Journal of
eISSN: 2373-4396


Case Report Volume 9 Issue 4
1Department of Cardiology, High Specialty Medical Unit Baj
2Head of Health Research Division, Medical Unit of High Specialty No. 1 Hospital of Specialties National Medical Center, Mexico
Correspondence: Martha Alicia Hernández González, Head of Health Research Division, High Specialty Medical Unit No. 1 Hospital of Specialties National Medical Center, IMSS. Leon, Guanajuato, Mexico, Tel (52) 477 7174800
Received: August 04, 2017 | Published: August 16, 2017
Citation: Rey LLL, Xochitl GGM, Ignacio SMV, Horacio GO, Alicia HGM (2017) Idiopathic Aneurysm of the Pulmonary Artery Trunk. Case Report. J Cardiol Curr Res 9(4): 00333. DOI: 10.15406/jccr.2017.09.00333
The pulmonary artery aneurysm (AAP) are uncommon, if they breakthey have highmortalitythat´s whythey identification and stratification is necessary. They can be acquired, congenitaland rarely idiopathic. Its clinic spectrumcomes sinceasymptomaticwith an accidentally discovery in the chest X-ray, dyspnea, hemoptysis, chest pain or sudden death in case of rupture. It reportsthe sixty-two years woman case, with an incidental diagnosticof Pulmonary Artery Aneurysm ofIdiopathic etiologyanditsdiagnostic andtherapeutic approach.
Keywords: pulmonary artery aneurysm, idiopathic, tomographic angiography
Sixty-two years woman, hypertensive, without any other precedent. Asymptomatic, in functional class I of the NYHA. Ingressbyan accidentally discovery in thorax radiography of volume increase in the pulmonary cone. It feel Thrill in the2ºleft intercostal space in parasternal line, mate the percussion of 2cm of diameter, mesotelesystolicmurmurin the pulmonary focus, of soft tonality, intensity III/VI, without irradiations, with 2ºfirm sound; normal peripheral pulses, no cyanosisnordigital clubbing.The rest of the exploration is normal.
Chest x-ray without cardiomegaly, with prominent pulmonary artery cone; Electrocardiogram in sinus rhythm, normal; Transthoracic echocardiogram with aneurysmal dilatation of the pulmonary artery trunk (TAP), maximum diameter of 60m, extending to the emergency of the left branch with a diameter of 37mm, pulmonary artery systolic pressure of 30mmHg, wall thickness of the right ventricle of the right ventricle 10mm without pulmonary valvular pathology; In the Angiotomography the TAP dilatation of 58/67 / 63mm is corroborated, in the proximal,mid and distal segments, extending to the left main branch with a diameter of 35mm. Tests of renal, hepatic and thyroid function were normal; Autoimmune markers (antinuclear antibodies, anti-Sm antibodies and anti-DNA antibodies), antistreptolysin O, rheumatoid factor, VDRL and C-reactive protein, all of them were negative; Serology for Rubella, Toxoplasma, Mononucleosis, Brucella, Chlamydia, Aspergillus fumigatus and Candida were negative; Negative blood culture; Tumor markers Ca 19-9, Ca 125, Carcinoembryonic Antigen and Alpha Fetoprotein were normal. The existence of vasculitis or Marfan syndrome was dismissed, so it was concluded that it is idiopathic. Only medical surveillance is decided.The patient remained asymptomatic and unchanged in the TAP dimensions by echocardiogram at three months of follow-up.
Pulmonary artery aneurysms (AAP) are rare, 1 per 14,000 autopsies, where the prognosis is fatal in the event of rupture.The normal upper limit of the TAP diameter is 28mm and the interlobar artery 17mm; 40mm is considered an aneurysm and its most frequent location is in the TAP with or without involvement of the main branches, or with extension to the left branch.1,2
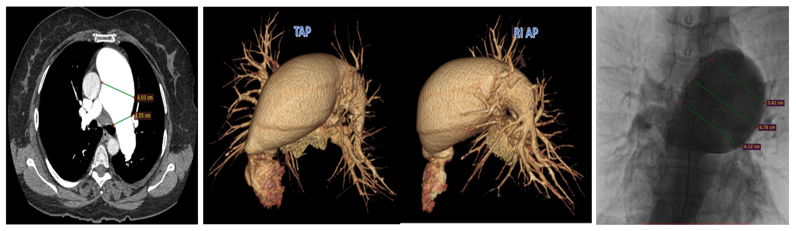
Figure 2 Angiotomographyc 3D reconstruction and angiogram correlation. Pulmonary trunk of 60mm and left artery pulmonary 35mm.
Its etiology is divided into congenital, acquired (connective tissue diseases, infections and trauma) and a small percentage is diagnosed by exclusion as idiopathic. The clinical spectrum may be asymptomatic as a casual finding, or present with dyspnea, hemoptysis and chest pain.3 The complications that may occur are the compression of nearby structures (bronchus or left coronary artery), intraarterial thrombosis, dissection or rupture of AAP where its most evident clinical manifestation is massive hemoptysis or sudden death.1
Surgery is indicated when there is a history of hemoptysis that speaks of dissection or rupture, or when the diameter of the pulmonary artery is greater than 60mm.There are still controversies regarding conservative treatment. It is generally accepted to correct the underlying cause, but in the idiopathic asymptomatic subjectlike this case,only medical surveillance with emphasis in the measurement of the diameter of the pulmonary artery by echocardiography, twice a year, is necessary.4
Idiopathic AAPs are very rare, it is generally accepted that in asymptomatic patients with a diameter of less than 60mm, normal pulmonary pressure, absence of congenital or acquired shuntsproved by echocardiogram are considered low-risk and conservative behavior is chosen, as was our case.
The authors acknowledge to Ramon Humberto Solorio Hernández, his writing assistance, technical editing and language editing.
None.
Author declares there no conflicts of interest.

©2017 Rey, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.