Journal of
eISSN: 2373-4396


Case Report Volume 11 Issue 3
Director of Cath Lab and Najaf Cardiac Center, Iraq
Correspondence: Khalid Amber, Director of Cath Lab and Najaf Cardiac Center, Iraq
Received: June 11, 2018 | Published: June 11, 2018
Citation: Amber K. Transcatheter management of post infarction ventricular septal repture with concomitant coronary angioplasty. J Cardiol Curr Res. 2018;11(3):157-159. DOI: 10.15406/jccr.2018.11.00390
Ventricular septal defect (VSD) or rupture (VSR) after acute myocardial infarction is an uncommon but catastrophic event with poor prognosis.1–5 Although immediate surgical closure with hemodynamic support (IABP) is the treatment of choice as adviced by the American College of Cardiology and American Heart Association (ACC/AHAr-9). Advanced patient age, hemodynamic instability, surgical challenges and comorbidities still associated with high mortality rates'2'1°'. Medical therapy alone has no role in improving survival and associated with very poor prognosis01'2'. Partial or complete closure of VSR through transcatheter approach appears to be very attractive alternative to surgery and associated with much less mortality and morbidity especially in good centers m.2–15 We introduce a case of large VSR that closed with PIMVSD concomitantly with coronary angioplasty of critically stenosed mid left anterior descending coronary artery it is the first case in Iraq with critical coronary artery disease and large post myocardial infarction VSR which was managed through transcatheter approach and the patient survived after closure.
A 68 years old female patient who is a known case of hypertension and dyslipidemia presented to the emergency department with typical ischemic chest pain and electrocardiographic findings of anteroseptal STEMI. Patient received thrombolytic therapy and consequently had coronary angiography and then refered to our hospital, 15days post infarction for further management. Transthoracic echocardiography revealed moderate left ventricular dysfunction, EF 40%, anteroseptal and apical akinesia, small apical aneurysm, large VSR (17'14mm) with dominant left to right shunt and right ventricular systolic pressure of 45mmHg. An informed consent was obtained and the patient prepared for elective cardiac catheterization with intending of transcatheter closure of the VSR. Under local anesthesia and transthoracic echocardiographic guidance , right femoral and internal jugular vascular access was obtained and selective left coronary artery and left ventricle (LAO/Cranial 35/35) angiography was performed (Figure 1).
Angioplasty of the mid LAD was achieved successfully with 14'2mm .....stent. the VSR was crossed from the LV with a 6F cut pigtail and standard terumo wire 0.35 inch where it advanced into the pulmonary artery. A manually modified 6F multipurpose catheter was introduce through the internal jugular vein into the pulmonary artery where the terumo wire had been snared and exteriorized. A 20mm PIMVSD device (AGA medical) was advanced into the left ventricle and under transthoracic echocardiographic and continuous hand-injection through the already cutted pigtail into the left ventricle, the Figure 2 & Figure 3.
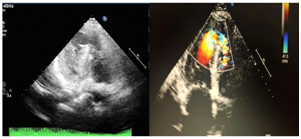
Figure 1 Transthoracic echocardiographic four chambers view shows the apical ventricular septa! defect with left to right shunt.
Although surgical management of the VSR with concurrent coronary artery bypass grafting is the treatment of choice for post infarction VSR, still significant percentage of patients had high mortality rate and specially those with hemodynamic instability, revealed moderate left ventricular dysfunction, EF 40%, anteroseptal and apical akinesia, small apical aneurysm, large VSR (17" 14mm) with dominant left to right shunt and right ventricular systolic pressure of 45mmHg. An informed consent was obtained and the patient prepared for elective cardiac catheterization with intending of transcatheter closure of the VSR. Under local anesthesia and transthoracic echocardiographic guidance , right femoral and internal jugular vascular access was obtained and selective left coronary artery and left ventricle (LAO/Cranial 35/35) angiography was performed.
Angioplasty of the mid LAD was achieved successfully with 14" 2mm .....stent. the VSR was crossed from the LV with a 6F cut pigtail and standard terumo wire 0.35 inch where it advanced into the pulmonary artery. A manually modified 6F multipurpose catheter was introduce through the internal jugular vein into the pulmonary artery where the terumo wire had been snared and exteriorized. A 20mm PIMVSD device (AGA medical) was advanced into the left ventricle and under transthoracic echocardiographic and continuous hand-injection through the already cutted pigtail into the left ventricle, the device deployed completely. At that time, a significant rise in the left ventricle systolic pressure was obsereved. Only after device stability was assessed by left ventricle angiography and transthoracic echocardiography, the device was released. The patient transferred to the intensive care unit and discharged three days later with a well general condition.
Although surgical management of the VSR with concurrent coronary artery bypass grafting is the treatment of choice for post infarction VSR, still significant percentage of patients had high mortality rate and specially those with hemodynamic instability, cardiogenic shock, and/or comorbidities. Generally, closure of the ventricular septa! repture was either performed early after the acute myocardial infarction (less than 14days) which usually carry a high rate of mortality or late (more than 14days) which was associated with successful closure of more than 70%. Transcatheter closure with different types of devices increasingly achieved as good alternative for surgical closure with high rate of closure and much less rate of early mortality. The aim of transcatheter closure may be only a bridge to an urgent surgery or as definitive primary treatment with complete closure. Our case is the first case of post MI VSR in Iraq that was managed by transcatheter approach with concomitant coronary angioplasty and VSR closure at the same session and with successful results. Small hemodynamically non significant residual shunt was detected on transthoracic echocardiography at 24hours follow up. The procedure passed smoothly without significant complications which may be related to the good preparations and the unique team that involved coronary/structural and congenital interventionalists.
Although surgical management of the VSR with concurrent coronary artery bypass grafting is the treatment of choice for post infarction VSR, still significant percentage of patients had high mortality rate and specially those with hemodynamic instability, revealed moderate left ventricular dysfunction, EF 40%, anteroseptal and apical akinesia, small apical aneurysm, large VSR (17" 14mm) with dominant left to right shunt and right ventricular systolic pressure of 45mmHg. An informed consent was obtained and the patient prepared for elective cardiac catheterization with intending of transcatheter closure of the VSR. Under local anesthesia and transthoracic echocardiographic guidance , right femoral and internal jugular vascular access was obtained and selective left coronary artery and left ventricle (LAO/Cranial 35/35) angiography was performed.
Angioplasty of the mid LAD was achieved successfully with 14" 2mm .....stent. the VSR was crossed from the LV with a 6F cut pigtail and standard terumo wire 0.35 inch where it advanced into the pulmonary artery. A manually modified 6F multipurpose catheter was introduce through the internal jugular vein into the pulmonary artery where the terumo wire had been snared and exteriorized. A 20mm PIMVSD device (AGA medical) was advanced into the left ventricle and under transthoracic echocardiographic and continuous hand-injection through the already cutted pigtail into the left ventricle, the device deployed completely. At that time, a significant rise in the left ventricle systolic pressure was obsereved. Only after device stability was assessed by left ventricle angiography and transthoracic echocardiography, the device was released. The patient transferred to the intensive care unit and discharged three days later with a well general condition.
Although surgical management of the VSR with concurrent coronary artery bypass grafting is the treatment of choice for post infarction VSR, still significant percentage of patients had high mortality rate and specially those with hemodynamic instability, cardiogenic shock, and/or comorbidities. Generally, closure of the ventricular septa! repture was either performed early after the acute myocardial infarction (less than 14days) which usually carry a high rate of mortality or late (more than 14days) which was associated with successful closure of more than 70%. Transcatheter closure with different types of devices increasingly achieved as good alternative for surgical closure with high rate of closure and much less rate of early mortality. The aim of transcatheter closure may be only a bridge to an urgent surgery or as definitive primary treatment with complete closure. Our case is the first case of post MI VSR in Iraq that was managed by transcatheter approach with concomitant coronary angioplasty and VSR closure at the same session and with successful results. Small hemodynamically non significant residual shunt was detected on transthoracic echocardiography at 24hours follow up. The procedure passed smoothly without significant complications which may be related to the good preparations and the unique team that involved coronary/structural and congenital interventionalists.
Failure to family functioning index, means, cohesion and conflict in family relations, are among the factors influencing the index of myocardial infarction. The results of this study showed a significant difference between the two groups of patients and healthy in terms of conflict and coherence indices. If the degree of failure is higher, the risk of developing the disease increases. It is important to recognize the impact of these factors on preventing diseases for families, and reducing the gap between ignorance and the underlying condition of the disease. Given that families' access to such factors is not at a single level, facilitating access and providing a suitable platform for teaching and disseminating outcomes through inclusive media, health centers, etc., is essential and can ultimately lead to reducing the incidence of heart attacks for the Iranian population in the future.
The author declares no conflict of interest.

©2018 Amber. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.