Journal of
eISSN: 2373-4396


Research Article Volume 6 Issue 3
1Emergency Department, Instituto de Cardiolog
2Echocardiography Department, Instituto de Cardiolog
Correspondence: Rafael Matías Comisario, Cardiologist, Instituto de Cardiología de Corrientes Juana Francisca Cabral, Argentina
Received: June 21, 2016 | Published: July 28, 2016
Citation: Comisario RM, Popilovsky SN, Burgos CG, Fernandez EG, Barrios PA, et al. (2016) Prognostic Factors and 6 Months Survival of Out-Of-Hospital Cardiac Arrests in a Cardiology Institute From Corrientes, Argentina. J Cardiol Curr Res 6(3): 00203. DOI: 10.15406/jccr.2016.06.00203
Introduction: Cardiac arrest is the leading cause of morbidity and one of the main sources of health care costs. Each year more than 166,000 patients experience cardiac arrest in the United States and approximately 60% of them is treated in emergency departments.
Material and Methods: Cardiac arrest patients (88) admitted to the Emergency Room (ER) at the Corrientes Cardiology Institute (ICC) were studied. Demographic information (suspected cardiac arrest etiology, heart rhythm on admission, hospital survival and 6 months survival) was collected.
Results: Cardiovascular causes of cardiac arrest corresponded to 39.8%. In-hospital survival and 6 months survival was 25% and 12,5% respectively. Variables associated to worse prognosis in the univariate analysis were non-cardiovascular cardiac arrest (OR 8.8; CI 1.7-43; p=0.003), unknown cause of cardiac arrest (OR 1.79; CI 1.46-2.18; p=0.003), but no variable was an independent predictor in multivariate analysis. Mean survival was 76 days, and survival in patients discharged alive was 297 days (median 161 days). At follow-up patients had worse prognosis if admitted for non-cardiovascular origin of cardiac arrest (p=0.003), patients without clear origin of cardiac arrest (p=0.0001); and patients with non-shockable rhythms on admission (p=0.009).
Conclusion: Prognosis was worse in patients admitted for cardiac arrest secondary to non-cardiovascular causes, patients without clear origin of cardiac arrest and those with non-shockable rhythms.
Cardiac arrest is the main morbimortality cause and one of the main sources of health costs in the United States.1 In this country, more than 166.000 persons experiment a cardiac arrest annually, and aproximmately 60% of them is treated in emergency departments.2 A cardiac arrest is a particular entity regarding mortality, De Vreede-Swagemakers et al.3 studied 375 cases of sudden death, finding a survival of 13,5% in witnessed events and 6,2% in non-witnessed events. Nichol et al.4 found a survival of 4,6% in a 20520 patients survey.
Etiology is not always found, there is an important number of patients whose first contact with health professionals is at the event of cardiac arrest itself; however some series find that cardiac causes are present in more than 70% of the cases.2. Time and training are important factors, Weaver et al.5 found that early cardiopulmonary assistance is related with a better prognosis and Hallstrom et al.6 conducted a study in which survival was improved when cardiac arrest was assisted by trained volunteers. Admission rythm is also important, suggesting time of event onset. The United States Centers for Disease Control and Prevention published in 2011 a five-year registry, the CARES Registry.7 enrolling 40274 patients with out-of-hospital cardiac arrests, finding that the in-hospital survival in patients with shockable rythms on admission was 27% whereas in non shockable rythms the survival was as poor as 5, 2%. Kern et al.8 explain that survival curve in out-of-hospital cardiac arrest patients is particular: among those admitted to emergency department only 40% will have a successful reanimation and only 10% will be discharged alive.
Secundary objectives
Consecutive patients admitted for out-of-hospital cardiac arrest to the emergency department of the Corrientes Cardiology Institute, from january 9 of 2012 to july 16 of 2014, were included. An observational, unicentric, retrospective study was conducted collecting data about the events such as rythm on admission, probable etiology of cardiac arrest (this was with no specific protocol, only indirect interrogatory and complementary tests like laboratory results, electrocardiogram, chest X-ray and CT scan when possible), in-hospital survival and 6 month survival. Suspected etiologies were grouped in cardiovascular origin and non-cardiovascular origin. Alive discharged patients were followed via phone call survey. When phone comunication was not posible (2 cases), the last hospital alive admission registry through hospital admission software DocSys was considered.
Data was collected using Microsoft Excel 2010 and analyzed with statistics software SPSS 21. Cuantitative variables are expressed by mean and standard deviation and qualitative variables are expressed in percentages. For associations between cualitative variables, Chi2 test was used, and when the value of n was lower tan expected, Fisher exact test was used. Interaction terms with a p value of less than 0,04 were considered to be statistically significant. For identification of independent prognostic variables, binary logistic regression was used. Free event survival analysis was performed with Kaplan-Meier function.
The consecutive patients admitted for cardiac arrest to the emergency department of the Corrientes Cardiology Institute, from january 9 of 2012 to july 16 of 2014 were 88. Mean age was 68, 9 ± 15, 4 years, and 66% males. The main causes of cardiac arrests (distributed by frecuency) were: ST-segment elevation myocardial infarction 17%, non ST-segment elevation myocardial infarction 14, 8%, pneumonia 9, 1%, stroke 4, 5%, pulmonary embolism 3, 4%, sepsis 2, 3%, complete AV block 2, 3%.
The risk factors distribution was: hypertension 52,3%, coronary artery desease 35, 2%, diabetes 23, 9%, dislipidemia 17%, chronic renal impairment 15, 9% (hemodyalisis 2, 3%), tabaquism 13, 6%, atrial fibrillation 10,2%. Antecedents were: chronic heart failure 23,9%, previous percutaneous coronary angioplasty 21%, pacemaker 8%, coronary artery by-pass graft 6, 8%, pulmonary hypertension 4, 5%, chronic obstructive pulmonary disease 3, 4%.
The admission cardiac rythms were: asystole 30, 7%, pulseless electrical activity 28, 4%, ventricular fibrillation 18, 2%, and ventricular tachycardia 9, 1%, (non shockables 59, 1%, shockables 27, 3%). In 13,6% of cases, the admission cardiac rythm data was missing. Suspected etiologies of cardiovascular origin was 39,8% and those of non-cardiovascular origin was 60, 2%. In-hospital survival was 25% and 6 months survival was 12, 5%. Survival according to age was: 20 - 29 years: 0%; 30 - 39 years: 1, 1%; 40 - 49 years 1,1%; 50 - 59 years: 3, 4%, 60 - 69 years: 8%; 70 - 79 years: 5, 7%; 80 - 89 years: 5, 7%, 90 - 99 years 0% and 100 - 110 years: 0% (Figure 1).
Univariate analysis showed worse prognosis in patients with non-cardiac origin of cardiac arrests (OR 8, 8; IC 1,7 - 43; p=0,003), patients whose diagnosis could not be identified (OR 1, 79; IC 1,46 - 2,18; p=0,003), and a trend towards significance in patients with non shockable rythms (OR 2, 8; IC 0, 7 - 10, 7; p=0,09) (Table 1).
|
Factor |
OR |
IC |
p |
|
Diagnosis |
|||
|
STEMI |
0,14 |
0,05 - 0,9 |
0,05 |
|
NSTEMI |
0,4 |
0,07 - 1,1 |
0,08 |
|
Pulmonary embolism |
0,74 |
0,99 - 1,08 |
0,6 |
|
Complete AV block |
0,1 |
0,008 - 2,27 |
0,2 |
|
Isquemic stroke |
0,32 |
0,02 - 3,2 |
0,3 |
|
Hemorragic stroke |
0,65 |
0,98 - 1,03 |
0,87 |
|
Pneumonia |
1,01 |
0,11 - 9,0 |
0,6 |
|
Sepsis |
0,72 |
0,99 - 1,06 |
0,76 |
|
Complicated abdominal aortic aneurysm |
0,9 |
0,99 - 1,06 |
0,76 |
|
Non cardiovascular diagnosis |
9,4 |
1,7 - 43 |
0,003 |
|
Unknown diagnosis |
1,79 |
1,46 - 2,18 |
0,003 |
|
Rythm |
|||
|
Ventricular fibrillation |
0,6 |
0,08 - 1,27 |
0,1 |
|
Ventricular tachycardia |
0,1 |
0,03 - 0,9 |
0,05 |
|
Pulseless electrical activity |
5,3 |
0,38 - 9,5 |
0,3 |
|
Asystole |
0,9 |
0,4 - 10,7 |
0,2 |
|
Non shockable rythms |
2,8 |
0,7 - 10,7 |
0,09 |
Table 1 Univariate analysis of factors for in-hospital mortality
However, none of these variables was independent predictor in multivariate analysis. Mean survival was 76 days, and alive discharged patients mean survival was 297 days (median 161 days). In-hospital survival and 6 months survival according to admission cardiac rythm are summarized in Figure 2.
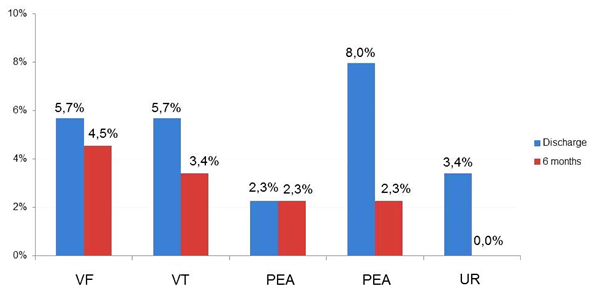
Figure 2 In-hospital and 6 month survival in cardiac arrest patients admitted according to admission rythm. (VF: Ventricular fibrillation. VT: Ventricular tachycardia. PEA: Pulseless electric activity. Asyst: Asystole. UR: Unknown rythm).
Event free survival curve shows that there is worse prognosis in patients without a certain etiology of cardiac arrests (Figure 3) p=0,0001; in patients admitted with a non-cardiovascular origin of cardiac arrest (Figure 4) p=0,003; and in those patients admitted with non-shockable cardiac rythms (Figure 5) p=0,009.
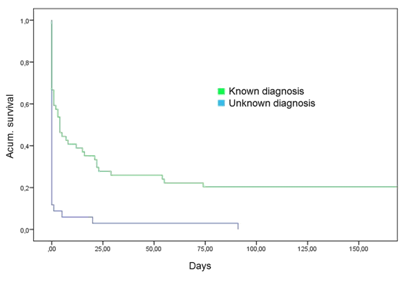
Figure 3 Survival in days for cardiac arrest admitted patients according to certainty of diagnosis (known etiology versus unknown etiology) p=0,003.
The main limitations of the study were:
Cardiac arrests have elevated mortality, and the information gathered is comparable to other publications. Although follow up is a non-gaussian variable, its expression using mean could give a false idea of survival (mean of 76 days), this is a variable that beats even non parametrical measurements of central tendency finding that median of survival is 0 because more than half of the population dies on the same admission day. For this reason alive discharged patients survival is expressed in mean and median (297 y 161 days respectively).
It is no surprising that among worse prognosis factors we found the fact of not knowing the etiology of the cardiac arrest. First treatment measures are common to all cases, but not being able to arrive to a diagnosis could limit specific treatment options. When a diagnosis was achieved, was with aid of complementary tests, and perhaps not arriving to a diagnosis represents not achieving spontaneous circulation and consecuent ICU admission with exhaustive study of the patient. The other factor associated to worse prognosis was admission with non-shockable rythms, probably representing more time from onset to arrival to emergency department, linked to cerebral anoxia. Survival according to cardiac rythm on admission at Corrientes Cardiology Institute differs from the survival reported by the CARES Registry.7, where we found hospital survival of 27% in patients with shockable rythms, but they found 5,7%.
There are also other slight differences, such as hospital survival in patients admitted with pulseless electric activity, they found 7,3% and we found 2,3%, and finally patients admitted with asystole, they registered in-hospital survival of 2,3% and we found 8%. These differences are probably attributable to the number of patients registred (40274). Young population had also low survival, patients under 39 years old were admitted by cardiogenic shock (one), hemorragic stroke (one), pulmonary embolism (one), unknown diagnosis (three) with a in-hospital mortality of 83% and 100% at six months. This differs from the report of van der Werf et al.9 with records of 4286 anatomopatologic reports of people under 40 years old between 1990 and 2009, where they found that even in this age range, the most common etiology is premature coronary artery desease (31%), followed by myocarditis (9, 1%), left ventricular hypertrophy (7, 7%) and hypertrophic cardiomyopathy (7, 5%), reaching 26% of cases with unknown etiology. Again, probably the number of patients can justify this difference.
In this study at the ICC, it was also observed that cardiac arrest patients admitted with a cardiac cause, have a better prognosis. This might be in part explained by the center specialization in this area; although the ICC is not a hospital with all medical areas available, a great proportion (60,2%) of patients with non-cardiac causes is admitted. Significative differences were not found at follow-up with any other variables.
The present study showed the pharmacological potential of the ethanolic extract of Neem bark. Our findings demonstrated that the F-EtOAc, obtained after saponification of EtCNeem, showed to be rich in phenolic and flavonoid compounds with antioxidant potential, as well as a nontoxic.
None.
The authors declare there is no conflict of interests.
None.

©2016 Comisario, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.