Journal of
eISSN: 2373-4396


Research Article Volume 11 Issue 1
1Santa Casa de Miseric
2Di Marchioni Office, Brazil
3Associa
Correspondence: Idiberto José Zotarelli Filho, Associação Brasileira de Nutrologia (ABRAN)/Brazilian Association of Nutrology, Catanduva/SP, Rua Belo Horizonte, 909 - Centro, Catanduva SP Brazil, Tel 55(17) 8166-6537
Received: January 16, 2018 | Published: January 23, 2018
Citation: Junior JB, Buchalla M, Valeriano RC, Novelli D, Fernandes HT, et al. (2018) Statistical Approach to Longitudinal Retrospective Study with Over 1,000 Participants Shows Main Predictors of Cardiovascular Disease for Angioplasty. J Cardiol Curr Res 11(1): 00368. DOI: 10.15406/jccr.2018.11.00368
Introduction: Cardiovascular diseases are the leading causes of death in the population. According to data from the World Health Organization of 2016, of the 20.8 million deaths from these diseases, 9.2 million occur due to atherosclerotic coronary disease.
Objective: aimed to conduct a retrospective longitudinal and observational study on the metabolic, behavioral and clinical profile of patients who underwent angioplasty.
Methods: A total of 1035 participants were submitted to eligibility analysis, followed by the rules STROBE (Strengthening the Reporting of Observational studies in Epidemiology), The present study followed a retrospective longitudinal and observational model on the analysis of the profile profile of patients who underwent angioplasty at Santa Casa de Misericórdia Hospital, São José do Rio Preto, Brazil. The predictors were: clinical, coronary segment affected, laboratory abnormality, types of procedures, previous AMI, previous ATC, previous ATC / Actual ATC.
Results: the result of the statistical correlation of regression between the continuous predictors and the response was demonstrated by means of the Matrix-Plot model graph. All analyzes presented statistical difference with p > 0.05, except between the predictors segment affected x DM, laboratory abnormality x gender, laboratory abnormality x sedentary lifestyle, previous AMI x gender and previous ATC x gender. All the latter presented statistical significance, with p<0.05.
Conclusion: Through the present observational study, we confirmed the literary findings in the questions that involve the direct correlation between the main cardiovascular risk factors such as Diabetes mellitus, sedentary lifestyle, age, SAH, smoking and dyslipidemia in the increase of angioplasty procedures.
Keywords: cardiovascular disease, atherosclerosis, angioplasty, clinical trial
MB, Mitochondrial diseases; mtDNA, mitochondrial DNA; MRI, magnetic resonance imaging; GTCS, generalized tonic-clonic seizure; HSV, herpes simplex virus; ENMG, electroneuromyography
Cardiovascular diseases are the leading causes of death in the population. According to data from the World Health Organization of 2016, of the 20.8 million deaths from these diseases, 9.2 million occur due to atherosclerotic coronary disease (ACD).1 ACD is the most common cause of mortality in developed countries.1,2 Comparing Brazilian patients with stable ACD from 40 to 75 years per 1,000 inhabitants with those from European countries, it is noted that Brazil (58.4 %) is surpassed only by England (59.0 %) and Spain (81.5 %).3,4 This disease is the leading cause of death in some South American countries, such as Argentina (12.0 %), Bolivia (11.0 %) and Ecuador (8.0 %). In Brazil, it is responsible for large numbers of deaths and health care expenditures.2
Among ACDs, we highlight coronary diseases (CDs) resulting from occlusion or narrowing of the coronary arteries due to the formation of atherosclerotic plaques. The CDs, responsible for about 7.4 million deaths per year in Brazil.1,2,5 are associated with a set of risk factors, including advanced age, gender, smoking, obesity, hypertension, diabetes, genetic factors, hypercholesterolemia and sedentary lifestyle.2,3,6
Within the therapeutic arsenal for the treatment of acute myocardial infarction with ST segment elevation (AMICST) to the electrocardiogram (ECG), primary percutaneous coronary intervention is the most important reperfusion strategy. However, its accomplishment within the deadlines defined in the evidence of the studies is a great challenge.7 The typical clinical manifestation of chronic ACD is stable angina, characterized by pain or discomfort in the chest, epigastrium, mandible, shoulder, dorsum or upper limbs. It is usually described by the patient as tightness, oppression, constriction or weight, and is typically triggered or aggravated by physical activity or emotional stress and attenuated with rest and use of nitrates.5,7
The pathophysiological manifestation of ACD involves coronary insufficiency, characterized by the imbalance between supply and consumption of oxygen at the myocyte level. Thus, the goal of treatment of stable angina depends on increased myocardial oxygen supply and reduced demand, which are closely related to contractility, left ventricular parietal stress, myocardial mass, and heart rate and post-load variations determined by blood pressure.6
The diagnosis of ACD is based on the association of clinical history and complementary examinations, since the majority of patients with ACD present normal physical examination. Thus, complete anamnesis and evaluation of personal and family history are fundamental.8,9 The exams are used for the investigation of ACD and follow-up of risk factors, being useful in the diagnostic definition and assessment of its severity, including resting electrocardiogram, chest X-ray, simple ergometric test, echocardiography, myocardial scintigraphy, magnetic resonance imaging, coronary angiotomography and coronary angiography.10,11
The treatment of acute myocardial infarction with ST-segment elevation is consolidated in the trinomial thrombolysis chemistry-primary angioplasty-salvage angioplasty. Depending on the place of care and local conduct, these strategies work and lead to huge reductions in deaths and myocardial damage.2,12 It is essential that the health system is organized to establish the best local strategy to obtain this enormous benefit of opening the artery responsible for the occluded infarct in the shortest time. The most used procedure for the treatment of coronary lesions is the angioplasty with stent implantation.5,13
Although there are advantages with this procedure, restenosis continues to be one of the main limiters of therapeutic success. It is known that inflammation, with accumulation of activated mononuclear cells, may contribute to the development of restenosis.5,14 Primary angioplasty is the use of the balloon catheter with or without coronary stent implantation and without prior thrombolytic use, to mechanically restore the anterograde coronary flow. When available, it is the best option to obtain coronary reperfusion, if started up to 90 min after patient admission. If there is contraindication to thrombolysis or in case of cardiogenic shock, primary angioplasty is also the preferred option.6,15
Therefore, the present study aimed to conduct a retrospective longitudinal and observational study on the metabolic, behavioral and clinical profile of patients who underwent angioplasty.
Participants
A total of 1035 participants were submitted to eligibility analysis, followed by the rules STROBE (Strengthening the Reporting of Observational studies in Epidemiology), https://www.strobe-statement.org/index.php?id=strobe-home.
Study design
The present study followed a retrospective longitudinal and observational model on the analysis of the profile of patients who underwent angioplasty at Santa Casa de Misericórdia Hospital, São José do Rio Preto, São Paulo, Brazil. The predictors were: clinical, coronary segment affected, laboratory abnormality, types of procedures, previous AMI, previous ATC, previous ATC / Actual ATC.
Statistical analysis
Statistical analysis of the data was performed and interpreted by the author of the present study. For data analysis a database was built in the Microsoft Excel spreadsheet which was exported to the Minitab 17 statistical program. A common descriptive statistical analysis and Anderson-Darling normality test were performed for all variables and controls, with reference p> 0.10 as "normal". As there were continuous and categorical predictors (gender, age, SAH, dyslipidemia, DM, smoking e sedentary) and the response predictors (clinical conditions, affected segment, laboratory change, procedure types, previous AMI, previous ATC, previous ATC / actual ATC), linear regression and residual Durbin-Watson analysis were applied. For all linear regression tests, alpha level lower than 0.05 was adopted as significant. For Durbin-Watson residue analysis, the reference significance level was 0.05, adopting as acceptable range of independence 1.46 <dw <1.63 (according to the Durbin-Watson standard table, dU <dw <4-dU), with two explanatory variables for sample size of n > 1.000.
According to the Table 1, we found the profile of the demographic gender (-Male: 62.5%, -Female: 37.5%, age (62.7%), SAH (82.5%), dyslipidemia (40.0%), DM (37.5%), smoking (35.0%) and sedentary lifestyle (95.0%).
|
Continuous Predictors |
Values in Percentage (%) |
|
Gender |
-Male: 62.5 |
|
-Female: 37.5 |
|
|
Age |
62.7 |
|
SAH |
82.5 |
|
Dyslipidemia |
40 |
|
DM |
37.5 |
|
Smoking |
35 |
|
Sedentary |
95 |
Table 1 Demographic data of continuous predictors
We also found the profile of the predictors response, such as Clinical Condition with AMI SUPRA ST: 10.0 %, AMI: 5.0 %, stable angina: 2.5 %, unstable angina: 62.5 %, asymptomatic: 12.5 %, Other: 7.5 %; Affected segment with anterior: 22.5 %, lower: 42.5 %, lateral: 35.0 %; Laboratory change no change: 47.5 %, troponin: 15.0%, CPK / CK-MB: 12.5%, Troponin + Enzymes: 17.5 %, not harvested: 7.5 %; Procedure type with elective: 10.0 %, segment-time: 10.0 %, SCA: 70.0 %, Primary: 10.0 %; Previous AMI: 42.5 %; Previous CTA: 47.5 %, and, finally, was found Previous CTA / Actual CTA with restenosis: 25.0 %, progression: 27.5 %, another injury: 42.5 %, unknown evolution: 5.0 %, according Table 2.
|
Response Predictors |
Types and Values in Percentage (%) |
|
Clinical Condition |
1. AMI SUPRA ST: 10.0 |
|
2. AMI: 5.0 |
|
|
3. stable angina: 2.5 |
|
|
4. unstable angina: 62.5 |
|
|
5. asymptomatic: 12.5 |
|
|
6. Other: 7.5 |
|
|
Affected segment |
1. anterior : 22.5 |
|
2. inferior: 42.5 |
|
|
3. lateral: 35.0 |
|
|
0. no change: 47.5 |
|
|
Laboratory change |
1. troponin: 15.0 |
|
2. CPK/CK-MB: 12.5 |
|
|
3. Troponin + Enzymes: 17.5 |
|
|
4. not harvested: 7.5 |
|
|
Procedure type |
1. elective: 10.0 |
|
2. segment-time: 10.0 |
|
|
3. SCA: 70.0 |
|
|
4. Primary: 10.0 |
|
|
Previous AMI |
42.5 |
|
Previous CTA |
47.5 |
|
Previous CTA / Actual CTA |
1. Restenosis: 25.0 |
|
2. progression: 27.5 |
|
|
3. another injury: 42.5 |
|
|
4. unknown evolution: 5.0 |
Table 2 General data of the response predictors
In Figure 1, the result of the statistical correlation of regression between the continuous predictors and the response was demonstrated by means of the Matrix-Plot model graph. All analyzes presented statistical difference with p > 0.05, except between the predictors segment affected x DM, laboratory abnormality x gender, laboratory abnormality x sedentary lifestyle, previous AMI x gender and previous ATC x gender. All the latter presented statistical significance, with p <0.05
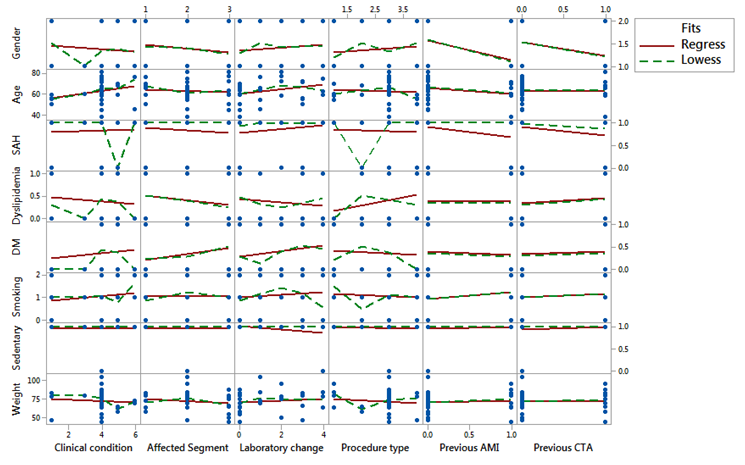
Figure 1 Graph matrix-Plot model showing the results of the regression analysis between continuous predictors and response.
In addition, the results of the regression by Durbin-Watson residual analysis were confirmed in Figure 2, were within the acceptable range of independence 1.46 <dw <1.63 (according to the Durbin-Watson standard table, dU <dw <4-dU) with two explanatory variables and a sample size of n> 1,000. Therefore, there was no relationship of dependence (significance) between the data analyzed, except between the predictors segment affected x DM, laboratory abnormality x gender, laboratory abnormality x sedentary lifestyle, previous AMI x gender and previous ATC x gender. Thus, the results are confirmed by Figure 2, where the residues appear to follow a straight line. There is no evidence of discrepant points or unidentified variables; the residues appear to be randomly scattered around zero. There is no evidence of non-constant variance, absent terms, discrepant points or influential points; the histogram does not follow a normal curve; the residues appear to be randomly scattered around zero. There is no evidence that the error is correlated with each other.
According to the results of the present study and in relation to other literary findings, chest pain suggestive of acute coronary insufficiency remains one of the most frequent complaints in individuals seeking emergency care.1,2,5 Although very common, in general hospitals only a small part of them present acute coronary heart disease or another significant heart problem, leading to a large volume of unnecessary hospitalizations, with a high cost. Even so, the percentage of patients diagnosed with neglected AMISST is not negligible, largely due to the limitations of care protocols and diagnostic tools used.6,7,16
It is not uncommon for patients who present with ACDs without ST elevation to have no electrocardiographic or laboratory abnormalities. In view of this, adequate assessment of the probability of atherosclerotic disease is fundamental.2. The presence of one or more risk factors for coronary atherosclerotic disease, considerably increases the possibility of being the patient with an acute myocardial ischemic disease. Older age, male gender, family history of coronary disease, diabetes, hyperlipidemia, hypertension, smoking, chronic renal failure, previous infarction or atherosclerotic or carotid disease are widely known risk factors.5
The initial diagnosis of ACDs with supra ST is temporally confounded with its treatment. Due to the severity and drama of the disease, diagnosis and treatment go hand in hand, with no loss of time.8-12 The central symptom of sudden cardiac arrest (SCA) with supra ST is chest pain that lasts for more than 20 minutes, which does not subside with rest, nor with the use of nitrates.13-15,17 As in cases of ACDs without supra ST, the pain is usually in oppression, it can radiate to one or both arms, jaw or nape. Also in these cases there are those who present atypical symptoms, usually elderly, women or diabetics. For this reason, these patients, who may reach 30.0% of those who seek the emergency service, receive less frequently adequate therapy according to some analyzes.4
In recent years, technical advances in computed tomography with multiple detectors allowed the assessment of coronary artery lumen noninvasively. The accuracy of coronary artery computed tomography (CT) angiography for the diagnosis of coronary stenosis, when compared to conventional angiography, is already well demonstrated, with a high negative predictive value.3,18-21 Several studies have demonstrated that ATCCor is an important tool in the evaluation of patients with acute chest pain, especially in low and intermediate risk individuals, and is a safe method for the diagnosis of AMISSST and reducing the rate and duration of hospital admission and, if necessary, , the overall cost.22-24
The use of ATCCor in the evaluation of acute chest pain was initially investigated in different unicentric studies, demonstrating high sensitivity for detection of coronary stenosis, high negative predictive value to avoid acute coronary syndromes and moderate positive predictive value. Three large multicenter, controlled and randomized studies evaluated the use of ATCCor in chest pain treated in emergency units. A multicenter trial of 699 patients with low-risk chest pain for stratification strategies using coronary angiotomography (angio-CT) or myocardial computed tomography (CT) scintigraphy rest and stress.2
The CT angiographic strategy reduced the time to diagnosis by 54.0% and the hospitalization costs by 38.0 %, without any difference in the rate of adverse events in relation to the scintigraphy strategy.2. The purpose of the ACRIN-PA study was to evaluate the safety of CT angiography in the evaluation of patients with low and intermediate risk chest pain compared to the traditional approach. None of the patients with negative CT angiography had the primary endpoint analyzed, composed of cardiac death or infarction within the first 30 days after admission. In addition, patients in the angio-CT group had a higher rate of discharge from the emergency units (49.6% vs. 22.7%) and fewer days of hospitalization (18 hours vs. 24.8 h, p <0.001), without significant differences in the incidence of coronary angiography or revascularization in 30 days.
The Rule out Myocardial Infarction by Cardiac Computed Tomography II study (ROMICAT II) evaluated, in similar groups of patients, length of stay in the emergency and hospital costs. The study included 1,000 patients with a mean age of 54 years (46% female). The time of hospital stay was significantly lower in patients stratified for ATCCor when compared to the traditional group (23.2 ± 37 hours vs. 30.8 ± 28 hours, p = 0.0002). The time to exclusion of the SIMI diagnosis was also lower in the group submitted to ATCCor (17.2 ± 24.6 hours vs. 27.2 ± 19.5 hours, p <0.0001). Regarding safety goals, there was no significant difference between the groups.25,260
In the group stratified by ATCCor, there was a significant increase in patients who were discharged directly from the emergency room (46.7 % vs. 12.4 %, p = 0.001), but the use of diagnostic tests was significantly higher in the group submitted to ATCCor (97 % vs. 82 %, P <0.001). Despite the higher cost associated with performing ATCC or and a trend towards more catheterizations and revascularizations, overall costs were similar between the two groups (p = 0.65).26. In summary, the use of coronary artery CT angiography is a safe strategy in the evaluation of patients with low and intermediate risk acute chest pain, reducing incidence, length of hospital stay, and probably costs. Its impact on the number of invasive procedures and revascularization rates are still conflicting.27,28 Its application in patients with low / intermediate risk acute chest pain is recommended as an alternative to the ischemia test in several international guidelines.
In addition, the term SCA is used in situations in which the patient presents clinical and/or laboratory evidence of acute myocardial ischemia, caused by an imbalance between supply and demand of oxygen to the myocardium, and the main cause is the instability of an atherosclerotic plaque. SCA presents in two clinical forms: ST-segment elevation (SCACSST), or acute myocardial infarction with ST-segment elevation (STEMI), and ST-segment elevation non-ST-segment elevation (SCASSST).5,6
Patients with IAMCSST should be treated immediately with primary PCI (within 90 mins of admission). Patients with a formal contraindication to thrombolytic therapy should be transferred for primary PCI within 12 h of symptom onset. The best option for reperfusion therapy in IAMCST is primary PCI. But the delay in achieving PCI reduces this advantage over thrombolytic therapy.29 When this delay is greater than 60 minutes, the advantages equal. Thus, a strategy of prehospital chemical thrombolysis followed by planned PCI (for hemodynamically stable patients) or salvage PCI has shown results equivalent to or better than primary PCI for those patients presenting to the emergency department early.
Especially in those patients where primary PCI cannot be performed within 120 minutes of the first medical contact, or if chemical thrombolysis can be performed 60 minutes prior to PCI. Chemical thrombolysis still seems to play an important role in the treatment of patients with AMICST, especially in those who can not reach a facility capable of delivering effective primary angioplasty rapidly. However, a treatment strategy based on invasive drug therapy depends on the adequate training of a team ready to administer prehospital thrombolytics and the efficiency of the care network, as determined and suggested in the US and Brazilian guidelines. About the subject.
Over the past two decades, several studies have compared invasive strategy to conservative (or selective invasive) strategy.8-13 In meta-analysis by Mehta et al..27 (7 studies, 9212 patients), the implementation of an invasive strategy resulted in an 18% reduction in the relative risk of non-fatal infarction and death (14.4% vs 12.2%, OR, 0.82, 95% CI 0.72-0.93, p = 0.001). In a meta-analysis with 7 studies and 8375 patients, Bavry et al.28 revealed that the invasive strategy was associated with a 25.0% reduction in death (4.9% vs 6.5%, RR = 0, 95% CI 0.63-0.90, p = 0.001), 17.0% in non-fatal infarction rates (7.6% vs 9.1%, RR 0.83 CI 95% 0.72-0 , 96) and 31% in rehospitalization due to unstable angina (RR 0.69 95% CI 0.65-0.74).
In a more recent meta-analysis from O'Donoughe et al.28, 8 studies, n = 10150), it was demonstrated that the invasive strategy resulted in lower death rates, non-fatal infarction and rehospitalization due to angina after one year (21.1 vs 25.9%, OR 0.78, 95% CI 0.61-0.98), such benefits being restricted to patients with increased markers of myocardial necrosis.17. With a longer-term segment, Fox et al.29 (3 studies, 5467 patients) also revealed that patients submitted to the invasive strategy had a lower occurrence of death or infarction after 5 years (14.7 % vs 17.9 %, RR = 0.81, 95 % CI 0.71-0.93, p = 0.002). The absolute risk reduction was more pronounced according to the severity of each patient (2.0 % in low risk patients, 3.8 % in those at risk intermediate and 11.1 % in high-risk individuals). Thus, the sum of the available evidence (from randomized studies and 4 meta-analyzes) supports the option of invasive strategy, since this approach is associated with a significant reduction in death rates, infarction, and recurrent ischemia, when compared to the conservative strategy.
Through the present observational study, we confirmed the literary findings in the questions that involve the direct correlation between the main cardiovascular risk factors such as Diabetes mellitus, sedentary lifestyle, age, SAH, smoking and dyslipidemia in the increase of angioplasty procedures.
The work was supported by Santa Casa de Misericórdia Hospital - São José do Rio Preto - SP, Brazil.
There were no financial interest or conflict of interest.
The authors declare no conflict of interest.

©2018 Junior, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.