Journal of
eISSN: 2373-4396


Research Article Volume 6 Issue 6
Military Hospital, Tunis, Tunisia
Correspondence: Rim Ben Said, Military Hospital, Tunis, Tunisia
Received: May 29, 2016 | Published: October 31, 2016
Citation: Said RB, Jedaida B, Mimouni M, Dahmani R, Gommidh M, et al. (2016) Cardiogenic Shock Complicating Acute Myocardial Infarction. J Cardiol Curr Res 6(6): 00230 DOI: 10.15406/jccr.2016.06.00230
Background: Cardiogenic shock (CS) is still the leading cause of in-hospital mortality in patients presenting with acute myocardial infarction (AMI).
Aim: To investigate the epidemiological and clinical characteristics of a series of patients hospitalized for AMI complicated by CS and to determine the in-hospital mortality.
Methods: We retrospectively analysed 70 patients affected by AMI complicated by CS admitted to cardiology department of the military hospital between October 2005 and April 2015.
Results: A total of 70 patients were included in the study, 56 (80%) patients were male. The mean age was 63±10years. Diabetes mellitus (62%) and hypertension (50%) were the predominant risk factors. On admission, 41% of patients were in left ventricular failure and 59% in shock. The mean LVEF was 49±14.4%. Thrombolysis was performed in 51% of patients. Seventy-two (72%) of patients underwent angiography and 56.6% had percutaneous coronary intervention (PCI). Of these, 27% were taken for primary PCI and 73% had rescue PCI. Revascularization was complete in 37% of cases. The success rate of PCI was 85%. The average of hospital stay was 7±8days. Patients revealed a mortality rate of 47%, occurring on average in the 6th day of hospitalization. We found that renal failure (p=0.014), late onset of shock (p=0.031), hyperglycemia (p=0.014), leukocytosis (p=0.02), use of vasopressors (p=0.003), and the anterior territory of MI (p=0.003) were significantly predictive of hospital mortality.
Conclusion: Despite significant advances in the treatment of myocardial infarction, the in-hospital mortality of patients in CS complicating MI remains high. Renal failure, late onset of shock, hyperglycemia and the anterior territory of MI were the major predictive of hospital mortality. A multidisciplinary approach including medical actors and pre-hospital centers specialized in the treatment of this condition is actually necessary.
Keywords: cardiogenic shock, myocardial infarction, mortality, prognosis
CS, cardiogenic shock; AMI, acute myocardial infarction; PCI, percutaneous coronary intervention; STEMI, st-elevation myocardial infarction; NSTEMI, non-st-elevation myocardial infarction; SD, standard deviation; IABP, intra-aortic balloon pump; NRMI, national registry of myocardial infarction
Although numerous clinical complications are associated with the development of acute myocardial infarction (AMI), none are more potentially devastating or carry a worse prognosis than cardiogenic shock (CS). It’s the leading cause of death in patient hospitalized with AMI and continues to complicate between 5-8% of ST-elevation myocardial infarction (STEMI) and approximately 2.5% of non-ST-elevation myocardial infarction (NSTEMI) cases.1,2 Mortality from CS remains highand reaches 70-80% in those treated conservatively,3 despite marked advances in the treatment of AMI. The aim of our study was to investigate the epidemiological and clinical characteristics of a series of patients hospitalized for AMI complicated by CS as well as to recognize the predictive factors of early mortality.
We retrospectively analysed 70 patients affected by AMI complicated by CS admitted to cardiology department of the military hospital between October 2005 and April 2015. AMI was defined as typical chest pain for more than 30min and significant ST-elevation in 2 or more leads. We used the following clinical criteria for CS: systolic blood pressure (SBP) <90mmHg in the absence of hypovolemia and associated with evidence of hypoperfusion (cyanosis, cold extremities, changes in mental status, persistent oliguria, or congestive heart failure), pulse>100bpm and reduction in the cardiac index <2.2l/min/m². Patients in whom AMI was not confirmed or with non-cardiac shockwere excluded from the analysis.
All relevant data including demographic, clinical, in-hospital treatment, and outcome characteristics of the patients were recorded. Diagnosis of the different definitions of data variables were based on the ACC clinical data standards.4 The follow up of patients was until 6months after discharging. All statistical analyses were performed using SPSS Statistics version 20. Continuous variables were summarized as a mean± standard deviation (SD). Comparisons between two groups were performed with a t-test for continuous variables. Comparisons between two groups were performed with the chi-square test for categorical variables. A p-value of <0.050 was considered statistically significant.
A total of 70 patients were included in the study: 56(80%) patients were male and 14 (20%) were female. The mean age was 63±10years (range: 40-85years). Cardiovascular risk factors were as follows: 89% were smokers, 62% presented diabetes mellitus, 50% had hypertension, 40% had dyslipidemia and 10% had a family history of coronary artery disease. 24% of patients had renal insufficiency.
Thirty-nine percent were admitted before the 6thhour from the onset of the chest pain, 12% were admitted between the 6th and the 12thhour and 45% were admitted beyond the 12thhour. The clinical data are summarized in the (Table 1 & 2). On admission, 41% of patients were in left ventricular failure and 59% in shock. The majority of myocardial infarction (45%) were anterior followed by inferior infarction with extension to the right ventricle (34%). The mean LVEF was 49±14.4%: mean LVEF was 37.8% in anterior MI and 57.6% in inferior MI.
|
Variable |
Number (%) |
|
Meanage (years±SD) |
63 |
|
Men |
56 (80%) |
|
Women |
14 (20%) |
|
Hypertension |
5 (50%) |
|
Diabetes |
44 (62%) |
|
Dyslipidemia |
28 (40%) |
|
Smoking |
62 (89%) |
|
Family History of CAD |
7 (10%) |
|
Renal Insufficiency |
17 (24%) |
Table 1 Patient Characteristics
|
Variable |
Number (%) |
|
Mean HR (bpm) |
92 |
|
Mean SBP (mmHg) |
81 |
|
Mean RR (cycle/min) |
23 |
|
Mean Arterial Saturation in O2 |
89% |
|
Signs of Hypo Perfusion Organs |
45 (64%) |
|
Mechanical Ventilation |
11 (15%) |
|
Anterior MI |
32 (45%) |
|
Inferior MI with Right Extension |
24 (34%) |
Table 2 Clinical data
HR: Heart Rate; SBP: Systolic Blood Pressure; RR: Respiratory Rate; MI: Myocardial Infarction
Thrombolysis was performed in 51% of patients, 57% of them had thrombolysis before the 6thhour. The thrombolytic agent used was Metalyse. Seventy-two (72%) of patients underwent angiography and 56.6% had percutaneous coronary intervention (PCI). Of these, 27% were taken for primary PCI and 73 % had rescue PCI. Angiography had identified a single-vessel diseasein 28% of cases, double-vessel disease in 44% of cases and multi-vessel disease in 28 % of cases. Revascularization was complete in 37% of cases. The success rate of PCI was 85%. The majority of stents used were bare stents (83%). Forty nine of patients (70%) needed inotropic agents: 43 of patients had dobutamine, 17dopamine and 9 noradrenaline. An intra-aortic balloon pump (IABP) was used in two patients with a mean duration of 2days.
The average of hospital stay was 7±8days. In-hospital outcome of the study, patients revealed a mortality rate of 47%, occurring on average in the 6thday of hospitalization. We found that renal failure (p=0.014), late onset of shock (p=0.031), hyperglycemia (p=0.014), leukocytosis (p=0.02), use of vasopressors (p=0.003), and the anterior territory of MI (p=0.003) were significantly predictive of hospital mortality.
The mean age of our study population was 63years, which was lower than studies reported from the United States (69.4±12.7years).5 Most patients were male (80%) which is comparable to other studies. This may be because MI is more common in men than in women. Among the risk factors, diabetes was most prevalent at 62%, which is higher than previous studies (range=29-35%).5,6 This high prevalence of diabetes is alarming as it is well known that diabetic patients have poor hospital outcomes.7 Hypertension was at 50% which was similar to the prevalence in the SHOCK “Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock” study (53%).8
In our study, 59% of patients were in CS at admission and 41% developed it secondary. However in the SHOCK trial, only 15% were in shock at admission.8 This high prevalence in our study may be due to the delay that patients took to consult after the onset of chest pain. The incidence of anterior wall STEMI was nearly 50%. Garcia-Alvarez et al.,9 reported that 68% of their patients had anterior STEMI. Infarctions were located anteriorly in most patients (55%) in the SHOCK trial registry (Figure 1).8 We found also that the anterior wall STEMI was a strong predictive factor of intra-hospital mortality (Table 3). Our results are similar to other populations suggesting that extensive myocardial damage from anterior infarction is the predominant cause for CS. Early revascularization is the cornerstone treatment of AMI complicated by CS. Thrombolytic therapy was used in almost 51% of patients in this study. Another study reported a similar figure of 69%.10 However, thrombolysis is efficient when it’s used before the 6th hour, later, results became poor.11
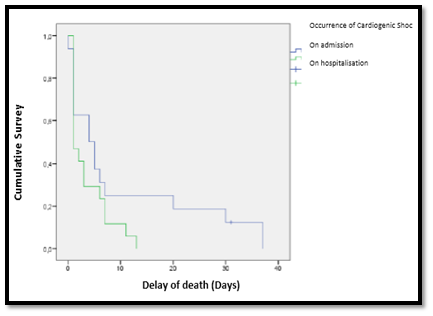
Figure 1 Survival curves.
Intra-hospital mortality is higher in patients presenting shock secondary during hospitalization comparing to patients with shock at admission.
|
Predictive Factors of Intra-Hospital Mortality |
Anova P |
|
Age |
0.57 |
|
Gender |
0.9 |
|
Hypertension |
0.71 |
|
Diabetes |
0.67 |
|
Dyslipidemia |
0.35 |
|
Smoking |
0.66 |
|
Renal Insufficiency |
0.014 |
|
Anterior Wall of Infarction |
0.003 |
|
Arrhythmia |
0.37 |
|
FEVG |
0.004 |
|
Inotropic Agent |
0.003 |
|
Glycaemia |
0.014 |
|
CRP |
0.06 |
|
Troponine |
0.44 |
|
Hemoglobin |
0.11 |
|
Leucocytes |
0.02 |
Table 3 Predictive factors of intra-hospital mortality
Hence, the primary PCI strategy, as mentioned in the ACC/AHA and ESC guidelines,12 should be adopted: it’s is the most efficient therapy to restore coronary flow in the infarct- related artery. The GUSTO-I investigators13 found that while PCI was performed in only 19% of the 2972 patients with CS, this translated into a mortality rate of 31% compared with 61% for patients who did not undergo dilation. The superiority of PCI compared to fibrinolysis is due to more effective restoration of coronary patency and less coronary reocclusion.
Intra-aortic balloon pump (IABP) was used in 2 patients and did not show any significant mortality benefit which is similar to other meta-analysis.14 We observed in our study high in-hospital mortality in patients presenting with CS. However, the in-hospital mortality observed (47%) was similar to other studies, which was reported between 40–50%.15 The US National Registry of Myocardial Infarction (NRMI) data showed in-hospital mortality of 47.9%.6
One predominant reason in ourstudy for high mortality could be non-availability of the catheterization laboratories, and the subsequent delay in transfer of patients to our hospital for intervention. In the United States, Shaefi et al.,16 stratified hospitals according to the number of CS volumes per year and showed that in-hospital mortality decreased from 41% to 37.01% in hospitals with higher CS case volumes.
A study conducted in Spain reported significant LV systolic dysfunction (about 25±10%) in the CS no survivor group (Figure 2). They also found multi vessel disease in 25% of cases and left main involvement in 12% cases.9 The IABP-SHOCK II-trial showed that overall EF was about 25%, and left main involvement was 9%.17 These findings are similar to our study, where in the majority of patients having severe LVsystolic dysfunction especially when it was an anterior wall and left main disease, which may have led to high mortality in this study. In the NRMI registry, of the 340 CS patients enrolled, 163 (47.9%) died. Among the expired CS patients, 74 (33.9%) underwent revascularization by PCI, and 63 (34.1%) patients had primary PCI.6
In the IABP-SHOCK II trial, 96% of patients underwent PCI (Figure 3). Cardiac mortality was 50%.5 The high mortality rate in these two large registries indicates that even if PCI is done in these high-risk CS patients mortality remains high at about 50% which is similar to our analysis. We found that renal insufficiency is a predictive factor of mortality which is concordant with Koreny‘s study.18 Finally, CS is the result of temporary or permanent derangements in the entire circulatory system and the primary goal in preventing CS is to reduce the time to effective treatment, because of the fact that early reperfusion limits ongoing necrosis and salvages myocardium. The SHOCK trial8 demonstrated a steady fall in hospital mortality of CS patients, and a significant survivor benefit for those treated with revascularization at six months.
Our data lacked information on the time from onset of CS to revascularization, which has an effect on mortality. Other variables associated with mortality after PCI, such as ST-segment resolution, myocardial blush grade, thrombolysis in myocardial infarction flow grade, and hemodynamic data were not studied. We had a small number of patients in this study, which may not lead to conclusive results.
Despite significant advances in the treatment of myocardial infarction, particularly reperfusion techniques, and therapeutic drug in intensive care units, the in-hospital mortality of patients in CS complicating MI remains high. Renal failure, late onset of shock, hyperglycemia and the anterior territory of MI were the major predictive of hospital mortality. A multidisciplinary approach including medical actors and pre-hospital centers specialized in the treatment of this condition is actually necessary.
None.
Author declares there are no conflicts of interest.
None.

©2016 Said, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.