Journal of
eISSN: 2373-4396


Research Article Volume 14 Issue 6
1Department of Cardiology, Henry Ford Hospital, USA
2Department of Emergency Medicine, Henry Ford Health System, USA
3Department of Public Health Sciences, Henry Ford Health System, USA
4Diagnostics Division, Abbott Laboratories, USA
Correspondence: Krishna Modi, Department of Cardiology, Henry Ford Hospital, Detroit, MI, USA, Tel 313-932-5310
Received: October 31, 2021 | Published: December 27, 2021
Citation: Modi K, McCord J, Russell C, et al. Elements of the fourth universal definition used in the diagnosis of acute myocardial infarction. J Cardiol Curr Res. 2021;14(6):175-179. DOI: 10.15406/jccr.2021.14.00538
In the era of high-sensitivity cardiac troponin (hs-cTn) assays, a high proportion of individuals coming to the emergency department (ED) suspected of having an acute myocardial infarction (AMI) will generate a reportable troponin concentration. This results in greater scrutiny in clinical context to differentiate from myocardial injury to prevent inappropriate treatment plans, hospitalizations, and cost to the healthcare system compared to contemporary troponin assays. This study evaluates the use of ischemic symptoms, ECG changes, abnormal angiography/imaging results, which adjudicating physicians use in determining the diagnosis of AMI, as per the 4th universal definition of MI. Patients who presented to the ED and were evaluated for possible AMI were included in this study. After completion of patient care, a diagnosis of AMI was independently adjudicated by 2 cardiologists and 1 emergency medicine physician. This adjudication process determined that patient symptomatology was the most prevalent factor, influencing the adjudication process in 95.2% of AMI diagnoses. Electrocardiography supported AMI diagnosis in 35.7% of patients, with significantly more utility in diagnosing Type 2 AMI. Of the 4 factors, coronary angiography was less performed (10.5%) yet had a high positive rate, being used as one of the confirming factors in 59.5% of all AMI patients. Coronary angiography had greater utility in diagnosing Type 1 AMI. Imaging including echocardiography and nuclear imaging was performed in 30.1% of all patients but was a factor in diagnosing AMI in 26.2% AMI patients. This study emphasizes that symptomology remains critical in diagnosing AMI.
Keywords: high sensitivity cardiac troponin, acute myocardial infarction, fourth universal definition of myocardial infarction
ED, emergency department; AMI, acute myocardial infarction; FUDMI, fourth universal definition of MI; ECG, electrocardiogram; cT, cardiac troponin
Each year 8 to 10million individuals present to emergency departments in the United States and are evaluated for possible acute myocardial infarction (AMI).1 Of these, approximately 1million are diagnosed with an AMI.2 The fourth universal definition of MI (FUDMI) requires an elevation in cardiac troponin (cTn) above the 99th percentile upper reference limit, additional evidence of a rise and/or fall in cTn for the injury to qualify as “acute” as well as at least 1 of the following 4 factors: symptoms of myocardial ischemia, ischemic electrocardiogram (ECG) changes, findings on coronary angiography, or new wall motion abnormalities noted on cardiac imaging.3 However, elevations in cTn levels may be difficult to interpret as they are observed commonly in non-AMI conditions: hemodynamic stress, arrhythmias, sepsis, and chronic kidney disease.4
High-sensitivity cTn (hs-cTn) assays are now replacing conventional cTn assays in the United States. They are defined by having a coefficient of variation at the 99th percentile of less than 10% and levels measurable in at least 50% of a healthy population.5,6 Hs-cTnI assays are much more sensitive and precise when compared to older cTn assays.7 Higher sensitivity and precision at low levels allows AMI to be identified and excluded more rapidly when compared to older cTn assays.7,8 Use of hs-cTnI results in fewer missed diagnoses of AMI, particularly in women, who typically have lower cTn levels.9,10 While there are many benefits of increased sensitivity, reduced specificity raises concern for increases in hospitalizations and cost to the healthcare system, especially if serial testing strategies are not employed.2,11
In the era of hs-cTn assays, the frequency of the factors determining the presence of AMI has not been well-studied. The purpose of this study is to evaluate the relative contribution of ischemic symptoms, ECG changes, cardiac imaging abnormalities, and coronary angiography in the diagnosis of AMI.
Study population
The Rapid Evaluation of Acute Myocardial Infarction in the United States (REACTION-US) study was a prospective diagnostic study that enrolled patients that presented to the emergency department and were evaluated for possible AMI. Details of the study have been previously published.9 The study period was from May 2013 to April 2015 at a single tertiary United States hospital. Inclusion criteria were patients older than 21years of age, symptoms suspicious for possible AMI as evidenced by the clinician ordering an ECG and cTn, and the ability to comply with all aspects of the protocol. Patients were excluded if they were pregnant or breast-feeding, in acute distress requiring immediate life-saving intervention including cardiopulmonary resuscitation or external defibrillation/cardioversion, or if they had a ST-elevation myocardial infarction requiring immediate reperfusion therapy. Patients were also excluded if they did not have baseline bloodwork performed within 1hour of triage ECG or if they were incapacitated. This study was approved by the institutional review board at Henry Ford Hospital. Patients were screened and enrolled by research coordinators after providing written consent.
The subjects underwent clinical assessment by an emergency physician, including history, physical examination, review of ECGs, standard blood testing including contemporary cTn (Siemens Centaur system TnI Ultra assay on a Centaur XP analyzer, Siemens Medical Solutions USA, Inc. Malvern PA; 99th percentile 40ng/L) measurements, and other testing per the emergency physicians’ discretion.
After written informed consent was obtained, research coordinators obtained a detailed history of the patients’ symptoms verified by the medical record and recorded them on a case report form. Blood samples consisting of 6 to 8.5mL of blood were collected in a serum separator tube and an ethylenediaminetetraacetic acid tube. Baseline samples were collected within 60 minutes of completing the triage ECG. Additional blood samples were obtained at 30±10minutes, 1hour ±15minutes and 3 hours ±15minutes.
The ARCHITECT STAT High Sensitivity Troponin-I assay (Abbott, Abbott Park, IL) was used to determine the hs-cTnI levels. The limit of detection has been measured at 1.2ng/L, the 10% coefficient of variation concentration at 4.7ng/L, and the overall 99th percentile of upper reference limit at 26ng/L (90% CI 23-29ng/L).6,11,12
Acute myocardial infarction diagnosis/adjudication
To adjudicate the final diagnosis, 2 board-certified cardiologists independently reviewed the patients’ data from the case report forms. The diagnosis of AMI required at least 1 hs-cTnI above the 99th percentile, evidence of a rise and/or fall in cTn, as well as evidence from 1 of 4 factors to demonstrate clinical evidence of ischemia as per FUDMI.3 The adjudicators reviewed the laboratory findings, ECGs and other available studies including echocardiogram, stress test testing, and coronary angiography reports. They individually classified each case as a Type 1 AMI, Type 2 AMI, or no AMI. If the 2 cardiologists disagreed regarding AMI diagnosis, a board-certified emergency medicine physician reviewed the case and classified it accordingly. If a factor had utility in determining the diagnosis of AMI, it was recorded.
Primary data analysis
Patient demographic, medical history, and presenting vital signs were compared between the AMI and non-AMI patients using the two-sample t-test for numerical data, Fisher exact test for sparse categorical data, and chi-square test for non-sparse categorical data. Serial troponin differences among the 3 study groups; no AMI, type 1 AMI, type 2 AMI, were evaluated with the Kruskal-Wallis Test. The chi-square test was used to assess differences between the type 1 and 2 AMI patients regarding the factors used in diagnosing AMI. Resulting p-values less than 0.05 were considered statistically significant. The analysis was performed using SAS version 9.4 (SAS Institute, Cary, NC).
Characteristics of study subjects, and adjudicated diagnosis
Research coordinators screened 1,699 patients from May 2013 to April 2015. Ultimately 575 subjects were eligible for the study and 569 qualified for analysis. Reasons for exclusion are listed in Figure 1. These include lack of baseline blood sample drawn within one hour of the triage ECG, refusal to participate, impairment (cognitive or substance-induced) and previous enrollment.
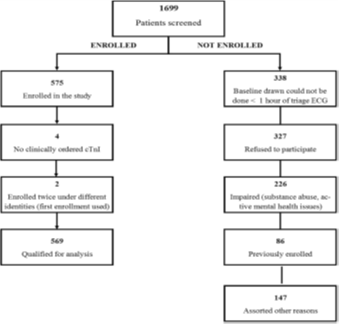
Figure 1 Rapid Evaluation of Acute Myocardial Infarction in the United States (REACTION-US) study patients screened, enrolled, and not enrolled.9
AMI was the adjudicated diagnosis in 7.4% (42/569) patients, with 64.3% having Type 1 AMI (27/42) and 35.7% Type 2 AMI (15/42). There was 1 patient whose diagnosis was ultimately determined to be ST-elevation myocardial infarction. Due to not receiving immediate reperfusion therapy, they were included in this study and are listed as a Type 1 AMI. Patient demographics and past medical history are listed in Table 1. Compared to non-AMI patients, AMI patients were significantly older and were significantly more likely to have prior MI, coronary revascularization, coronary artery disease, hypercholesterolemia, and hypertension, but significantly less likely to have chronic obstructive pulmonary disease.
|
No AMI (N=527) |
AMI (N=42) |
P-value |
|
Age, mean±SD(median) |
55.5±11.2(55.0) |
60.0±9.4(60.0) |
0.013(T)* |
|
Gender, N(%) Female Male |
256(48.6) 271(51.4) |
17(40.5) 25(59.5) |
0.312(C) |
|
Race, N(%) White Black Other |
439(83.3) 85(16.1) 3(0.6) |
34(81.0) 8(19.0) 0(0.0) |
0.734(F) |
|
Comorbidities, N(%) |
|
|
|
|
Hypertension |
424(80.5) |
40(95.2) |
0.018(C)* |
|
Diabetes |
151(28.7) |
13(31.0) |
0.752(C) |
|
Chronic obstructive pulmonary disease |
96(18.2) |
2(4.8) |
0.026(C)* |
|
Congestive heart failure |
124(23.5) |
13(31.0) |
0.279(C) |
|
ESRD on dialysis |
26(4.9) |
4(9.5) |
0.267(F) |
|
Hypercholesterolemia |
256(48.6) |
30(71.4) |
0.004(C)* |
|
Coronary artery disease* |
176(33.4) |
28(66.7) |
<0.001(C)* |
|
History of revascularization |
115(21.8) |
25(59.5) |
<0.001(C)* |
|
History of AMI* |
144(27.3) |
24(57.1) |
<0.001(C)* |
Table 1 Demographics and medical history, with further division based on final diagnosis based on adjudication by board-certified cardiologists and emergency medicine physicians
AMI, acute myocardial infarction; C, chi-square test; ESRD, end-stage renal disease; F, Fisher exact test; SD, standard deviation; T, two-sample t-test
*Statistically significant, P<0.05
The median hs-cTnI levels at baseline, 30minutes, 60minutes and 3hours of the triage ECG are shown in Table 2. There was a statistically significant overall difference in hs-cTnI among the Type 1 AMI, Type 2 AMI and non-AMI patients at all time points.
|
|
Baseline hs-cTnI(ng/L) |
30-minute hs-cTnI(ng/L) |
1-hour hs-cTnI(ng/L) |
3-hour hs-cTnI(ng/L) |
|
No AMI |
5.2(3.0-13.3) |
5.4(2.9-12.6) |
5.4(2.9-12.8) |
5.5(2.9-14.1) |
|
Type 1 AMI |
77.8(28.9-644.0) |
92.4(29.-9-694.2) |
81.7(33.0-659.8) |
199.7(60.6-1523.7) |
|
Type 2 AMI |
146.5(52.8-287.1) |
149.2(56.8-392.6) |
158.5(59.2-307.7) |
132.0(59.6-240.5) |
Table 2 Median (interquartile range) hs-cTnI levels measured by the Abbott Architect assay (Abbott Park, IL) at baseline, 30-minutes, 60-minutes, and 3-hours from triage electrocardiogram
AMI, acute myocardial infarction; hs-cTnI, high sensitivity cardiac troponin
Clinical factors used for diagnostic adjudication
The cardiologists agreed in diagnosing AMI in 73.8% of AMI cases (31/42). Cohen’s kappa for the 3 diagnostic categories (no AMI, type 1 and type 2 AMI) was 0.55 (95% CI 0.37-0.73). A third physician adjudicated the diagnosis in 11 patients. Figure 2 demonstrates the frequency of each clinical factor used to confirm the diagnosis of AMI. Clinical symptoms of myocardial ischemia were present in 95.2% of AMIs (40/42). One Type 1 AMI and one Type 2 AMI patient did not have ischemic symptoms. The patient with Type 1 AMI was diagnosed based on coronary angiography results, and the patient with Type 2 AMI based on ECG and imaging findings.

Figure 2 (A) Frequency of coronary angiography and cardiac imaging performed and (B) frequency of associated acute myocardial infarction diagnosis.
ECG findings of acute ischemia was present in 35.7% (15/42) AMI patients and was significantly less frequent in Type 1 AMI patients (22.2%, 6/27), versus type 2 AMI (60%, 9/15) (P=0.0014) patients. The frequency of coronary angiography and cardiac imaging performed in patients ultimately diagnosed without AMI and with Type 1 or 2 AMI are shown in Figure 2. Coronary angiography was performed in 60 patients (10.5%), with angiographic confirmation of coronary stenosis/occlusion in 25 (41.7%) patients. Coronary angiography findings confirmed AMI diagnosis more often in Type 1 AMI (63.0%, 17/27) versus Type 2 AMI (20.0%, 3/15) patients (P=0.008). Cardiac imaging, echocardiography, or single photon emission computed tomography (SPECT) was performed in 30.1% (171/569) of all patients including 45.2% (19/42) of AMI patients. Abnormal imaging results (wall motion abnormalities and perfusion defects) confirmed myocardial ischemia/infarct in 16.7% (7/42) of Type 1 AMI patients and 27% (4/15) of Type 2 AMI patients.
Figure 3 shows the clinical and diagnostic factors utilized to confirm AMI diagnosis. Clinical symptoms of coronary ischemia were used in >90% of confirmed AMI patients while ECG, echocardiogram, SPECT, and angiographic abnormalities were present in a minority of AMI cases. Coronary angiography is used significantly more often in diagnosing Type 1 AMI (63.0%) compared to Type 2 AMI (20.0%) (p = 0.008). ECG was used significantly more often in diagnosing Type 2 AMI (60.0%) rather than Type 1 AMI (22.2%) (p = 0.014). There were 10 AMI patients that had the diagnosis based on the history alone, and 10 patients that had a suggestive history along with coronary angiography findings.
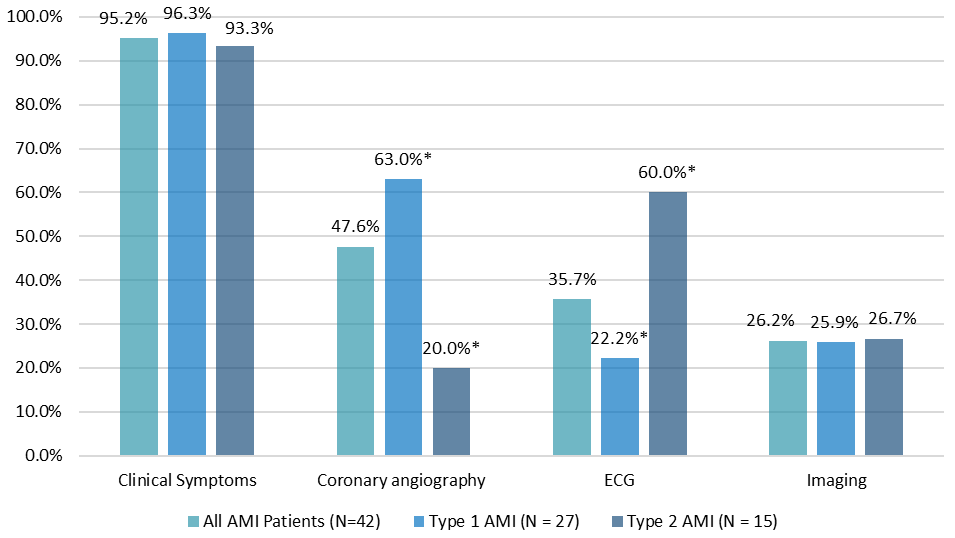
Figure 3 Comparison of the utility of the factors: clinical symptoms, ECG changes, wall motion abnormalities on cardiac imaging, and coronary angiography; used for diagnosis of type 1 and type 2 AMI. Statistically significant difference noted between Type 1 and 2 AMI diagnosis with coronary angiography and ECG (p<0.05). Abbreviations: AMI, acute myocardial infarction; ECG, electrocardiogram.
This study demonstrates that symptoms of cardiac ischemia were the most prevalent factor used in diagnosing AMI, followed by coronary angiography, ECG changes, cardiac imaging. Current literature documents presence of ischemic symptoms in 97% of AMIs.13 We noted equal representation of clinical symptoms being used for diagnosis for Types 1 and 2 AMI. One study suggests it to be the sole factor for diagnosis in 42% of Type 2 AMI patients.13 The significance of clinical symptoms creates a further challenge when the frequency of presentations involving atypical symptoms (especially in Type 2 AMI, women, and the elderly) is taken into account; one study notes dyspnea be the presenting complaint in 58% of Type 2 AMI. Lack of scrutiny in such cases may lead to misdiagnosis and higher mortality.13-15
After clinical symptoms, the most used factors for diagnosing AMI are coronary angiography, followed by ECG and imaging. Coronary angiography more commonly supported the diagnosis of Type 1 AMI as compared to Type 2 AMI (63.0% versus 20.0%, P<0.05). Studies have shown that coronary angiography confirms the diagnosis of AMI in a range of 70.8%-88.7% in Type 1 AMI and 21.5%-50.0% in Type 2 AMI.16-18
Ischemic ECG changes was noted in 35.7% of AMI patients. Compared to angiography, ECG changes was more common in Type 2 AMI (60%). The Thrombolysis in Myocardial Ischemia IIIb trial noted ECG changes in 74% of all AMI cases.19 This study did not document type of ECG changes, but other studies do note different types of ECG changes between Types 1 and 2 AMI. This includes transient ST elevation seen more in Type 2 AMI (8% vs. 3%), and the same with ST depression (30% vs. 22%). Persistent ST elevation and Q waves were significantly more seen in Type 1 AMI (32% vs. 0.9%; 22% vs. 10%).20
This study suggests that despite advances in imaging modalities, they have not yet translated to a high utility for diagnosing AMI. Such modalities were used in 30.1% of the total studied population, but 88.9% of these patients were adjudicated as to not having AMI. This may represent the high negative predictive value of imaging, particularly echocardiography. Unfortunately, echocardiographic abnormalities such as reduced systolic function and wall motion abnormalities can be due to pre-existing conditions and non-ischemic etiology such as infiltrative diseases.21,22 Our AMI patients diagnosed using imaging had equal proportions of echocardiography to nuclear imaging.
Primary limitations of this study include level of discrepancy in diagnosis between the two primary adjudicators, and limited patient population. The two primary adjudicators agreed in less than 75% of cases regarding the three diagnostic categories of no AMI, type 1 and type 2 AMI. Other studies have shown that there is greater agreement between physicians in terms of Type 1 AMI diagnosis, but that Type 2 AMI is more challenging.23,24 Our adjudication process did not include diagnosis of non-thrombotic or non-ischemic myocardial injury that was likely a more accurate diagnosis in a considerable proportion of our reported Type 2 AMIs. The diagnostic decision-making of the 3 adjudicators in our study does not necessarily reflect the clinical thinking of other physicians, and further studies will need to be performed to further validate our work.
This study was completed at a single urban center hospital with patients presenting to the emergency department, and multiple exclusion criteria that further limit the patient population evaluated in this study. The study on the different criteria used to diagnose AMI needs to be replicated in other settings, with further expansion of the patients for further validity.
Coronary ischemia symptoms, ECG changes, or abnormal angiography/imaging results are required to substantiate AMI diagnosis in the setting of elevated hs-cTnI. Our study demonstrates clinical symptomology is the most useful confirmatory factor in diagnosing AMI.
Declared none.
The authors declare no conflicts of interest, financial or otherwise.
The study was funded by Abbott Diagnostics.

©2021 Modi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.