Journal of
eISSN: 2373-4396


Research Article Volume 4 Issue 2
1Fellow of the American Society of Hypertension, USA
2Fellow of the Royal Society for Promotion of Health, UK
3Editor-in-Chief of the Journal of Cardiology & Current Research, USA
Correspondence: Aurelio Leone, Fellow of the American Society of Hypertension (USA), Fellow of the Royal Society for Promotion of Health (UK), Editor-in-Chief of the Journal of Cardiology & Current Research (USA), Via Provinciale 27, 19030 Castelnuovo Magra, Italy
Received: November 06, 2015 | Published: December 4, 2015
Citation: Leone A (2015) Evidence of Impaired Night-Response of Blood Pressure in Hypertensive Smokers. An Update*. J Cardiol Curr Res 4(2): 00138. DOI: 10.15406/jccr.2015.04.00138
Epidemiological survey has demonstrated an impaired night response of BP in hypertensive smokers.
This Ambulatory Blood Pressure Monitoring Study (ABPM) conducted in hypertensive chronic smokers and updated by the analysis of more recent findings undoubtedly shows that a large majority of these individuals belongs to the group of non-dipper with a nocturnal fall in BP more than 10%.
Keywords: smoking, hypertension, non-dippers, dippers
S, smoking; H, hypertension; BP, blood pressure; ABPM, ambulatory blood pressure monitoring
Smoking (S) and hypertension (H) are major risk factors for cardiovascular disease.1-3 A crucial question is to assess whether S favors the appearance of H and potentiates the complications associated with hypertensive disease. There is evidence that blood pressure (BP) follows a circadian rhythm4 with morning increase and nocturnal fall in its values. Two groups of hypertensive patients have been described: dipper subjects, who have nocturnal blood pressure lowering more than 10%, and non-dipper individuals with a nocturnal fall in blood pressure less than 10%. The non-dipper hypertensive patients are believed to be at an increased risk of cardiovascular events.5 The purpose of this study was to update our previous data on the response to 24-hour Ambulatory Blood Pressure Monitoring (ABPM) of hypertensive out-patient smokers, enrolled from the Department of Internal Medicine, University of Pisa (year 2010), and Department of Internal Medicine, City Hospital Massa, Italy (data from the year 1999 to 2002) investigated in a previous report partly presented at the 2011 Meeting of the American Society of Hypertension in New York City.6
Study material (Table 1) consisted of 104 hypertensive men, aged from 55 to 72 years (mean: 63+/-8 years), 72 smokers (69%) and 32 non-smokers (31%), used as a control group, undergone 24-hour ABPM. Mean day systolic BP was 162 (+/- 18) mmHg and diastolic BP 92+/-7 mmHg for smokers group and 159+/-17 mmHg for systolic BP and 94+/-6 mmHg for diastolic BP in non-smoker control group. Statistical analysis was conducted by using paired T-test, with a P< 0.05 significant.
|
Patients (number) 104 (100%) |
|
Sex (male) 104 (100%) |
|
Age (mean year+/- SD) 63+/-8 |
|
Smokers 72 (69%) |
|
Non-smokers (control group) 32 (31%) |
|
ABPM 104 (100%) |
|
Mean systolic BP (mmHg, smokers) 162+/-18 |
|
Mean diastolic BP (mmHg, smokers) 92 +/-7 |
|
Mean systolic BP (mmHg, non-smokers) 159+/-17 |
|
Mean diastolic BP (mmHg, non-smokers) 94 +/-6 |
Table 1 Characteristics of Study Population
48 hypertensive smokers (67%) were non-dippers for systolic BP (night BP falls from 0 to 7%) while the other 33% (24 patients) were dippers with a BP fall from 10 to 13% (Table 2). Diastolic reduction was from 3 to 8% in 39 smoker patients (54%) and from 12 to 14% in others. On the contrary, among hypertensive non-smokers (Table 3), there were 26 dippers (81%) for systolic BP with a nightfall from 12 to 15% and 24 (75%) for diastolic BP (reduction from 10 to 14%), and 6 (19%) non-dippers with a systolic and diastolic night-BP fall from 4 to 9%. Statistical difference (P less than 0.05) existed between non-dipper smokers and dipper non-smokers as well as between non-dipper and dipper smokers particularly for systolic BP values.
|
BP Night fall(dippers) Night fall(non-dippers) |
|
N° N° |
|
Systolic BP 24 (33%) < 0-7% 48 (67%) >10% |
|
Diastolic BP 33 (46%) 3-8% 39 (54%) >10% |
|
Total 57 87 |
Table 2 Night-response in smokers for systolic and diastolic BP
|
BP Night-fall (dippers) Night fall (non-dippers) |
|
%fall BP N° %fall BP N° |
|
Systolic BP 12-15% 26 (81%) 4-9% 6 (19%) |
|
Diastolic BP 10-14% 24 (75%) 4-9% 6 (25%) |
|
Total 50 12 |
Table 3 Non-smoker dippers and non-dippers
In this study, hypertensive smokers were more frequently non-dippers particularly for systolic values of BP. It is worth noting that this pattern usually identifies a major extent of cardiovascular damage caused by the association of S with H. Moreover, non-dipper smokers usually have a night reduced fall in BP than that seen in non-dipper non-smokers (Figure 1). Previous and following papers7,8 to the observations here described achieved similar results, although with little differences in the methods of study and parameters assessed. The primary pathological mechanism to explain these responses is related to the role of adrenergic and sympathetic system, which play a different activity on BP in the morning and night. Thus, it is worth noting that S strongly feels the effects of the last two parameters, which are influenced by nicotine and carbon monoxide.9 Therefore, the adverse relationship between S and BP cannot be absolutely denied as this finding undoubtedly shows.
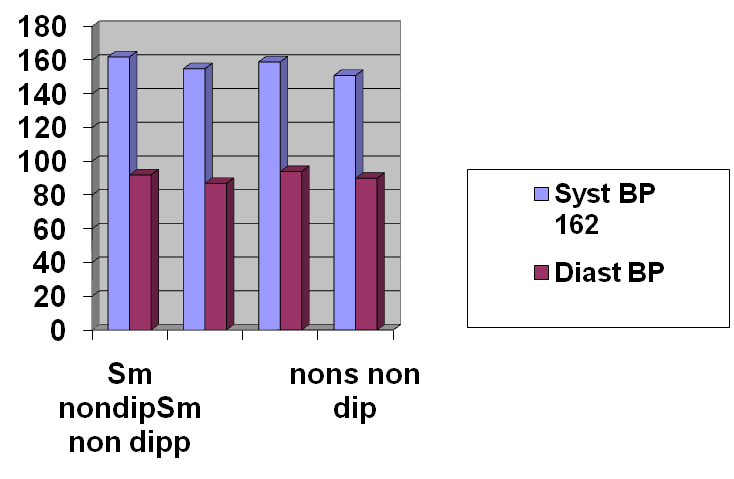
A: Non-dipper smokers day BP; B: Non-dipper smokers night BP; C: Non dipper non-smokers day BP; D: Non-dipper non-smokers night BP.
Figure 1 Day-night BP in non-dipper smokers and non-dipper non-smokers. Although all hypertensive subjects were non-dippers, there is evidence that smokers have a reduced fall in night BP compared to non-smokers.
None.

©2015 Leone. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.