Journal of
eISSN: 2373-4396


Case Report Volume 1 Issue 4
1Department of Cardiovascular and Thoracic Surgery, Cliniques Universitaires Mont-Godinne, Universite Catholique de Louvain, Belgium
2Department of Radiology of Cliniques Universitaires Mont-Godinne, Universite Catholique de Louvain, Belgium
3Department of Cardiology of Cliniques Universitaires Mont-Godinne, Universite Catholique de Louvain, Belgium
Correspondence: Emiliano Navarra, Department of Cardiovascular and Thoracic Surgery, Cliniques Universitaires Mont-Godinne, Universite Catholique de Louvain, CHU UcL Mont-Godinne, Avenue Docteur G. Thérasse, 1, 5530, Yvoir, Belgium, Tel 32-81-42-31-72, Fax 32-42-31-57
Received: July 23, 2014 | Published: September 13, 2014
Citation: Navarra E, Dupont M, Colles P, et al. Giant circumflex coronary artery fistula draining into the coronary sinus. J Cardiol Curr Res. 2014;1(4):109-110. DOI: 10.15406/jccr.2014.01.00021
Coronary artery fistulas are rare congenital anomalies arising from an abnormal direct connection between any coronary arteries and a cardiac chamber, a great vessel or the coronary sinus. In this case report we present a rare case of a giant fistula between the first marginal branch of the circumflex coronary artery and the coronary sinus in a patient symptomatic for dyspnea and palpitation. A selective coronary angiography revealed the presence of a fistula between a coronary artery and the coronary sinus. A contrast-enhanced ECG-gated multi-doctor computed tomography confirmed the presence of a giant coronary artery fistula between the first obtuse marginal branch of the circumflex coronary artery and coronary sinus. Due to the rapid progression of the fistula diameter and symptoms, the patient underwent to a surgical closure of the fistula. At six months follow up, the patient was in excellent condition and asymptomatic for dyspnea, palpitation or chest pain. A control contrast-enhanced ECG-gated multi-dector computed tomography showed a complete closure of the fistula without residual shunt.
Keywords: coronary, malformations, coronary fistula, congenital coronary fistula, coronary sinus fistula
CAF, coronary artery fistula; Cx, circumflex; MDCT, multi-doctor computed tomography
Coronary artery fistula (CAF) is a rare congenital anomaly with a reported incidence of 0.1–0.2% in the adult population referred for cardiac catheterization.1 It is defined as a direct connection between a coronary branch and a cardiac chamber, the coronary sinus, the inferior vena cava, or a pulmonary artery or vein. Only few cases of circumflex (Cx) coronary artery fistula, draining into the coronary sinus have been reported in the literature,2,3 representing only the 7% of all CAF.4 The position and the dimension of the fistula are the most important factor influencing the hemodynamic significance and symptoms. In this paper we describe a rare case of a giant aneurismal connection between the first marginal branch of the circumflex artery and the coronary sinus in an adult woman.
The patient, a 57-years-old woman, had a history of hypertension, hyperlipidemia and familiar history of cardiovascular diseases. She was addressed at our institution for a worsening dyspnea on exercise, associated to sporadic episodes of palpitation. Cardiac auscultation demonstrated the presence of a gross cardiac murmur without clear irradiation. Electrocardiogram showed normal sinus rhythm and no other specific changes. Trans-thoracic echocardiography evidenced the presence of a large and tortuous structure on the lateral and basal wall of the heart, showing systolic and diastolic turbulence on colour flow Doppler imaging (Figure 1). At the cardiac catheterization, pulmonary artery pressure was 34/14mmhg. Magnitude of left to right intracardiac shunting was quantified by an oximetry run giving a flow ratio (Qp/Qs) of 1.7with a significant right atrial step-up in blood oxygen saturation. Selective coronary angiography revealed the presence of a gross connection between the first marginal branch of circumflex coronary artery (CX) and the coronary sinus. The proximal segment of the Cx was severely dilated before the origin of the fistula (10.5 mm), while the rest of the coronary anatomy was normal. Fractional flow reserve assessment of the distal part of the Cx, just after the origin of the fistula, was performed and was 0.94. A contrast-enhanced ECG-gated multi-doctor computed tomography (MDCT) confirmed the presence of a giant CAF (max diameter 3cm) (Figures 2a&2b). Phase-contrast MRI measured an average flow per minute of 1.6 l/min in the CAF. Due to the rapid progression of the fistula diameter over the two years of follow up and considering the shunt, the patient underwent a surgical closure of the CAF through a median sternotomy. Digital compression of the distal part of the fistula allowed the antegrade cardioplegia administration. Inspection of the left side of the heart showed the presence of the giant CAF in the atrio-ventricular groove (Figure 3). In his proximal part, the CAF arose with a well delimited neck, and merged in the middle part of the coronary sinus. After the dissection of the CAF from the cardiac surface, the proximal connection of the CAF was closed using a Polipropilene 6-0 U stich on the neck, near the marginal branch the Cx and reinforced by a 3-0 silk ligature. The distal segment was closed by placing two 3-0 silk ligature. Weaning from cardiopulmonary bypass was uneventful and intraoperative trans-esophageal echocardiogram demonstrated good contractility of all myocardial segments and no turbulence or residual flow inside the excluded CAF on the Color-Doppler analysis. At six months follow up, patient was in excellent condition and asymptomatic for dyspnea or chest pain. A control ECG-gated MDCT scan showed a complete closure of the CAF without residual shunt (Figures 2c&2d). At level of the coronary arteries we observed a reduction of the internal diameter of the proximal CX (from 10.5mm to 7.5mm), while at level of the distal Cx, we observed an augmentation of the internal diameter (from 3.7mm to 5mm).
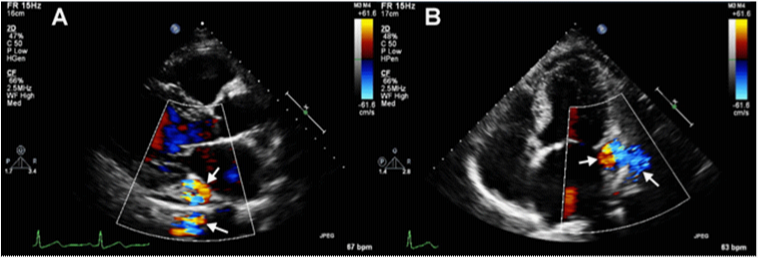
Figure 1 Trans-thoracic echocardiography showing the fistula at level of the atrio-ventricular groove (white arrows) in long axis (A) and four chambers (B) view.

Figure 2 (A) Volume rendering reconstruction (lateral view) of the AV fistula (white arrows) (B) Curved multiplanar reconstruction of the AV fistula (white arrows) (C) Volume rendering reconstruction (lateral view) of the left atrio-ventricular groove after surgical closure of the AV fistula (white star) (D) Curved multiplanar reconstruction of the left circonflex artery and its first marginal branch after closure of the AV fistula (white arrow).
CAF is a rare congenital anomaly and the presentation can widely vary between patients. Young patients are usually asymptomatic. Older patients can present with chest pain, if the CAF produce a myocardial ischemia, or dyspnea, if the symptom are connected with the degree of the shunt. Still debated is the appropriate approach for asymptomatic patients with CAF. The transcatheter closure of the CAF is an attractive alternative to the surgery in case of small CAF,5,6 without aneurysm of the coronary arteries. In case of large CAF, and in presence of aneurysm of coronary arteries, the surgical approach represents the treatment of choice.7
None.
Authors declare that there is no conflict of interest.
None.

©2014 Navarra, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.