Journal of
eISSN: 2373-4396


Case Report Volume 10 Issue 2
1Department of Intensive care, Sanliurfa Education and Research Hospital, Turkey
2Department of Cardiology, Sanliurfa Education and Research Hospital, Turkey
3Department of Anatomy, Faculty of Medicine, Akdeniz Universty, Turkey
4Department of Cardiology, Faculty of Medicine, Akdeniz Universty, Turkey
Correspondence: Yasemin Behram Kandem?r, Department of Anatomy, Akdeniz University Faculty of Medicine, 07070 Antalya, Turkey, Tel 90 242 2496942, Fax 90 242 2274485
Received: November 08, 2017 | Published: November 10, 2017
Citation: Yesiler FI, Tosun V, Kandemir YB, Guntekin U (2017) Is Cardiomyopathy Associated with Peripartum or Anaphylactic Reaction? Which One?. J Cardiol Curr Res 10(1): 00355. DOI: 10.15406/jccr.2017.10.00355
Peripartum cardiomyopathy (PPCM) is a form of dilated cardiomyopathy of unclear etiology. Cardiac failure develops in the last month of pregnancy or within five months after delivery. Symptoms of PPCM are not specific and transthoracic echocardiography (TTE) is the most important tool in diagnosis. Anaphylactic reaction treated with epinephrine due to blood transfusion may consider as a reason for cardiomyopathy. Here we reported a 21-year-old cardiomyopathy patient presented with pulmonary edema resolved with diuretic treatment. Anaphylaxis reaction was observed in the patient after blood transfusion and the patient was treated with epinephrine.
Keywords: peripartum cardiomyopathy, intensive care unit, cardiogenic pulmonary edema
Peripartum cardiomyopathy (PPCM) is a form of dilated cardiomyopathy of unclear etiology, defined as heart failure secondary to left ventricular systolic dysfunction.1,2 The exact pathogenetic mechanism is not fully understood. Several pathogenetic factors are inflammatory, infectious, genetic, autoimmune, oxidative stress.2 Risk factors include multiparity, black race, older maternal age, preeclampsia, and gestational hypertension. Transthoracic echocardiography (TTE) is the most important tool for diagnostic confirmation or exclusion of PPCM and should be performed in every suspected case.2 The approach for treating PPCM mirrors that of treating congestive heart failure.
Anaphylaxis is a severe systemic response by allergen mediated type 1 reaction(decreased systemic vascular resistance, hypotension, increased pulmonary vascular resistance, decreased left ventricular preload) initiated by exposure to a specific antigen in a sensitized organism.3 Rare cases have been reported in the literature about cardiomyopathy in the setting of anaphylaxis treated with epinephrine.4,5 Here, we reported a PPCM patient presented with pulmonary edema with anaphylaxis and epinephrine administration after blood transfusion.
The 21-year-old woman was admitted to the department of obstetrics and gynecology at the gestational age of 37 weeks with bleeding. There was no feature in her medical history. She was a housewife, gravida 1, parity 0. Her pregnancy was terminated by cesarean section due to placenta ablation and intrauterine ex-fetus. Erythrocyte suspension was transfused for intraoperative bleeding and low postoperative hemoglobin value. An anaphylactic reaction developed in the patient during blood transfusion (after about 100 ml). Deep hypotension, bilateral diffuse bronchospasm and anasarca edema were observed to the patient. Adrenaline (1:10000) was administered intravenously to the patient andinvasive blood pressure monitoring was performed. She was taken to the intensive care unit. The Glaskow coma score (GCS) was 14, physical examination was normal and she had not hypotension and tachycardia. Laboratory findings were hemoglobin: 7,4 g/dl, hematocrit: 23%, platelet: 75000, creatinine: 1,19 mg/dl, lactate dehydrogenase (LDH): 508 U/L, calcium: 6,6 mg/dl. The Following hemoglobin was 5,5 g/dl thus 3 units of washed erythrocyte suspension were transfused to the patient. The patient complained of dyspnea, orthopnea, and lower limb edema after 3 hours from the blood transfusion. Oxygen saturation was 84% in room air. On auscultation, bilateral inspiratory rales were heard at all zones of the lungs and she had bilateral marked pretibial edema. Four liters/minute of nasal oxygen, diuretic (furosemide intravenous) and anticoagulant (enoxaparin 6000 unit 2x1 subcutaneously) were given with predicted pulmonary edema and pulmonary thromboembolism. D-dimer (2.56 μg/ml), troponin-T (123 pg/ml) and LDH (505 U/L) were high. Her arterial blood gas analysis showed pH: 7,52; pO2: 69,6 mmHg; pCO2: 36,2 mmHg; HCO3: 29,2 mmol/L; SO2: 86%. Bilateral infiltrations especially at the middle and lower zones and cardiomegaly were notable on the chest x-ray (Figure 1). The bedside transthoracic echocardiography showed normal right ventricles, pulmonary artery pressure of 30 mmHg, left ventricular EF of 40% by Teicholz and Simpson’s methods (Figure 2). The case was diagnosed with PPCM and she was given treatment consisting of an angiotensin-converting enzyme inhibitor and furosemide. Regression was observed on control chest X-ray (Figure 3). Control levels of D-dimer (2,21 μg/ml), troponin-T (81 pg/ml) and LDH (450 U/L) decreased. When the clinical state findings improved, she was transferred to Department of Obstetrics and Gynecology. The patient was discharged after 5 days.
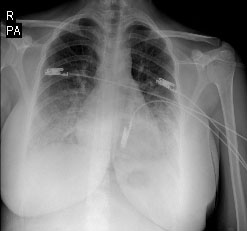
Figure 2 The M-Mode transthoracic echocardiography. A M-Mode transthoracic echocardiography shows a calculated left ventricular EF of 40%.
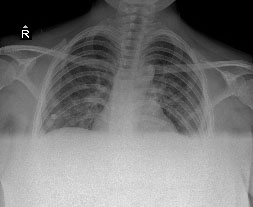
Figure 3 The control chest x-ray. A control chest x-ray shows bilateral regression of infiltrations.
PPCM is a rare form of heart failure with unknown etiology, which affects previously healthy women in late pregnancy or early puerperium. The diagnosis is defined on the basis of four criteria; 1) Development of cardiac failure in the last month of pregnancy or within five months of delivery, 2) Absence of an identifiable cause for the cardiac failure, 3) Absence of recognisable heart disease prior to the last month of pregnancy, 4) LV systolic dysfunction demonstrated by classic echocardiographic criteria such as decreased shortening fraction or ejection fraction (EF).2,6 Symptoms and laboratory findings of PPCM are not specific. TTE is the gold standard in diagnosis. Our patient presented with pulmonary edema that resolved with diuretic therapy. PPCM was diagnosed in our case due to no stories of heart disease, an occurrence of the disease in the early postpartum period, no other reasons to explain heart failure and presence of decreased EF in TTE.
Although the etiology of PPCM remains unclear, a number of potential risk factors have been proposed previously: multiparity, women of African descent, age greater than 30 years, pregnancy with multiple foetuses, a history of preeclampsia, eclampsia or postpartum hypertension, maternal cocaine abuse or selenium defıciency, long-term (>4 weeks) oral tocolytic therapy with adrenergic agonists, inflammation, viral infections, autoimmunity, stress-active cytokines and genetic factors.2,7 In the literature, there are rare case reports about cardiomyopathy following epinephrine administration for anaphylaxis.4,5 In our case, anaphylactic reaction treated with epinephrine due to blood transfusion may considered as a reason for cardiomyopathy. Anaphylactic reaction associated cardiomyopathy was not considered because of the patient had not hypereosinophilia on blood tests.
Patients with PPCM should be managed with established treatment for acute heart failure with oxygen, intravenous diuretics and angiotensin converting enzyme (ACE) inhibitors with intravenous nitrates and inotropes if required. Beta-adrenergic blockers should be added when acute heart failure has been stabilized. Patients with a reduced EF have a higher thrombotic risk.Therefore, low-molecular weight heparin should also be administered. Diuretic, ACE inhibitör, anticoagulant therapy and beta blockers after stabilization were started to our patient.1,2 Some studies showed high mortality rates such as 15% or 32% at 6 months.8 Survivors of PPCM have 30% risk of relapse and a significant decrease of left ventricular function in the subsequent pregnancies with reported 55% mortality and morbidity rates associated with recurrence in subsequent pregnancy.9 So, follow-up, and treatment should be performed in the intensive care unit after diagnosis.
PPCM is a disease with high rates of fetal-maternal morbidity and mortality, whose symptoms are nonspecific, whose diagnosis is based on the exclusion of other possible causes. Therefore, the clinicians should be aware of this disease. Although the etiology is not fully known, it should be evaluated well about risk factors. PPCM can be diagnosed quickly with bedside transthoracic echocardiography, follow-up and treatment in the intensive care unit can improve the prognosis.
None.
Authors declare that there is no conflict of interest.

©2017 Yesiler, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.