Journal of
eISSN: 2373-4396


Case Report Volume 11 Issue 4
1General Practitioner, Medical Department, Rashid Hospital, UAE
2Specialist Senior Registrar, Department of cardiology, Rashid Hospital, UAE
Correspondence: Akram Jehad Al Rishani, Specialist Senior Registrar, Department of cardiology, Rashid Hospital, UAE
Received: August 18, 2018 | Published: August 27, 2018
Citation: Al Zainal JH, Rajani AL, Al Rishani AJ. Coronary artery venous fistula: a rare cause of STEMI in a young female. J Cardiol Curr Res. 2018;11(4):194-196. DOI: 10.15406/jccr.2018.11.00397
A 25-year-old young woman, who is an immigrant with a long history of exertional chest pain for which she never sought medical advice, presented to the emergency department of our institute complaining of left sided chest pain radiating to the jaw and left shoulder. She was admitted as a case of Inferior wall ST-elevation myocardial infarction (STEMI). After a short period of time in the emergency room, the pain resolved and the ECG was not fulfilling the criteria for thrombolysis. It was only during the coronary angiography procedure that we discovered a fistula from left anterior descending coronary artery (LAD) draining directly into the right ventricle (RV), which is considered to be the culprit for her symptoms.
Coronary arteriovenous fistulas (CAVFs) are a collection of rare congenital anomalies, where a fistula arises as a result of direct communication between a coronary artery and a cardiac chamber, coronary sinus, the pulmonary artery or the superior vena cava while the other coronaries’ number, origin and course are normal1,22 We report a case of young female with a congenital fistula arising from the LAD into the RV, presenting as a case of inferior MI.
In this report, we present to you a 25-year-old presumably healthy female, an immigrant with long history of on-off atypical, exertional chest pain for which she did not seek medical advice. She is working as a teacher in a secondary school with no history of smoking or alcohol consumption. She attended our facility with symptoms of moderate chest pain radiating to jaw and left shoulder while she was at work. Her first ECG showed ST segment elevation in inferior leads (Figure 1). After a short time, the pain resolved and the ST segment has settled in the next ECG which was not fulfilling the criteria for thrombolysis (Figure 2). She had a similar episode of chest pain three days prior to admission, which resolved spontaneously. She had no complaints of dyspnea, palpitation or dizziness. She is allergic to paracetamol. On physical examination, she was vitally stable with blood pressure of 115/66 mmHg in sitting position, afebrile (37°C) and maintaining oxygen saturation of 100% on room air. She was however tachycardic with resting heart rate of 105 beats per minute. Upon auscultation, chest examination was clear with equal bilateral air entry. The cardiovascular examination was negative for any additive sounds.
The first ECG recording on presentation showed a 1mm ST segment elevation in the inferior leads and V5-V6 (Figure 1). The serial ECGs after, showed resolution of ST segment elevation with no other ST-T wave changes (Figure 2). By the time she was referred to the cardiology on call, there was no indication for thrombolysis as she was pain free and her ECG was not showing STEMI, which is why she was started on conservative management as a case of aborted inferior STEMI.
Laboratory readings showed a positive troponin at 0.05 ng/mL which later rose to 0.88 ng/mL, yet her other cardiac markers were initially negative then they rose up [Creatine Kinase 122 U/L then 479 U/L; Creatine Kinase-MB 9 U/L then 60 U/L]. All other readings from blood urea, electrolytes to kidney function were within normal limits. Pregnancy was ruled out. The suspicion of a pulmonary embolism was cut with a D-dimer of 0.11 mg/L.
Transthoracic Echocardiography showed a good left ventricular ejection fraction of 60% with no significant regional wall motion abnormality. During the coronary angiography, she was found to have a dilatation in the left main stem extending to the mid-segment of the LAD. (Figure 3) (Figure 4).
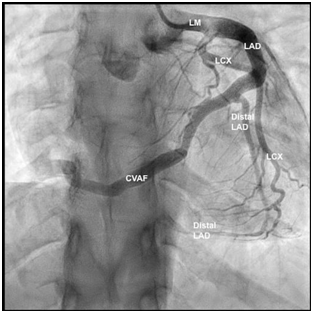
Figure 3 Coronary angiography: Straight antero-posterior view: Dilatation of the left main (LM) stem extending to the proximal and mid- left anterior descending artery (LAD). The coronary arteriovenous fistula (CVAF) originating from distal LAD. Type III LAD wrapping around the left ventricular apex, supplying the apical two-thirds of infero-posterior wall.
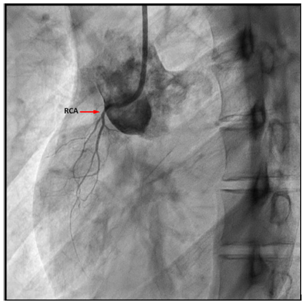
Figure 4 Coronary angiography: Straight Right anterior oblique view: Rudimentary right coronary artery (RCA).
There was an arterio-venous fistula, arising from the distal LAD with an unclear drainage end into the right heart chambers (Figure 3) (Figure 4). There was a slow flow in the distal LAD beyond the fistula origin. Her LAD was type III, wrapping around the left ventricular apex, supplying the apical two-thirds of infero-posterior wall. The right coronary artery (RCA) was rudimentary and the left circumflex artery (LCx) was normal. To further study these abnormalities, she was scheduled for CT Coronary Angiogram which revealed a fistula arising from the distal LAD and courses anteriorly on the right ventricle measuring 3.3 mm just after its origin from the LAD, terminating into the superior aspect of the right ventricle (RV). The terminal part of the AV measures 11.8 mm (Figure 5) (Figure 6). The rest of the coronary findings were matching those seen in the conventional coronary angiography.
The patient was started on the standard anti-anginal treatment with no recurrent chest pain during her hospitalization. After discussion in the heart team meeting with the cardiothoracic surgeons and the patient, she was offered both options for AV fistula closure: either percutaneously or surgically. The patient however, opted to receive full treatment in her home country. She was discharged home with aspirin 75 mg, bisoprolol 5 mg, Clopidogrel 75 mg, pantoprazole 40 mg and nitroglycerine spray and advised to follow up with a cardiologist to have the corrective procedure done.
She was discharged in a stable condition and advised to go for coronary fistula closure.
Coronary arterio-venous fistula (CAVF) were first classified by Odgen, as a major coronary anomaly, being present in 0.002% of the general population with majority of cases having a congenital origin (0.4%). They were first described by Krause in 18653,4 E. D. Fernande et al.,5 classified these oddities according to their site of origin, termination and distribution. Coronary artery fistulas are anomalies of termination, where the most common site of vessel-origin draining into the right ventricle are the right coronary artery (RCA) in 60% of the patients, left anterior descending (LAD) in 21% and the circumflex (LCX) in 9.5%.5
Patients with coronary fistulas are considered “hemodynamically significant”, as half of them present with congestive heart failure, subacute bacterial endocarditis, myocardial ischemia or infarction as a response to the “steal phenomenon” or rupture of an aneurysm.6,7 The golden standard of diagnosis and confirmation of the CAVFs is a coronary angiography procedure.5–8 Our patient had significant hemodynamic changes bringing about her symptoms of angina which, with investigations, marked her as a case of inferior STEMI, for which she was offered the optimal treatment.
Multiple cases were reported of CAVF. Darawzah et al.,8 published the case of a 51-year-old gentleman with multiple comorbidities, presenting to the emergency department with typical chest pain associating with sweating and nausea who was later diagnosed as anterior myocardial infarction. During angioplasty, a fistula originating from the circumflex artery and terminating into the pulmonary artery.8
Fennich et al.,9 discuss the case of a middle-aged gentleman presenting with complaint of chest pain. His electrocardiogram recording was positive for Q waves on the inferior leads and peaked T waves on the anterior leads. His coronary angiogram displayed a fistula originating from the right coronary artery, having dual draining sites: a) into the right ventricle b) coronary sinus. Another case reviewed is that of a 12-year-old girl presenting with febrile bronchitis and an acute onset of chest pain. Her coronary angiography showed an important vessel arising from the proximal left anterior descending artery draining into the right ventricle.
To this day, there are two approaches for ligation of the CAVFs: Trans-catheter ligation -indicated when the vessels involved in the fistula are non-tortuous, accessible distally, with a narrow distal end and there are no other clear indications for surgical intervention.10 The other option is the surgical ligation, which was first described by Bjork11 and has been considered the golden standard of treatment.
None

©2018 Al, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.