Journal of
eISSN: 2373-4396


Case Report Volume 15 Issue 5
Department of Cardiology, Mittal Hospital & Research Centre, India
Correspondence: Dr Sitaram Mittal, Department of Cardiology Gokhale Institute of Polytical Sciences and Economics, Pune, India
Received: December 22, 2022 | Published: December 30, 2022
Citation: Mittal SR, Govind M. Objective electrocardiographic documentation of ‘walk- through angina’ phenomenon during treadmill stress electrocardiography using Bruce protocol. J Cardiol Curr Res. 2022;15(5):140-144. DOI: 10.15406/jccr.2022.15.00569
The term ‘walk through angina’ is used when angina is relieved inspite of continued exertion. Objective documentation of ‘walk-through angina’ is rare. Two cases of ‘walk - through angina’ phenomenon with objective electrocardiographic documentation during treadmill stress test are reported. In both cases relief in angina was associated with reduction in electrocardiographic signs of ischemia. In one case, relief of angina was associated with reduction in rate - pressure product. In the second case angina reduced even when the rate pressure product was higher than at the onset of angina. Several factors could reduce angina inspite of increase in work load. Relief in anxiety, reduction in stress of exercise testing, coronary vasodilation, increased flow through collaterals or some adaptive process, alone or in combination, could contribute to relief in angina. Treatment is similar to chronic stable angina.
Keywords: angina of effort, coronary artery disease, coronary vasospasm, electrocardiographic exercise testing, read mill test, walk - through phenomenon, warm - up phenomenon
In ‘walk - through angina’ phenomenon, patient develops angina in the initial phase of exertion, However, if the patient continues to walk, angina gradually disappears.1–7 Appreciation of this phenomenon is important because relief in anginal discomfort with continuation of effort may mislead the patient as well as a clinician against the diagnosis of angina on effort. This is important because this phenomenon can occur even in the presence of severe coronary artery disease.3,4 Appreciation in also important because some of these patients may show significant improvement in exercise tolerance with exercise training.4 Documentation of walk-through phenomenon during exercise testing is rare.3 Mac Alpin and Kattus14 studied twelve patients of angina. They used a ramp protocol which allowed continued exercise at the same pace or minor increments in treadmill speed. Only four cases showed true ‘walk - through phenomenon’. In these cases also ischemic ST segment depression persisted even after decrease in severity of angina. Thus, there was no objective evidence of ‘walk- through phenomenon’. Other eight cases walked - through after reducing the speed of the treadmill or after a short rest or after use of nitro-glycerine. Thus, these cases were really examples of “ warm - up phenomenon” and not “walk-through” phenomenon. Rizi et al.5 have reported a patient who demonstrated scintigraphic left ventricular regional wall motion abnormality and decreased LV ejection fraction at the time of exertional angina which became normal at peak exercise with disappearance of ischemic pain despite higher systolic pressure-heart rate product. ECG remained normal throughout exercise. Coronary angiography revealed 80% proximal occlusion of right coronary artery. Gavazzi et al.3 observed “walk - through” phenomenon only in three out of 3900 exercise tests. It is not clear whether these cases had objective electrocardiographic or other evidence of ‘walk - through phenomenon’. Price8 and Leftwich9 have also reported some cases but once again without any objective confirmation. We observed objective electrocardiographic evidence of ‘walk - through phenomenon’ in two cases of angina, during treadmill stress electrocardiography using standard Bruce protocol.10
Case 1
A 67 year-old-female presented with complaint of angina on effort. Family history was not contributory. Fasting lipid profile and glycosylated haemoglobin levels were normal. Resting, supine electrocardiogram was normal (Figure1). Resting, supine heart rate was 54 beats per minute. Resting, supine blood pressure was 130/80 mm Hg. Examination of cardiovascular system and respiratory system was normal. Detailed echocardiographic examination did not reveal any abnormality. During second stage of treadmill stress test, patient complained of chest discomfort. Electrocardiogram showed sinus tachycardia (heart rate-115 beats per minute) and significant ST segment depression in leads I, II, aVF, V4 ,V5, V 6 and ST segment elevation in leads aVR and V1 (Figure 2). However, the patient felt that she could continue exercise. Gradually her discomfort reduced and heart rate started decreasing. By the end of third stage chest pain had disappeared and heart rate dropped to 82 beats per minute. Although the systolic blood pressure increased to 160/80 mm Hg, rate pressure product declined from 16100 at the end of second stage to 13120 at the end of 3rd stage. There was significant normalization of ST segment deviations (Figure 3). Patient could exercise for nine seconds during stage 4 without recurrence of angina or ST segment changes in electrocardiogram. There was no recurrence of angina or any fresh change in electrocardiogram during recovery (Figures 4&5).
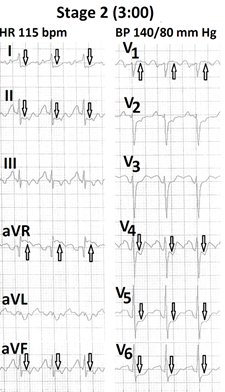
Figure 2 Electrocardiogram recorded at the end of the second stage of Bruce protocol showing sinus tachycardia (115 bpm) with significant ST segment depression in leads I, II, aVF, V4 to V6 and ST segment elevation in leads aVR and V1 .
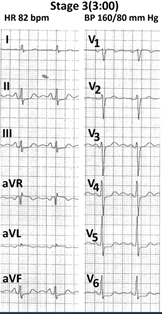
Figure 3 Electrocardiogram recorded at the end of third stage of Bruce protocol showing heart rate of 82 bpm with significant reduction in ST segment depression in leads I, II, aVF and V4.
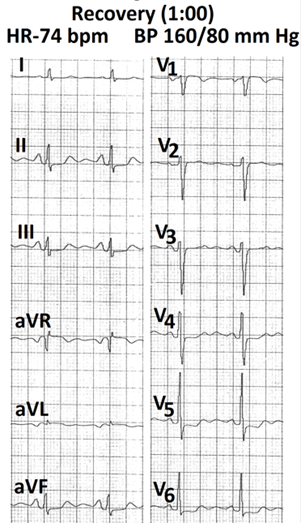
Figure 4 Electrocardiogram recorded at the end of first minute of recovery showing no recurrence of increase in ST segment depression.
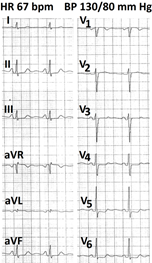
Figure 5 Electrocardiogram recorded at the end of third minute of recovery showing mild decrease in ST segment depressions.
Case 2
A 42 year-old-female presented with history of angina on effort. Family history was not contributory. Fasting lipid profile and glycosylated haemoglobin were normal. Resting supine heart rate was 99 beats per minute. Resting, supine blood pressure was 120/80mm Hg, Resting twelve lead electrocardiogram was normal (Figure 6). Detailed echocardiographic examination did not reveal any abnormality. Towards the end of stage 1 of treadmill test, patient complained of mild chest discomfort. Heart rate was 168 beats per minute and blood pressure was 130/80 mm Hg. Rate pressure product was 21840. ECG showed significant horizontal ST segment depression in leads I, V2 to V6 , slow upsloping ST segment depression in leads II and aVF and ST segment elevation in leads aVR and aVL (Figure 7) Patient continued exercise. By the end of stage 2, chest discomfort disappeared and ST segment depression became rapid upsloping (Figure 8). Heart rate was 187 beats per minute and blood pressure was 140/90 mm Hg. Rate pressure product was 26180.
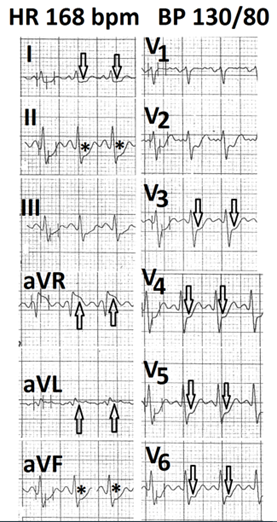
Figure 7 Electrocardiogram recorded at the end of the first stage of Bruce protocol showing sinus tachycardia (168 bpm) with horizontal ST segment depression in leads I, V2 to V6 (marked ), slow upsloping ST segment in leads II, aVF (marked ↓) and ST segment elevation in lead aVR and aVL (marked ↑).
Our cases provide objective electrocardiographic evidence of “walk- through- phenomenon”. Exact mechanism of this phenomenon is not clear. Several mechanisms have been postulated. Firstly, increasing heart rate causes significant dilatation of coronary arteries.11 Continued exercise can, therefore, cause abolition of coronary spasm present at rest and during early phase of exercise. Secondly, anxiety and neurohumoral activation can result in increase in heart rate, coronary tone and blood pressure during the first few minutes of exercise.12 Rate pressure product is an important determinant of myocardial oxygen demand.13 This can result in angina during initial phase of exercise. As exercise proceeds in the first stage, this increase in rate - pressure product usually settles down towards resting level.13 This results in relief of angina. However, if anxiety of stress test continues, angina may persist. Our first case showed significant reduction in heart rate and rate-pressure product when there was relief in angina. However, second case had higher rate- pressure product at the time of relief in angina. Gavazzi et al.3 and Rizi et al.5 have also observed disappearance of chest pain despite a greater rate pressure product. This shows that some different mechanisms are involved in relief of angina in such cases. Thirdly, exercise induced hypoxia can also contribute to dilatation of epicardial coronary arteries14 and collaterals and capillary recruitment.15 This can also contribute to relief in angina at a constant work load. However, increase in collateral circulation may not be adequate if work load is increased in presence of significant coronary stenosis. Fourthly, some authorities feel that relief of angina be due to some adaptation to continued hypoxia. Patterson et al.16 while performing ‘anoxemia test’, in patients with angina pectoris, observed that in an occasional patient ST segment depression may decrease during continued hypoxia. They felt that such adaptation could be related to ‘walk -through angina.’ Such adaptation could occur at cellular level. Drugs like Ranolazine and Trimetazidine reduce angina by acting on cardiac myocytes without modulation of heart rate and blood pressure.17,18 Such a mechanism could also produce relief in angina on continued effort. Some adaptive process is also postulated to be involved in situations where repeated episodes of stress produce angina at higher work load or electrocardiographic evidence of myocardial ischemia diminish at same work load.19,20 Different mechanisms, independently or in combination, could contribute to relief of discomfort in a given patient (Figure 9&10).
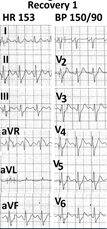
Figure 9 Electrocardiogram recorded at the end of first minute of recovery showing further improvement in ST segment deviations.
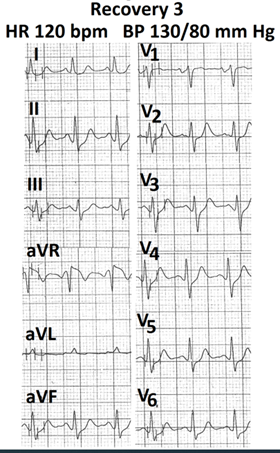
Figure 10 Electrocardiogram recorded at the end of third minute of recovery showing further improvement in ST segment deviations.
‘Walk - through phenomenon’ is not related to severity of lesion seen on coronary angiography.3 Patients with vasospastic angina can have normal coronary angiograms. On the other end patients with stable exertional angina and severe coronary artery disease can also show ‘walk- through phenomenon’.3,4
‘Walk - through phenomenon’ may not be reproduced during a repeat exercise test.3 This is probably related to variations in coronary tone at the time of repeat exercise stress test. Variations in magnitude of anxiety and neurohumoral stimulation could also contribute to such variability. Some ‘adaptive process’ secondary to repeated stress could also play some rate.19,20 Such ‘adaptive process’ plays a role only if the test is repeated after a short period of rest in the same sitting or repeated after a period of exercise training.4 In patients with severe coronary artery disease, delayed appearance of angina or ischemic changes on electrocardiogram could be due to recruitment of more collaterals and capillaries.
In some patients with history suggestive of ‘walk - through angina’, the phenomenon may not be produced during stress testing using any of the conventional protocols. This is difficult to explain. Mac Alpin et al.4 and Rizi et al.5 have observed that ‘walk - through’ phenomenon usually occurred during a steady state of heart rate and blood pressure i.e. at a constant rate-pressure product. During daily walking, work load is relatively constant. During exercise testing, there is progressive increase in work load with each increase in stage of exertion. This progressive increase in work load may not allow relief in angina. Circadian variation in coronary tone could be another factor. Treatment of ‘walk - through angina is similar to that of chronic stable angina.
‘Walk- through’ phenomenon should be differentiated from ‘warm-up phenomenon’. Term ‘warm -up phenomenon’ is considered in following situations. Firstly, when little effort precipitates angina in morning hours whereas even more sternous exertion does not produce angina later in day.1 Circadian variation21 in exercise capacity is due to exercise induced reduction in coronary arterial spasm. Secondly, when first exercise stress test produces angina and ischemic changes in electrocardiogram but second exercise test performed after a rest does not produce angina and ECG changes at the some work load. Thirdly exercise stress test performed after a period of exercise training does not produce angina and ischemic changes at the some work load.4 Some adaption mechanism could be responsible in other cases.22
Walk - through angina’ can occur in patients with vasospastic angina as well as in those with obstructive coronary artery disease. Objective evidence during conventional treadmill testing is rarely found even in persons who give history suggestive of ‘walk - through phenomenon.’ Relief in anxiety with resultant drop in rate pressure product, relief of coronary spasm, exercise induced vasodilation, increased flow through collaterals or ‘adaptation’ , alone or in combination can contribute to this phenomenon.
B Search and review of literature, analysis of findings, compilation of results.
None.
No conflicts of interest.
None.

©2022 Mittal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.