Journal of
eISSN: 2373-4396


Research Article Volume 2 Issue 6
1Department of Physiotherapy, Sumandeep Vidyapeeth University, India
2College of Applied Medical Sciences, Jazan University, Saudi Arabia
3Department of Physiotherapy, Batra Hospital and Medical Research Centre, India
4Department of Cardiology, India
Correspondence: Faizan Ahmed, Lecturer, College of Applied Medical Sciences, Jazan University, Jazan, Saudi Arabia, Tel 966545382424
Received: April 14, 2015 | Published: June 2, 2015
Citation: Akhtar SA, Ahmed F, Grover S, Srivastava S (2015) Effect of Respiratory Muscle Stretch Gymnastics on Pain, Chest Expansion, Pulmonary Functions and Functional Capacity in Phase 1 Post-Operative CABG Patients. J Cardiol Curr Res 2(6): 00084. DOI: 10.15406/jccr.2015.02.00084
Background: Post operative complications after CABG are a major source of morbidity & mortality& increases hospital stay. Pain level which is experienced with an activity after CABG reduces the functional capacity & QOL. In this study we aimed to effectively reduce post CABG pain and improve respiratory functions in phase 1 post CABG patients with the help of Respiratory Muscle Stretch Gymnastics (RMSG) technique.
Objective: To study the efficacy of combine Phase 1 cardiac rehabilitation & RMSG11 in post CABG patients with pain & impaired pulmonary function in phase 1 post operative CABG patients.
Methods: In a pre test post test experimental study the subjects were randomly assigned to two groups Group A (n=15) performed conventional cardiac rehabilitation and RMSG 3 times/day from 3rd POD to 7th POD of phase 1 cardiac rehabilitation. Group B (n=15) performed only conventional cardiac rehabilitation for same frequency and number of days as above. Following outcome measures PCP, chest expansion, FEV1 and FEV6 were measured by numerical pain rating scale (NPRS), measuring tape and portable spirometer, respectively on 3rd POD and at 7th POD.
Results: There were significant difference of pain intensity occurs in between group (p=0.001). The other respiratory parameters like chest expansion and pulmonary function test did not show any significant change with RMSG. (P> 0.05) Comparison of mean six minute walk distance at the time of discharge was higher in group A (299 ± 16.48 meter) than group B (292.04 ± 13.17 meter), but it was not significant (p =0.185).
Conclusion: The study result shows that inclusion of RMSG in phase 1 cardiac rehabilitation can significantly reduces the post CABG pain and muscle ache around the scapula, and may improves exercise participation of patients as pain reduces.
Keywords: coronary artery bypass grafting, phase 1 cardiac rehabilitation, post-operative CABG pain, respiratory muscle stretch gymnastics, inspiratory muscle Stretching; FEV6
Worldwide cardio-vascular disease is estimated to be the leading causes of death & loss of disabilities– adjusted life style. Coronary artery disease is the 2nd top most life threatening disease in the world.1 Coronary artery bypass grafting (CABG) is a surgical procedure developing during 1960s for the treatment of coronary artery disease.2 Over the years coronary artery revascularization surgery has come to gain importance in the management of IHD.3,4 Current economic situation in health care management is changing rapidly so that post operative hospital stay, patients care and recovery is been important factors and currently being reanalyzed. Post operative complications after CABG can be a major source of morbidity & mortality and may significantly increase the length of hospital stay & resource utilization. Cardiac surgery by its very nature alters pulmonary and cardiac mechanisms5 in the post-operative period.
Pain can keep the patient away from participating in expected activities such as deep breathing exercise, and getting out of bed. Cardiac surgery can be associated with intense post-operative pain 6,7 especially during the first POD 8 & high incidence of chronic sternotomy pain has been reported 9 Post operative chest wall pain can be a major factor that inhibits post-CABG recovery in phase 1 patients. Post-CABG pain (PCP) 4 is believed to be due to the procedure as well as due to the long term post operative recumbent positioning. It has been said that pain level which is experienced with an activity after CABG surgery reduces the functional capacity & QOL.10 The main goal of the exercise component of the phase 1 cardiac rehabilitation is to contour the reconditioning effect of prolonged bed rest and prepare the patients for return to normal daily activities. To achieve this goal, subsidence of post CABG pain and effective exercise participation is necessary. In this study, with the help of Respiratory muscle stretch gymnastics (RMSG) technique,11 we aimed to effectively reduce post-CABG pain and improve respiratory functions in phase 1 cardiac rehabilitation patients. RMSG is a group of stretching exercises sequentially performed to stretch specific muscles involved in respiration. RMSG technique was originally developed to alleviate exercise induced respiratory distress in patients with chronic pulmonary disease by Yamada et al.12
As per the knowledge of the authors of this study there is no existing literature regarding the effects of RMSG technique, in case of CABG patients, on severity of Post-CABG pain, Chest expansion, Pulmonary functions and functional capacity. There exists one study by Aida et al.,13 in which the investigators used a modified form of RMSG on Japanese post-CABG surgery patients. Therefore, the authors of the present study intended to investigate the effects of RMSG, in its unmodified form, on the above mentioned variables.
A total of thirty, male, post-CABG patients with post CABG pain on 3rd post operative day were included in the study. All the subjects were recruited from the Batra Hospital & Research Center, New Delhi, after the institutional ethical clearance. The criteria of inclusion were, subject with age of 40-70 years, post-CABG patients after removal of chest drain, post-CABG pain (PCP),4 cooperative & motivated patients, and Ejection Fraction at least 25% or more.
Procedure
30 Post CABG patients who fulfil above mentioned criteria at 3rd POD, following chest drainage tube removal, were included in study after signing the written informed consent form. The patients were then randomly assigned to either of the two groups i.e. Group A (Experimental group) or Group B (Control group). Each group was assigned 15 patients. Group A patients received exercise component of conventional cardiac rehabilitation (1 session of each exercise, three times daily) and Respiratory muscle stretch gymnastics (2 sessions of five RMSG patterns, 3 times daily) from the 3rd Post-operative day (POD) to 7th POD. Group B patients received only exercise component of conventional cardiac rehabilitation for same frequency and number of days i.e. 1 session of each exercise, 3 times daily, from 3rd to 7th POD. The measurement of dependent variables was carried out at baseline (i.e. 3rd POD) and at post intervention (i.e. 7th POD).
Respiratory muscle stretch gymnastics: A brief description of movement is given below. On the starting day of RMSG rehabilitation, patients learned the 5 pattern by watching a demonstration. Five patterns were used by the therapists. A brief description of the movement is given below.
As you slowly breath in through your nose, gradually elevate both the shoulders. After taking a deep breath, slowly breath out through your mouth, relax and lower your shoulders.
Place both the hands on your upper chest. Pull back your elbows and pull down your chest while lifting your chin and inhaling a deep breath through your nose. Expire through your mouth and relax.
Hold your hands in front of your chest. As you slowly breath in through your nose, Move tour hands frontward and down and stretch your back. After deep inspiration, slowly breath out and resume the original position.
Hold the end of the towel with both hands outstretched at shoulder height. After taking a deep breath, move your arms up while breathing out slowly. After deep expiration, lower your hands and breath normally.
Hold one hand behind your head. Take a deep breath through your nose. While slowly exhaling through your mouth, Stretch your trunk by raising your elbow as high as is easily possible. Return to the original position while breathing normally. Repeat the process using the alternate hand behind the head. (While doing this exercise one hand is used to protect the surgical wound to prevent exacerbating post cabg pain - therapist can also support the wound by himself).
The exercise component of conventional cardiac rehabilitation consisted of: (protocol).
|
Phase 1 POD 1 – POD 7 |
POD |
Exercise |
|
Prescription For phase 1 cardiac Rehabilitation:‐ Intensity: METs–1‐3 METs (gradually increase from 1 POD to 7th POD) |
1st POD Long sitting Intensity : 1‐1.5METs |
a ) Chest prophylaxis |
|
b) Mobilization |
||
|
c) DVT prophylaxis ‐ (Ankle pump exercise) 5‐10 |
||
|
2nd POD |
a + c ‐ Same as above |
|
|
3rd POD |
a ‐ Same as above |
|
|
4th POD |
a ‐ Same as above |
|
|
5th POD |
a + c ‐ Same as above |
|
|
7th POD 3METs |
A ‐ Same as above |
|
|
Before discharge |
a ‐ Same as above |
Protocol Phase 1 of Conventional Exercise Based Cardiac Rehabilitation Protocol
Measurements: Chest circumference was measured at two different levels (axilla and xiphisternum) using a flexible measuring tape.
Placement of measuring tape
a) At axilla level: Anteriorly 3rdintercostal space at mid clavicular line. Posteriorly 5ththoracic spinous process.
b) At xiphisternal level: Anteriorly tip of the xiphoid process. Posteriorly 10ththoracic spinous process.
Severity of pain was assessed using Numerical pain rating scale. Along with that, the location of pain was assessed using the (Figure 1) drawn below.
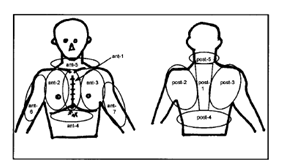
Figure 1 Upper body observational sheet for post operative pain.
*The following anatomical areas are shown in the figure above: ant -1: Median full sternotomy wound; ant 2-3: Intercostals region; ant -4: Epigastrium or drainage extubation; ant -5: Ant .neck region, or central vein drip extubation; ant 6-7: Upper arm region; post -1: Vertebral region; post 2-3: Acrominal process & scapular region; post-4: Lumber region; post-5: Posterior neck region.
PFT values FEV1 and FEV6 were measured using portable spirometer. As FEV6 value is accepted as surrogate for FVC, 14-17 it was measured instead. Functional capacity was measured by 6 Minute walk distance test at 7th POD in both the group.
Data analysis was done using the software package SPSS Version16. Mean values and standard deviation of all the variables were calculated. Paired t test was used for within group analysis. Between groups analysis was done using independent samples / unpaired t test for the difference between the two groups for each dependent variable.
A total of 30 male post CABG patients were included in the study, with a mean age of 56.5 ±6.4 years, and mean Ejection Fraction of 48 ± 10.6%. Table 1 shows demographic details of Mean ± standard deviation (SD) and the level of significance ‘p’ value.
|
|
Mean ±SD |
‘p’ value |
|
|
Experimental Group |
Control Group |
||
|
Age |
56.80 ± 6.899 |
56.20 ± 6.144 |
0.803 |
|
Height |
165.07 ± 10.38 |
162.80 ± 8.58 |
0.520 |
|
Weight |
75.07 ± 14.85 |
72 ± 12.56 |
0.627 |
|
E.F% |
48.33 ± 10.635 |
47.67 ± 10.99 |
0.867 |
Table 1 Demographic description of patient
The mean pain reduction of experimental group (4.93 ± 0.59 to 1.07 ± 0.70) was found to be significantly higher than the control group (4.67 ± 0.61 to 2.40 ± 0.70) (p = 0.001) (Figure 2). Chest expansion
RMSG non-significantly increased chest expansion at both levels, at the axilla from 1.67 ± 0.47 to 2.62 ± 0.42 (p = 0.545) and at the xiphisternal level from 1.64 ± 0.60 to 2.08 ± 0.49 (p =0.945) (Table 2).
|
|
|
Group A |
Group B |
|
|
|
Mean ± SD |
Mean ± SD |
t value |
‘p’ value |
||
|
3rd POD |
Pain |
4.93 ± 0.59 |
4.67 ± 0.61 |
1.206 |
0.238 |
|
CEA |
1.67 ± 0.47 |
1.76 ± 0.39 |
-.583 |
0.565 |
|
|
CEX |
1.64 ± 0.62 |
1.70 ± 0.52 |
-.291 |
0.774 |
|
|
FEV1 |
46.53 ± 14.21 |
50.53 ± 7.39 |
-.967 |
0.342 |
|
|
FEV6 |
47.07 ± 15.44 |
47.73 ± 11.44 |
-.134 |
0.896 |
|
|
7th POD |
pain |
1.07 ± 0.70 |
2.40 ± 0.73 |
-5.06 |
0.001* |
|
CEA |
2.62 ± 0.42 |
2.52 ± 0.46 |
0.613 |
0.545 |
|
|
CEX |
2.08 ± 0.49 |
2.10 ± 0.55 |
-.070 |
0.945 |
|
|
FEV1 |
65.07 ± 14.06 |
66.47 ± 10.29 |
-.311 |
0.758 |
|
|
FEV6 |
72.53 ± 13.06 |
66.87 ± 11.071 |
1.282 |
0.210 |
|
Table 2 Comparison of mean pain, chest expansion and pulmonary function values between groups
(Significance level: p<0.05). CEA: Chest Expansion at Axilla; CEX: Chest Expansion at Xiphisternal; FEV1: Forced Expiratory Volume In 1 Second; FEV6: Forced Expiratory Volume In 6 Second (Level of significance: P < 0.05)*
Pulmonary function & exercise capacity
The pulmonary function test value measured at 3rd POD shows that there was no significant difference between the two groups. On the 7th Post operative day, the mean improvements in FEV1 and FEV6 in experimental group were 18.54 % and 25.46%, respectively, and in the control group 15.94% and 19.14% respectively. Both the values showed improvement in the experimental group however they were not found to be statistically significant. ‘p’ value for FEV1 & FEV6 was 0.75 & 0.21 respectively. Comparison of mean 6MWT values at discharge between the experimental group (299.46 ± 16..48 meter) and the control group (292.04 ± 13.17 meter) using independent sample ‘t’ test shows that the mean 6 Minute Walk distance was improved in experimental group but the difference was not significant ( P = 0.185).
Acute Post CABG pain represents a significant health problem that may impact negatively on quality-of-life issues and healthcare costs after CABG surgery. Postoperative chest wall pain (PCP)4,8 and discomfort may be the major factor that inhibit post CABG recovery and increase length of hospitalization. Previously PCP has been treated by advanced method of analgesia or other relaxation technique18–20 but there are limited numbers of studies to relieve PCP by more active method such as facilitating recovery of the natural functions of respiratory muscles.
The results of the present study show that RMSG significantly reduced chest wall pain (PCP) and muscle ache around scapula, but the other variables under investigation i.e. respiratory parameters did not significantly change. A significant difference was found in the severity of pain between the two groups (p= 0.001) (Figure 3 & 4). In an earlier study, Miller KM investigated the effectiveness of slow deep breathing relaxation technique to relieve post CABG pain, they concluded that significant decrease were observed on the visual descriptor scale, but the same observations were not true when using the visual analogue scale. In the present study, a significant difference in numerical pain rating scale after application of RMSG followed by deep breathing exercise was observed. The reason for the difference in the results may be that the respiratory muscle stretching & deep breathing, both the component of RMSG, would be the possible mechanism of pain relief and relaxation in post CABG patients.

Figure 3 Comparison of mean chest expansion value.
3CEA, chest expansion at axilla level 3rd POD; 7CEA, chest expansion at axilla level at 7th POD; 3CEX, chest expansion at xiphisternal level at 3rd POD; 7CEX, chest expansion at xiphisternal Level at 7th POD
In another study, Aida et al.,13 who used modified RMSG13 to alleviate PCP, observed that pain was reduced significantly (p=0.049). Similar findings were observed in the present study, but with a higher level of significance (p=0.001). This may indicate that that the original RMSG11 technique may have greater amount of pain reduction in Phase 1 Post CABG patients compared to the modified RMSG13technique shown and used by Aida et al.13 However, the same needs to be investigated with the help of a randomized controlled trial. The observed significant difference in experimental group shows that stretching exercise, in form of RMSG,11- as an alternative method of pain relief along with conventional cardiac rehabilitation & pain medication could be more effective to alleviate post CABG pain, reduced muscle ache around scapula and increase the degree of movement than only conventional cardiac rehabilitation exercise & pain medication. As results of low state of fitness and the adverse effects of bed rest and surgery on the musculoskeletal system of the cardiac patients, there is need for special stretching and joint readiness exercise during phase 1. Due to surgical trauma to the muscles and bones of the upper body, these areas may become atrophied and are vulnerable to the development of adhesions. Upper extremity ROM and stretching exercises may enhance blood flow to the damaged areas and accelerate the tissue repair. In addition stretching may enhance flexibility, thereby preventing the development of undue weakness and poor posture.
The main purpose of phase 1 cardiac rehabilitation is to contour the reconditioning effects of prolonged bed rest and prepares the patients for a return to normal daily activities. But one of the main factors which may cause hindrance to this purpose is PCP. Thus, the overall results of study indicate that inclusion of RMSG in cardiac rehabilitation for the purpose of pain relief would be more desirable technique to achieve the goal of phase 1 cardiac rehabilitation.
Comparison of Mean chest expansion values at axilla and xiphisternal level showed no significant improvement in the values of chest expansion (p > 0.05 at both levels) (Table 3). Our study results of RMSG on post CABG phase 1 found some contradictory results to Minogushi et al.,21 study of RMSG on COPD patients. They found that 4 weeks (3 session of 5 RMSG pattern 4 times each day) of RMSG technique in COPD patients improved chest expansion at all 3 levels. While our study population is from the intensive care unit and we used RMSG technique only for 5 days (1 session of 5 RMSG pattern 3 times each day). Possible reasons behind limited improvement in chest expansion in all 30 patients would be the shorter treatment duration and midsternotomy pain.
|
Group |
Group A |
Group B |
‘t’ test |
|
|
Mean ± SD |
Mean ± SD |
t |
‘p’ |
|
|
7th POD |
299.46± 16.48 |
292.40± 13.17 |
1.36 |
0.185 |
Table 3 Comparison of mean 6MWT between groups (Significance level: P < 0.05)
As the patients of CABG had undergone medial sternotomy operation, so they used avoid to take deep breaths as they had severe pain with diaphragm and thoracic cage movement, so the chest expansion reduced dramatically immediately after median sternotomy incision. The results of our study reveal that, the chest expansion at both level increased gradually along with the significant reduction of pain from 3rd POD to 7th POD, but the difference was statistically insignificant.
The study results concluded that The RMSG stretching technique may reduce chest wall stiffness as maximum chest expansion value of experimental group is higher than that of control group but RMSG is not effective to significantly increase the chest wall expansion in post CABG phase 1 patients in a limited number of days. From the results of our study, it seems that RMSG may not have beneficial effect in context with chest expansion.
Between group analysis of experimental and control group showed, there were no significant difference observed in FEV1% (p=0.758) & in FEV6 % (p=0.210) value at 7th POD (Table 2). Pulmonary functions are often diminished after surgery as results of the combined effects of anesthesia, bed rest and a reluctance to breathe deeply because of sternal discomfort. In the present study, the effect of RMSG on pulmonary function could not be verified because post CABG patients are in a state of transient and mechanical restrictive impairment due to sternal pain. Our results are similar to Minoguchi et al.,21 2002, who did 4 weeks study on relationship of RMSG with COPD & found that, no significant difference in FEV1% values in COPD patients. Study by Aida on CABG patients using Modified RMSG on CABG failed to show statistically significant difference in FEV1 % value. We noted in the present study that the possible reasons for limited improvement in FEV1 % and FEV6 % would be the short post operative stay & intervention (i.e. of 5 days treatment, 15 session of RMSG) and small subject population (30 patients). Other important reason for the poor effort of patients was Post sternotomy pain and fear of dehiscence of sternal suture with forced expiratory maneuver performed during pulmonary function testing. Through individual group analysis we observed that there were significant improvement of both FEV1% & FEV6 % value at 7th POD compared with 3rd POD.
The results of our study shows that the additional respiratory muscle stretching exercise in form of RMSG has no impact on walk distance (p > 0.05). Mean distance walked in experimental and control group was (299.46 ± 16.48 meter) (292.04 ± 13.17 meter) respectively. The higher reduction of pain and improved exercise participation would be the possible reason for greater walk distance in experimental group than control group. The additional mean distance walked in experimental group was near about 8 meters, so we cannot assert that it would be because of effect of RMSG. So the overall results of study shows, inclusion of RMSG in cardiac rehabilitation for the purpose of post CABG pain relief, would be more desirable technique to achieve the goal of phase 1 cardiac rehabilitation. The stretching techniques are simple to execute, and patients adapt it easily.
The present study suggest that inclusion of RMSG in phase 1 cardiac rehabilitation can significantly reduces the post CABG pain and muscle ache around the scapula. Exercise participation of patients may improve with reduced pain.
None.
The authors state that there is no conflict of interest.
None.

©2015 Akhtar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.