|
Number of diseased vessels |
1-vesseles |
14 (35.90) |
5(45.46) |
0.558 |
0.756 |
|
2-vesseles |
14 (35.90) |
4 (36.36) |
|||
|
3-vesseles |
11 (28.20) |
2 (18.18) |
|||
|
Type of stent |
Bare metal |
28 (71.79) |
10 (90.9) |
2.005 |
0.157 |
|
Drug-eluting |
11 (28.21) |
1 (9.1) |
|||
|
TIMI flow grade |
Grade 0 |
0 (00) |
3 (27.27) |
52.69 |
<0.001* |
|
Grade 1 |
0 (00) |
4 (36.36) |
|||
|
Grade 2 |
0 (00) |
4 (36.36) |
|||
|
Grade 3 |
39 (100) |
0 (00) |
|||
|
Myocardial blush grade |
Grade 2=19 (48.7) |
Grade 0=5 (45.5) |
|||
|
Grade 3= 20 (51.3) |
Grade 1=6 (54.5) |
||||
Table 2 Coronary angiography and PCI data of both groups
PCI with stent of culprit vessel was achieved in all patients. Bare metal stents were more commonly (76%) deployed at the culprit lesion than drug-eluting stents (24%), and more commonly used in group B (90.9%) than in group A (71.7%). All patients in group A were successfully re-perfused at the tissue level achieving MBG 2 (48.72%) and MBG 3(51.28%), while no patients in group B achieved successful reperfusion (MBG 0 in 45.45% of group B patients and MBG 1 in 54.55% of patients). All patients in group A were successfully re-canalized achieving TIMI 3 flow grade(about 78% of entire study group of patients) while no patients in group B achieved it. The predictors of failure re-canalization were, DM, HTN, and patients had positive family history of CAD.
Standard echocardiography: i. In patients with group A (78%), there was a statistically significant improvement of LV EF more than 5% (recovery), it was (46.8±6.3) at baseline and became (59.3±6.2) one month after PCI (p<0.001), and this is reflected on significant improvement of resting wall motion score index after one month follow up (p<0.05).
Tissue Doppler data: Both systolic and diastolic PTD parameters were recorded from 6 sectors (anterior, inferior, anteroseptum, inferoseptum, posterior and lateral walls).
Detection of LV functional recovery
In comparison between group A and group B using the mean systolic (S) velocity showed a cutoff value of 4.83cm/sec or more for prediction of recovery of global systolic function with a sensitivity and specificity of 100% and 90% respectively while the positive predictive value, negative predictive value and accuracy were 97.5%, 100%and 0.986 respectively (Figure 1). When we comparison between group A and group B using the mean Ea as a parameter of diastolic function of the pulsed wave tissue Doppler showed a cutoff value of 5.38cm/sec or more for prediction of recovery of diastolic function after myocardial infarction treated with 1ry PCI with a sensitivity and specificity of 97.4 %and 100%respectively while the positive predictive value, negative predictive value and accuracy were 97.5%, 100%and 0.986 respectively (Figure 2).
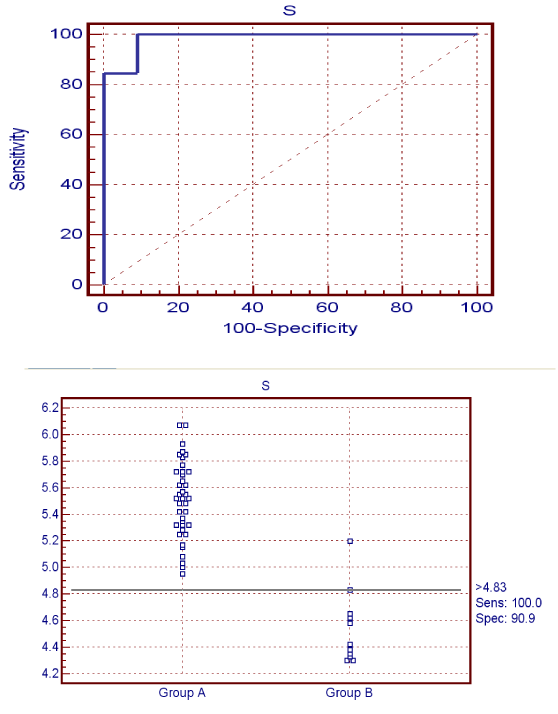
Figure 1 The sensitivity and specificity of S wave for detection of recovery of LV systolic function.
PTD measurements and global LV function
In patients of group A (78%), the mean LV EF increased from 46.8±6.3% at baseline to 59.3±6.2% after PCI (P <0.001), while in group B, the mean LV EF of this group increased from 37.3±3.5 at baseline to 39.2±3.4(mean 1.909%) which is less than 5% (the cutoff value for prediction LV functional recovery). The mean value of S-wave velocity in group A, showed significant improvement, that increased from 5.5±0.28 at baseline study to 9.9±0.72cm/s one month after PCI (p<0.001), but it was insignificant in group B (p>0.05). The change in mean S-wave velocity before and after PCI was correlated with the change in global systolic function (r=0.003, P-value=0.034) (Figure 3) (Table 3).
|
Group A |
P value |
Group B |
P value |
||||
|
Baseline |
Follow up (2nd ) |
Baseline |
Follow up |
||||
|
(1st) |
(1st ) |
(2nd) |
|||||
|
RWM sore index |
3.4±0.7 |
2.3±0.6 |
<0.05* |
4±0.44 |
3.7±0.46 |
>0.05 |
|
|
LVES volume |
67.4±8.3 |
63.9±8.9 |
<0.01* |
76.7±9.7 |
80±9.1 |
>0.05 |
|
|
LVED volume |
159.5±118 |
159.5±11.2 |
>0.05 |
165.4±15.6 |
195.4±16.3 |
<0.01* |
|
|
LVES diameter |
40.5±15.4 |
42.8±10.3 |
>0.05 |
45.6±5 |
48±5.2 |
>0.05 |
|
|
LVED |
5.2±0.5 |
5.2±0.47 |
>0.05 |
50.2±0.5 |
65±0.48 |
<0.05* |
|
|
diameter (mm ) |
|||||||
|
EF% |
46.8±6.3 |
59.3±6.2 |
<0.001* |
37.3±3.5 |
39.2±3.4 |
>0.05 |
|
|
TDI |
S wave |
5.5±0.28 |
9.9±0.7 |
<0.01* |
4.5±0.27 |
4.05±0.27 |
>0.05 |
|
Ea wave |
6.3±0.64 |
10.7±0.83 |
<0.01* |
5.53±0.67 |
3.61±0.69 |
<0.05* |
|
|
Aa wave |
6.7±0.71 |
6.8±0.65 |
>0.05 |
8.2±0.50 |
8.2±0.48 |
>0.05 |
|
|
E/A ratio |
0.94±0.3 |
1.5±0.4 |
<0.01* |
0.67±0.3 |
0.43±0.2 |
>0.05 |
|
Table 3 comparisons between the baseline and follow up Echocardiography data of the studied groups
Follow up the patients for major adverse cardiac events
We found that, out of 11 patients in group B, 2 patients developed heart failure and required CCU admission, and one patient needed coronary revascularization with total MACE (27.27%).
The relationship between PTD parameters and noninvasive reperfusion criteria has been previously reported in patients who received thrombolytic therapy and thus, invasive markers of reperfusion were not evaluated.3 The success of reperfusion in the patients enrolled in our study was examined by a variety of invasive (TIMI flow grade and myocardial blush grade) and noninvasive (ST-segment resolution and early peaking of cardiac biomarkers) markers. Of these, MBG and S-T segment resolution were specifically targeted, as these parameters also provide information about myocardial perfusion.10 We recorded systolic and diastolic PW-TDI parameters at the level of the mitral annulus, evaluating the longitudinal shortening of the LV within 48 hours as baseline and one month later as a follow up study. As the LV contracts, shortening occurs along both the long and the short axis. Shortening across the LV long axis can be used in the evaluation of regional and global LV functions.11 In our study, patients with greater than 50% ST resolution showed significant improvement of systolic PTD parameters in the infarct-related and non–infarct related walls between the first and second PTD evaluation, whereas those with 50% or less S-T resolution showed significant deterioration in the systolic S wave values at all examined walls both at the baseline and follow up evaluation. Because of failure of micro-vascular reperfusion in these patients, they possibly demonstrate a larger infarct size, resulting in functional deterioration of systolic motion in the infarct-related segments. Similarly, patients with an early CK peak showed significant improvement of systolic PTD parameters and those with a delayed CK peak showed significant deterioration in the infarct-related walls.
In the present study, the mean, systolic (S) velocity showed a cutoff value of 4.83cm/sec or more for prediction of recovery of global systolic function with a sensitivity and specificity of 100% and 90% respectively, while the mean Ea showed a cutoff value of 5.38cm/sec or more for prediction of recovery of diastolic function after myocardial infarction treated with 1ry PCI with a sensitivity and specificity of 97.4 % and 100% respectively. These simple noninvasive tools could play an important role in detecting the success of micro-vascular reperfusion through the changes detected in regional myocardial function after acute MI. In our study, all patients of studied group had diastolic dysfunction before PCI, that originated primarily from reduction of the Ea wave without change in Aa wave, because E-wave represents the energy dependant rapid filling phase and A-wave the atrial contraction dependent passive filling phase, it is not surprising that only E-wave peak levels are reduced.12 During acute ischemia, in order to protect LV filling against sudden reduction in LV compliance, A-wave peak levels can increase, which shows increased atrial contribution to ventricular filling. On the other hand, Alam et al.11 did not observe significant changes in A-wave peak levels 2 to 4 days after AMI compared with controls, which parallel to our finding.
Bach et al.13 Observed impairment of diastolic functions while systolic functions were preserved in the first 2 second after inflation of the balloon, although there was no significant (50%) stenosis in remote myocardial segments, they concluded that, diastolic function is much more sensitive to ischemia than systolic function. In our study, EF was significantly higher in patients with good reperfusion criteria the mean LV EF of the group A increased from 46.8±6.38% before PCI to 59.3±6.2% after PCI (P<0.001). Although we have measured LVEF only 48 hours after the acute MI, such large-scale studied as TEAM or GUSTO have not found significant changes in LVEF in the period between 90 minutes and 1-to 2-week after AMI.14 In this study we found that, a significant positive correlation between LVEF and the average of systolic velocity measured from six different mitral annular locations (r=0.300, p-value 0.034). The average of systolic mitral annular velocity measured from six locations 4.83cm/sec, can be used for prediction of recovery (increase of LVEF≥5% between baseline and follow up) of global systolic function with a sensitivity and specificity of 100%and 90% respectively while the positive predictive value, negative predictive value and accuracy were 97.5%, 100%and 0.986 respectively.
In a cross-sectional setting, positive correlations have been found between systolic myocardial velocities and LVEF. For example, Gulati et al.15 showed in a population with various underlying cardiac diseases that pulsed wave derived peak systolic velocity, measured as an average from six sites at the level of the mitral annulus correlated well (r¼ 0.85) with LVEF. However, no studies have investigated whether myocardial and/or annular velocities are related to LVEF at a time point when LVEF is generally accepted to have stabilized.16 In our study we found that, the predictors of LV function recovery after PCI were, LVEF>45%, LVES volume<68 ml, and S wave>5.5 cm/sec. in baseline echocardiography. In a study of Joost et al.17 in which they aimed to detect if TDI can predict LV function recovery ,infarct size and remodeling as measured by MRI at 4 months, they used the screening ability of S wave to identify patients with LVEF greater or less than 40% (area under the curve 0.79; P¼ 0.009). Although numbers were low for patients with poor LVEF, S velocity≤3.0cm/s appeared to be an excellent predictor to identify post-MI patients with LVEF≤40% (PPV 100%), while S wave 6.5cm/s or more excellent to identify post-MI patients with LVEF≥40% with sensitivity 62%, whereas the specificity was 78%. Park et al.18 found that, 46% of patients showed remodeling, in contrast to 18% of the patients in Joost et al.17 study, while in our study LV remodeling was detected in 22% of patients who had failed to show significant invasive and non–invasive reperfusion. This difference can be explained by the difference in percentage of anterior infarctions included (100% vs. 52%, vs 50% respectively). Infarct size on contrast MRI may be superior to LVEF and LV volumes for predicting long-term mortality in patients with MI Roes et al.19 they established a firm inverse relationship between S and the extent of myocardial necrosis at 4 months, even with same age and sex. We found that, out of 11 patients, three patients (27.27%) in group B were developed MACE, 2 of them admitted to CCU by heart failure while the other one need for revascularization due to recurrent chest pain.
LV recovery occurs in STEMI patients treated with primary PCI and it is an important for favorable outcome and can be estimated by TDI.
None.
Authors declare that there is no conflict of interest.

©2014 Rashid, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.