Journal of
eISSN: 2373-4396


Case Report Volume 2 Issue 5
Department of Cardiology, Bulgaria
Correspondence: Valentin Hristov, Department of Cardiology, Specialized Cardiology Hospital for Active Treatment -Pleven, Bulgaria
Received: February 19, 2015 | Published: May 6, 2015
Citation: Hristov V, Negrilov S, Marchev S, et al. Percutaneous angioplasty of the right coronary artery originating from the left coronary sinus. J Cardiol Curr Res. 2015;2(5):119-122. DOI: 10.15406/jccr.2015.02.00074
Congenital anomalies of the coronary arteries are relatively rare - they are found in 1.3% of all patients undergoing coronary arteriography. They are a common cause of sudden cardiac death in young athletes and hard labor workers. The atypical origin of the right coronary artery from the left coronary sinus has a clinical significance when the anomalous artery is compressed between the aorta and the pulmonary artery causing intermittent ischemia. Atherosclerosis and rupture of the atherosclerotic plaque could be a common cause for ischemia too. The atypical origin of the coronary artery is a challenge for the interventional cardiologist.
Keywords: Percutaneous angioplasty, Right coronary artery, Atypical origin from the left coronary sinus, Coronary anomaly
Coronary anomalies are a congenital defect of one or more of the coronary arteries. They could consist of anomalous aortic origin and/or altered size of the coronary arteries. They are often diagnosed in patients with other heart abnormalities. Coronary arteries supply highly oxygenated blood to the myocardium, therefore the presence of such an anomaly could limit the supply of oxygen to the myocardium. Coronary anomalies could lead to myocardial ischemia and sudden cardiac death. The people at greater risk of sudden cardiac death caused by coronary anomalies are young athletes and hard labor workers.
Congenital anomalies of the coronary arteries are relatively rare. They are found in 1.3% of all patients undergoing coronary arteriography. Anomalous aortic origin of the right coronary artery (RCA) represents 8% of these congenital malformations and was considered benign for many years.1 In 1982 Roberts suggests, that the anomaly could lead to clinical manifestations similar to the ones instable angina pectoris, myocardial infarction, ventricular tachycardia or sudden cardiac death. This coronary anomaly has a clinical significance when the anomalous artery is compressed between the aorta and the pulmonary artery causing intermittent ischemia.2 A cause for ischemia in this artery could be also a more common one-atherosclerosis and subsequent inflammation and rupture of the atherosclerotic plaque (Figure 1 & 2).3
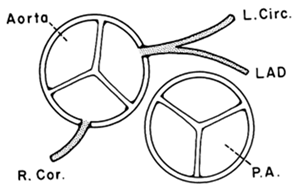
Figure 1 Normal origin of the two coronary arteries: left main coronary artery originating from the left Valsalva sinus. Right coronary artery originating from the anterior (right) Valsalva sinus.
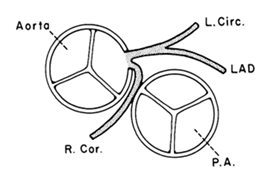
Figure 2 Both coronary arteries originating from the left Valsalva sinus.3
The clinical manifestation of the anomalous aortic origin of the right coronary artery can include angina pectoris, myocardial infarction, ventricular tachycardia and ventricular flutter. Most commonly these are present during or after physical activities. There are two pathophysiological mechanisms, which could be acting at the same time or separately. The anomalous artery could be compressed between the major vessels of the heart during the cardiac cycle. The second mechanism involves compressing of the anomalous artery by a dilated aorta. This diagnosis could be suspected more often in patients without major coronary risk factors, but with symptoms of angina pectoris, myocardial infarction or malignant ventricular arrhythmias. A non-invasive method for diagnosis is also coronary CTA (Figure 3).4 Percutaneous angiography is performed as an invasive method for diagnosis of this condition. Treatment of this anomaly could be CABG, reimplantation of the ostium to its rightful place or implanting a stent in the compressed segment of the RCA. Indication for operation is proved ischemia.5
This clinical case is about a 69 years old woman who admitted for the first time in the hospital with chief complaints of chest pain predominantly on the left, radiating towards the left shoulder, arm and neck. These symptoms were accompanied by shortness of breath, diaphoresis and nausea. The onset of symptoms was around 14:30 in the afternoon, and shortly after that the patient seeked medical help in the ER. After ECG was recorded she was diagnosed with STEMI of the inferior wall of the left ventricle (ST segment elevation myocardial infarction). Patient was transported for interventional treatment. The physical examination revealed normal body temperature, 146 bpm heart rate and 200/120 mmHg arterial pressure. General appearance: alert, conversant, in distress. Eyes: anicteric sclerae, moist conjunctivae; no lid-lag; PERRLA (Pupils equal, round, reactive to light and accommodation). Head Eyes Nose and Throat were atraumatic; the oropharynx was clear with moist mucous membranes and no mucosal ulcerations; normal hard and soft palate. Neck: Supple. No JVD. No rigidity.. Lungs: Coarse vesicular breath sounds, moist rales in more than half of each lung field. CV: Heart sounds were normal but irregular, with no murmurs. Abdomen: Soft, non-tender; no masses or HSM. Extremities: peripheral edema, no extremity lymphadenopathy. Skin: pale, profuse sweating, oral cyanosis, no rash, ulcers or subcutaneous nodules. Psych: Appropriate affect, alert and oriented to person, place and time. The ECG showed atrial fibrillation, heart rate-146 bpm, ST- segment elevation-1 mm in leads II, III, AVF. The echocardiogram revealed hypokinesia in the inferior wall segment of the left ventricle without any significant valvulopathy or pericardial fluid, LV- dyssynchrony with EF (Simpson) - 40 %. The aortic root and ascending aorta were normal. Main laboratory findings revealed CPK-138 IU/L, normal range: 0-240 IU/L; CK-MB-21 IU/L, normal range: 0-24 IU/L; TROPONIN I- 0, 46 ng/ml.
The patient was transferred to the Catheterization Laboratory in order to undergo coronary angiography. The coronary angiography revealed normal anatomy of Left Main Coronary Artery, LAD- 80% mid segment stenosis. LCx - irregularities. RCA - anomalous origin from the left Valsalva sinus. 50% mid segment stenosis, distal occlusion with thrombus. PCI was performed with guiding catheter XB 3.5 6F, coronary guide wire Terumo Runthrough 0.014". Predilation with balloon 2, 75/20 mm and implantation of two drug eluting stents 2, 75/28 mm with overlapping. Post-dilation at the site of overlapping with the balloon of the second stent.
The patient was previously hospitalized for chronic heart failure NYHA class III and ventricular fibrillation, which was treated with a synchronized shock. She also has arterial hypertension present for the past 20 years, permanent atrial fibrillation and type 2 diabetes. For these conditions she was on the following medication therapy: Bisoprolol Fumarate, Telmisartan, Amiodarone, Gliclazide, Metformin, Acenocoumarol, Tavipec and Azithromycin (Figure 4–6). The cause of the present ischemia is not a result of a mechanical compression of the artery, but is a result of atherosclerosis and plaque rupture with subsequent development of myocardial infarction (Figure 7 & 8).
Medication therapy after discharge
Aspirin 100 mg, Clopidogrel 75 mg, acenocoumarol, metoprolol, amiodarone, HMG-CoA reductase inhibitor, furosemide, spironolactone, ACEI, metformin.
Although coronary anomalies are not common in the clinical practice, they should not be underestimated especially in young athletes and physically active people. It is imperative that angina pectoris symptoms in these groups of patients be recognised and diagnosed. Methods used for diagnosis are - history of the present illness, physical examination, ECG, coronary CTA and coronary arteriography. Some coronary anomalies could be asymptomatic during childhood. Their diagnosis in adulthood is due to the clinical manifestation of myocardial ishemia as a result of coronary artery disease and its complications, or by mechanical compression of the anomalous artery. In this case study the patient presents itself with chest pain,acute myocardial infarction and a medical history of ventricular tachycardia. 30 days after the initial hospitalisation, the patient was admited for hospital treatment again,because of the persistent symptomatic significant stenosis of LAD. Coronary angiography revealed optimal result after the PCI of the RCA. There are also no sighs that RCA is situated between the aorta and the pulmonary artery.This proves that the etiology of STEMI in this case was purely due to athrerosclerosis.
None.
The authors state that there is no conflict of interest.
None.

©2015 Hristov, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.