Journal of
eISSN: 2373-4396


Commentary Volume 16 Issue 3
Department of Medicine, NHS the UK and Mansoura University, Egypt
Correspondence: Ahmed N Ghanem, Faculty of Medicine, Department of Urology, Mansoura University, Retired Consultant Urologist Surgeon, No1 President Mubarak Street, Mansoura 35511, Egypt, Tel 00201020883243
Received: June 02, 2023 | Published: June 15, 2023
Citation: Ghanem ANM. Acutely ill patients suffering ARDS with massive, generalized oedema: Are they in a state of hypo- or hypervolemia? J Cardiol Curr Res. 2023;16(3):71-73. DOI: 10.15406/jccr.2023.16.00581
I read with great interest this recently published article by Professors Dull, R.O. and Hahn, R.G.1 The authors are commended on this review based on evidence from published reports that represent the current understanding of the condition and its scientific basis. The authors have faithfully and factually summarized the evidence based on published reports, including some of the commonly received errors and misconceptions on the scientific foundation2 that identifying and correcting may help answer the vitally important question in the report's title. I asked myself the very same question “What is wrong?” after attending the post-mortem examination of 3 patients who were killed by ARDS, complicating the TUR syndrome back in 1981. It took me >40years of hard, comprehensive, intensive, and profound scientific research to find the correct answer.
The authors acknowledge that Starling’s law represents the scientific foundation of the volume-pressure relationship of the vascular, capillary, and interstitial fluid compartments. It thus underlies and dictates the rules that govern fluid therapy in shock management. This is the subject on which both authors are among the top world authority. My research has demonstrated clearly and completely the substantial evidence that Starling’s law is wrong, and the correct replacement is the hydrodynamics of the porous orifice (G) tube3 that has been gathered in a book.4 This will revolutionize our understanding of the condition and related issues, particularly on the path-etiology and management of ARDS. The hydrodynamics of the G tube in a surrounding chamber mimics the capillary-interstitial fluid (ISF) transfer (Figure 1).
Keywords: shock, fluid therapy, ARDS, starling’s law, oedema, hypovolaemia, Hypervolaemia, vascular pressure, and volume
ARDS, acute respiratory distress syndrome; TUR, syndrome transurethral resection of the prostate syndrome; G tube, porous orifice tube; ISF, capillary-interstitial fluid; VO, volumetric overload; VOS 1, volumetric overload shock type 1; VOS 2, volumetric overload shock Type 2; AKI, acute kidney injury; MODS, the multiple organ dysfunction syndrome; CVP, central venous pressure; NaCl, sodium chloride; NaCo3, sodium bicarbonate; HST, hypertonic sodium therapy
I read with great interest this recently published article by Professors Dull, R.O. and Hahn, R.G.1 The authors are commended on this review based on evidence from published reports that represent the current understanding of the condition and its scientific basis. The authors have faithfully and factually summarized the evidence based on published reports, including some of the commonly received errors and misconceptions on the scientific foundation2 that identifying and correcting may help answer the vitally important question in the report's title. I asked myself the very same question “What is wrong?” after attending the post-mortem examination of 3 patients who were killed by acute respiratory distress syndrome (ARDS), complicating the transurethral resection of the prostate (TUR) syndrome back in 1981. There was massive tissue oedema with swollen vital organs and 3 litres of fluid in each of the peritoneal and pleural cavities. They were literally internally drowned by fluids infused for the resuscitation of shock. I asked the pathologist why he does not mention that in his report. His reply was: “Because it offends the treating physicians”! It took me >40 years of hard, dedicated, comprehensive, and intensive scientific research to find the correct answer.
The authors acknowledge that Starling’s law represents the scientific foundation of the volume-pressure relationship of the vascular, capillary, and interstitial fluid compartments. It thus underlies and dictates the rules that govern fluid therapy in shock management. This is the subject on which both authors are among the top world authority. My research has demonstrated clearly and completely the substantial evidence that Starling’s law is wrong, and the correct replacement is the hydrodynamics of the porous orifice (G) tube3 that has been gathered in a book.4 This will revolutionize our understanding of the condition and related issues, particularly on the path-etiology and management of ARDS. The hydrodynamics of the G tube in a surrounding chamber mimics the capillary-interstitial fluid (ISF) transfer (Figure 1).
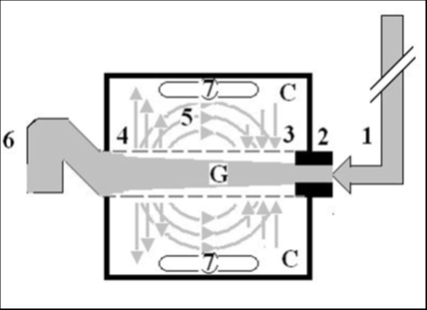
Figure 1 Shows a diagrammatic representation of the hydrodynamic of G tube based on G tubes and chamber C. This 38-years old diagrammatic representation of the hydrodynamic of G tube in chamber C is based on few photographs. The G tube is the plastic tube with narrow inlet and pores in its wall built on a scale to capillary ultra-structure of precapillary sphincter and wide inter cellular slit pores. The chamber C around it is another bigger plastic tube to form the G-C apparatus. The chamber C represents the ISF space. The diagram represents a capillary-ISF unit that should replace Starling’s law in every future physiology, medical and surgical textbooks, and added to chapters on hydrodynamics in physics textbooks. The numbers should read as follows:
“Hypovolaemia and peripheral oedema” refer to the condition that affects acutely ill surgical patients presenting with any shock then suffer clinically with ARDS induced by excessive fluid therapy in whom there is massive volumetric overload with hypotensive shock (Hypovolaemia?) and massive fluid creep on the interstitial fluid space causing generalized oedema. It complicates fluid therapy for shock resuscitation of burns, sepsis, haemorrhage, trauma, and acute pancreatitis.5,6 It initially presents and seamlessly occurs as volume kinetic or volumetric overload shock (VOS)7 among new scientific discoveries in physics, physiology, and medicine.8 It has high morbidity and mortality and affects thousands of patients every year all over the world. Although there is hypotensive shock here, it is probably incorrect to assume “hypovolaemia” exists. In other words, and contrary to what is generally believed, hypotension is not synonymous with hypovolaemia. It is a simple physics: if the cardiovascular system is overfilled to above its maximum capacity, the surplus fluid will simply spill into the ISF space!
Starling’s law has proved wrong on both of its hydrostatic and oncotic pressure forces3 However, it continues to dictate the current faulty rules on fluid therapy in the management of shock. It thus misleads physicians into giving too much fluid during shock resuscitation.9 More than 21 reasons were reported to show that Starling’s law is wrong.10 The correct replacement is the hydrodynamic of the porous orifice (G) tube (Figure 1) that was built on the capillary ultrastructure anatomy of the precapillary sphincter11 and a porous wall12 that allows the passage of plasma proteins thus nullifying the oncotic pressure in Vivo. It follows that the extended Starling Principle is wrong, and a misnomer, and all the equations are also wrong. Com¬monly received but erroneous concepts and laws represent fraud in modern science.
The clinical significance is that Starling’s law dictates the faulty rules on fluid therapy causing many errors and misconceptions that mislead physicians into giving too much fluid infusions of albumin and crystalloids for the resuscitation of shock9 which both cause oedema of ISF space and vital organs as well as “hypervolemia” with hypotension.7,15 This shock is mistaken for septic shock or any known shock and is wrongly treated with further huge volume expansion, occurring with both liberal and conservative approaches of fluid therapy. This has been newly recognized as volume kinetic or volumetric overload shocks (VOS).7,15
Volumetric overload inducing VOS is of 2 types: VOS 1 is induced by sodium-free fluid such as 1.5% Glycine, 5% Glucose, 3% Mannitol, and Sorbitol fluids that cause the TUR syndrome13 which has a lifesaving therapy now.14 VOS 2 is induced by sodium-based fluids of crystalloids and plasma proteins and causes ARDS and acute kidney injury (AKI) as part of the multiple organ dysfunction syndrome (MODS) with high morbidity and mortality.15 VOS 2 may complicate VOS 1 or occur de novo. Volumetric overload shock induced by persistence to elevate CVP to a high level of 20-22 mmHg during shock resuscitation is also based on the faulty Starling’s law and induces ARDS that was originally reported by Ashbaugh et al in 1967 in which the dead patients had 12-14 Litres of fluid creep retained in their bodies.16 In recent huge prospective multicentre clinical trial studies, fluid retention is 7-10L in surviving ARDS patients.17
I trust the respected authors, and invite the world authorities, to kindly fulfill their authority and responsibility by writing an update on the subject that summarises the results of my recently reported research for the awareness of the doctors’ readers and the undoubted benefit of their patients. Fortunately, the treatment is currently available which is hypertonic sodium therapy (HST) of 5% NaCl and 8.4% NaCo3 that simply saves lives.18 This HST should be given as early and as quickly as possible while refraining from giving isotonic fluid when the retained fluid creep is 2-3 L or KG in weight. I also believe it is the right time to write new guidelines and recommendations on the use of fluid therapy for shock resuscitation.4
None.
None declared.
Funds received: None declared.
Is not applicable. I consent to participate in and consent to publish this article.
The datasets used can be accessed from the given references of published articles.
None.

©2023 Ghanem. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.