Journal of
eISSN: 2373-4396


Case Report Volume 15 Issue 5
1Department of Neurology, Santa Casa da Misericórdia de Goiânia, Brazil
2Department of Neurology, Hospital de Urgências de Goiânia – HUGO, Brazil
3Department of Neurology, Alberto Rossi State Hospital, Brazil
Correspondence: Pinheiro SR, Department of Neurology, Alberto Rossi State Hospital, Brazil, Tel (64) 36241-404
Received: November 18, 2022 | Published: November 30, 2022
Citation: Pinheiro SR, MachadoOV, Damasceno E, et al. Spontaneous anterior spinal cord syndrome and pulmonary thromboembolism - the first manifestation of a hematologic disease: a case report. J Cardiol Curr Res. 2022;15(5):121-122. DOI: 10.15406/jccr.2022.15.00566
A healthy 32-year-old man presented with bilateral dorsalis at the scapular level upon arising in the morning, sudden onset, intense and brief, rapidly evolving into an occipital headache, the worst pain of his life, approximately 30 minutes later evolving with paraparesis and paraplegia. Besides the acute paraplegia, the patient presented involuntary, refractory and persistent priapism. Bladder retention requiring the use of urinary catheterization and fecal retention. However, there was no report of current illicit substance use, and he reported previous recreational use of marijuana and cocaine. On admission physical examination, there was no change in skin color, arterial pulses, and lower limb trophism; motricity was grade 0 in the left lower limb and grade 1 in the right lower limb. He presented loss of thermal and pain sensitivity at the T2 sensory level, and bilateral Babinski reflex. An indwelling urinary catheter was used due to urinary problems, and he persisted with involuntary priapism for five days after hospitalization. Computed tomography angiotomography (CTA) scans of the abdomen and neck were normal. Chest angiotomography showed minimal filling failure in the right lower lateral inferior segmental and sub segmental artery, consistent with acute pulmonary thromboembolism (PTE). General laboratory tests and cerebrospinal fluid, were normal. Magnetic resonance imaging (MRI) of the spinal cord showed ischemia of the anterior spinal artery beginning at C7 - T8. They found no arteriovenous malformations or aneurysms. Thrombophilia screening showed 2 confirmed antithrombin III(ATIII) deficiency tests. Discussion: Spontaneous anterior spinal cord syndrome, is rare, and affects the anterior 2/3 of the spinal cord, causing motor paralysis and loss of pain and temperature below the level of injury. Any process that limits blood flow in the region can be an etiology, spontaneous and thrombophilia causes in young people are rarely reported. ATIII is a blood protein, which blocks the formation of abnormal blood clots, and at low levels, predisposes to thrombus formation, causing ischemia in multiple organs. In this case, the patient had acute lung and spinal cord involvement acutely. There was no family history of hematologic disease. The neurological outcome was positive, the patient presented with independent gait 30 days after discharge. He is on full anticoagulation with Warfarin 5mg (5x/week) and is in motor rehabilitation. Final comments: we reveal a case of acute paraplegia, of spontaneous, sudden and rare occurrence in a young man, affecting the spinal cord and the lung simultaneously, as the first manifestation of thrombophilia.
Keywords: pulmonary thromboembolism, computed tomography angiotomography, cerebrospinal fluid, magnetic resonance imaging
CTA, computed tomography angiotomography; MRI, magnetic resonance imaging; PTE, pulmonary thromboembolism; CSF, cerebrospinal fluid; NR, non-reactive; GLT, general laboratory tests, RF, rheumatoid factor
A healthy 32-year-old male presented with bilateral Dorsal at scapular level upon arising in the morning, sudden, intense, brief onset, evolving to occipital headache, the worst pain of his life. The patient presented paraplegia, involuntary priapism, refractory and persistent. Bladder retention requiring urinary catheterization delay, and fecal retention. There was no report of current illicit substance use; however, he reported previous recreational marijuana and cocaine use. On admission physical examination, there was no change in skin color, arterial pulses, and lower limb trophism; motricity was grade 0 in the left lower limb and grade 1 in the right lower limb. He presented loss of thermal and pain sensitivity at the T2 level, and bilateral Babinski reflex. An indwelling urinary catheter was used due to urinary problems, and he persisted with involuntary priapism for five days on hospitalization. Computerized tomography (CT) of the abdomen and neck were normal. Chest angiotomography showed minimal filling failure in the right lower lateral segmental and sub segmental artery, consistent with acute pulmonary thromboembolism (PTE). General laboratory tests (GLT) and Cerebrospinal fluid (CSF), were normal. Magnetic resonance imaging (MRI) of the spinal cord showed ischemia of the anterior spinal artery beginning at C7 - T8. There were no arteriovenous malformations or aneurysms. Thrombophilia screening showed 2 confirmed antithrombin III (ATIII) deficiency tests. *12/12/2020 (GLT): Non-Reactive (NR)/Reactive (R) : Anti-HIV I/II: NR/Anti-hbs NR/ Hemosedimentation rate :80 / Anti-HCV NR/ VDRL NR/ FtaBs igM/IgG: NR/ FAN: NR/ P-ANCA E C-ANCA NR// B12 Vitamin B12 312/Reticulocyte 2.70 [Reference Value(RV) <2.7)]/C Protein functional: 145% (RV:140%)/ FtAbs IgG: NR/Factor V LEIDEN: Negative/ Factor VIII: 213.6 (RV:70-150) / Aldolase 9.1/D-dimer 0.9 (VR: <0,5)/ Serum iron test: 74 (LR:65-175)/TSH 4,17/Rheumatoid Factor(RF): 3,5(NEGATIVE)/Fibrinogen:313(VR:180-350)/ SCHISTOSOMOSOME IgG: NR
Spontaneous anterior spinal cord syndrome is uncommon and very rare in young adults. It affects the vascularization of the anterior 2/3 of the spinal cord, causing acute motor paralysis and sensory loss (pain and temperature) below the level of injury. Any vascular process that limits and interferes with the blood flow in the spinal cord region may be the etiologic cause. However, spontaneous, thrombophilia causes in young adults have rarely been reported in the world literature. Antithrombin III (ATIII) is a blood protein that blocks the formation of abnormal blood clots and, at low levels predisposes to thrombus formation, favoring the occurrence of thromboembolic events in various organs. ATIII deficiency has remarkably higher risk rates for thromboembolic events, than those reported for other thrombophilia. In addition, thrombosis can occur early and recurrently. Thrombosis is a complex disease, and ATIII deficiency shows remarkably heterogeneous clinical range with vascular events from a young age and recurrently. The onset of the hematologic picture can vary greatly, as environmental as well as genetic factors interfere in the modulation of the biological and clinical phenotypes of thrombosis related to antithrombin deficiency (Figure 1).
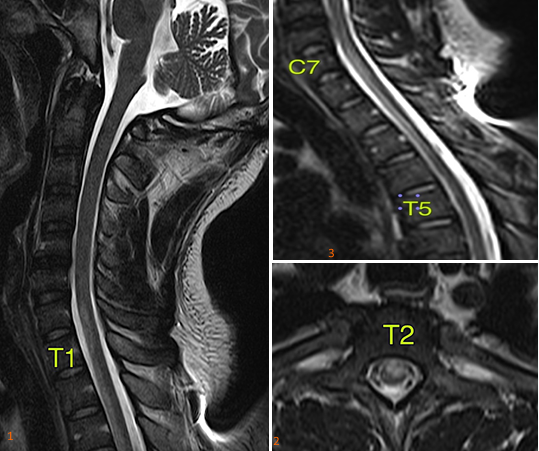
Figure 1 Sagittal T2-weighted sequence of the spine with signal alteration in the anterior third of the spinal cord. 2. axial T2-weighted sequence observes signal alteration in the anterior third of the spinal cord with predominance of grey matter involvement. With predominance of involvement in the gray matter. 3. extension of the alteration in the anterior third of the spinal cord (C7-T5).
In this case, the patient presented with acute pulmonary involvement with acute pulmonary thromboembolism and anterior spinal artery occlusion as the first manifestation of the hematologic disease. Antithrombin III deficiency was detected and confirmed in blood tests, and elucidated as the primary etiologic cause, since there are no other commemoratives. The patient had no family history of hematologic disease and no history of previous thrombosis. The patient showed a good therapeutic response with gradual improvement of the motor part, after 30days of hospital discharge, the patient was able to ambulate on his own. He is on full anticoagulation on sodium warfarin 5mg (5x/week) and physical therapy for motor rehabilitation 3x/week. After 8months of the event, there was a complete motor recovery, being able to perform complex motor activities independently, such as driving and soccer practice; however, there was partial improvement in thermal and pain sensitivity, and a complaint of decreased sensitivity to sexual activities.1–4
This case illustrates a rare cause of acute medullary vascular involvement in a young man with aggressive manifestations of previously undiagnosed hematologic disease. It is important to always remember hypercoagulability etiologies (thrombophilia’s), even if rare, as the cause of severe vascular events in young people without other justifiable risk factors.
None.
None declared by the authors relevant to this article.
No funding sought for the writing or publication of this paper.

©2022 Pinheiro, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.