Journal of
eISSN: 2373-4396


Case Report Volume 9 Issue 1
Cardiology, Hospital Universitario Marqu
Correspondence: Gabriela Veiga Fernández, Interventional Cardiology, Hospital Universitario Marqués de Valdecilla, Santander, Cantabria. Avda.Valdecilla 25, CP. 39008, Santander, Cantabria, Spain, Tel 942 20 27 44, Fax 942 33 74 22
Received: May 11, 2017 | Published: May 18, 2017
Citation: Fernández GV, Sastre VF, Camarero TG (2017) Gerbode Defect. An Uncommon Complication of Infective Endocarditis. J Cardiol Curr Res 9(1): 00307. DOI: 10.15406/jccr.2017.09.00307
Left ventricular to right atrial (LV-RA) shunt (Gerbode defect) is rare. It is usually congenital, but rarely is acquired, as a complication of endocarditis. Usually the organism involved is Staphylococcus Aureus however other apparently less aggressive microorganism may be involved making diagnosis and early treatment of these patients a great challenge. We present a case of a 79years old man with dyspnea and fever who was diagnosed of bacterial endocarditis due to Streptococcus anginosus complicated with a Gerbode defect secondary to an extension of infection to the subanular region surrounding the interventricular membranous septum. Despite of an early antibiotic and surgical treatment the patient died showing us the severity of this complication.
Keywords: gerbode defect, bacterial endocarditis
The congenital shunt defect between the left ventricle (LV) and the right atrium (RA) was initially described by Gerbode. Although less common, this shunt has also been described after thoracic trauma, aortic or mitral valve replacement, and in infective endocarditis as an extension of infection to the subanular region surrounding the interventricular membranous septum. Usually the organism most involved is Staphylococcus Aureus.1 However other microorganisms may be involved, assuming in all cases a serious and potentially fatal complication.
A 79years old man was admitted to the hospital because of dyspnea and fever. Eleven days before admission, the patient had been diagnosed of a Klebsiella Oxytoca urinary tract infection initiating antibiotic treatment with ciprofloxacin. He had history of hypertension, dyslipidemia and multiple urological interventions with internal urethrotomy and dilatation due to urethral stenosis. Clinical examination at admission was normal without signs of heart failure. Electrocardiogram (ECG) showed complete heart block requiring implantation of a temporary pacemaker. Laboratory analysis showed leukocytosis with left deviation and elevated C-reactive protein suggesting an infectious process. In this context, a transthoracic (TTE) (Figure 1) and a transesophageal echocardiography (TEE) was performed showing a large pediculated vegetation on a bicuspid native aortic valve that extends to the left ventricle (LV) and right atrium (RA) (Figure 2). A high velocity jet was observed across the right atrium simulating pulmonary hypertension. Aortic wall was complicated with an aneurysm. Rest of valves and biventricular function were normal.2
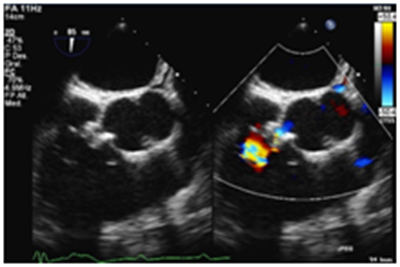
Figure 2 Image with TEE. Color Doppler jet from the left ventricle to the right atrium. despite these the patient finally died.
With the diagnosis of Gerbode defect (LV to RA shunt) due to bacterial endocarditis a coronary angiography was done to rule out the presence of coronary disease before cardiac surgery. The aortography showed contrast across the LV to the RA (Figure 3). Streptococcus anginosus was isolated in blood cultures starting antibiotic treatment with ceftriaxone and daptomycin. The patient underwent surgery with cryopreserved homograft implantation of the aortic root with reimplantation of the coronary arteries. After cardiac surgery the patient developed postcardiotomy cardiogenic shock requiring aortic counterpulsation ballon and advanced mechanical circulatory support with veno-arterial extracorporeal membrane oxygenation (VA ECMO)
Even though the adquired Gerbode defect due to bacterial endocarditis is uncommon there are cases reported in the literature. It´s important to think in it to accurately differentiate it because of it´s challenging diagnosis that can confuse us, for example, with an eccentric jet of tricuspid regurgitation. The causative organism is usually a Staphylococcus aureus and the most patients present with sepsis, shock or heart failure but this not occurred in our case so this should leads us to keep a high index of suspicion in all patients despite their clinical and hemodynamic stability. A correct diagnosis with TEE and color Doppler should be done in all patients with suspicion of infective endocarditis because an early treatment may lead to better clinical results. However the prognosis remains poor even with surgery and advanced circulatory mechanical support.
None.
None.
Author declares there are no conflicts of interest.

©2017 Fernández, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.