Journal of
eISSN: 2373-4396


Case Report Volume 8 Issue 6
1Specialist Senior Registrar, Cardiology Department Rashid Hospital, United Arab of Emirates
2Specialist Registrar, Cardiology Department Rashid Hospital, United Arab of Emirates
3Intern, Medical Department Rashid Hospital, United Arab of Emirates
Correspondence: Akram Jehad Al Rishani, Specialist Senior Registrar, Cardiology Department Rashid Hospital, Dubai, United Arab of Emirates, Tel (+)971528852948
Received: May 05, 2017 | Published: May 9, 2017
Citation: Rajani AR, Al Rishani AJ, Al Zainal J, Al Ali J (2017) Atrial Myxoma: An Emergent Presentation of Acute Bilateral Lower Limb Ischemia and Multi-Organ Showering. J Cardiol Curr Res 8(6): 00302. DOI: 10.15406/jccr.2017.08.00302
A 51-year-old man presented with an acute onset of bilateral lower limb paresthesia. He was diagnosed as acute lower limb ischemia. The Doppler signals were absent in the distal arteries and the CT angiogram confirmed the blockage of left iliac and femoral artery and right popliteal artery. He underwent urgent embolectomy from left femoral and right popliteal artery. The transthoracic echocardiography showed small mass in attached to interatrial septum. The transesophegeal 2D and 3D echocardiography asserted the remnant of cardiac myxoma attached to interatrial septum near the base of anterior mitral leaflet. The removed embolus from the blocked arteries were sent for histopathology and the findings were consistent with myxoma.
Cardiac tumors are very rare and usually detected incidentally. The cardiac myxoma are the most common primary benign tumors found in adults and commonly arises from the left atrium. The clinical presentation may vary from asymptomatic to obstructive symptoms causing syncope, peripheral embolization leading to limb or organ ischemia or stroke, cardiac failure imitating mitral stenosis and constitutional symptoms. Echocardiography plays vital role in the diagnosis of cardiac myxoma. Our patient presented with an unusual presentation of distal embolization of cardiac myxoma causing acute bilateral lower limb ischemia.
A 51-year-old male presented with a history of acute onset of bilateral lower limb paresthesia. There was no other associated symptom. He was known to have diabetes, hypertension, dyslipidemia and bronchial asthma. He did not have any prior ischemic heart disease, arrhythmias, heart failure or any form of coagulopathy. He there was no history of any recent trauma. He stopped smoking two years back.
On clinical examination, he was conscious, oriented. His heart rate was at 81/minute regular, respiratory rate of 20/minute, blood pressure was 152/108 mmHg and was afebrile. Chest auscultation and respiratory examination were unremarkable. On examination of his lower limbs, the left leg was cold, bluish, mottled all the way to the thigh, tender on palpation with absent pulses on Doppler. While his right leg was warm, with no change in color but on Doppler examination, only the popliteal signal was detected, there were no Doppler signal heard in anterior tibial artery.
His ECG was showing normal sinus rhythm (Figure 1). The blood examination included , hemoglobin 12.5 g/dL, hematocrit 39.7%, white blood cells 22.7 x 103/uL, platelets 485 x 103/uL, creatinine phosphokinase 26330 U/L, creatinine kinase MB 271 U/L, troponin 1.38 ng/mL, ,creatinine 2.4 mg/dL, potassium 3.6mmol/L, sodium 136mmol/L, urea 40 mg/dL, bicarbonate 18.4 mmol/L, erythrocyte sedimentation rate 74mm in the first hour, prothombin time 13.6, international normalization ratio (INR) 1.12, absolute partial thrombin time 59.7, osmolality 239mOsm/Kg.H2O, procalcitonin 6.98 ng/mL. Hepatitis and HIV serology were negative and liver function test were normal. Anticardiolipin antibody, antinuclear factor, phosphotidyl serine titers were negative. Protein C. protein S and antithrombin III were within normal range.
The CT angiogram and CT chest aortogram revealed a hypodense filling defect in the aorta below the level of the renal arteries causing partial occlusion of the aorta (Figure 2). There was complete occlusion of the left common iliac artery just after bifurcation of aorta extending up to the common femoral artery (Figure 3). There was good contrast uptake in right common iliac artery, femoral artery, superficial femoral artery up to the popliteal artery then the abrupt cut off of right popliteal artery present with no contrast filling seen in the distal arteries (Figure 4 and 5). Additionally, multiple bilateral wedge shaped infarcts seen in both the kidneys and the spleen (Figures 6). Chest x-ray was normal.
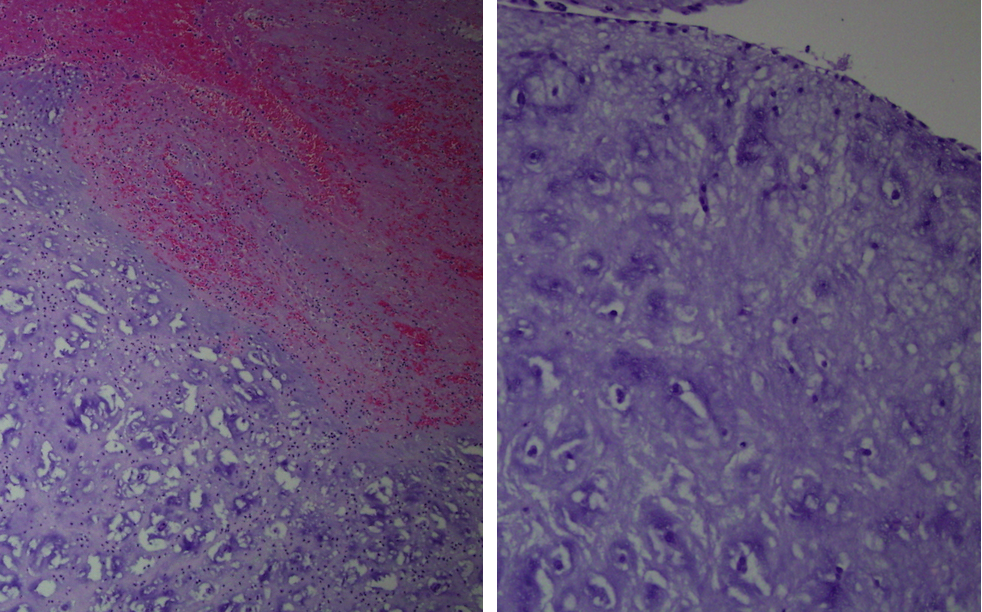
The histopathology of the mass was reported as tumor fragments composed of cords and isolated cuboidal cells and few elongated and stellate cells. Stroma contains myxoid material and hemorrhage. These findings are consistent with myxoma (Figures 7).
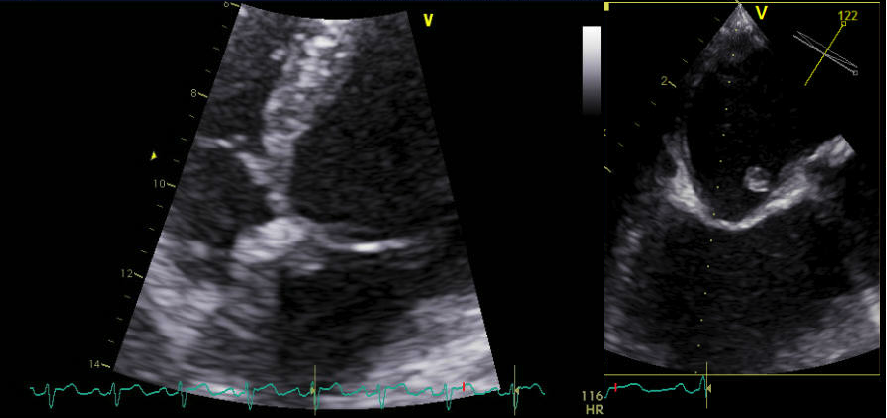
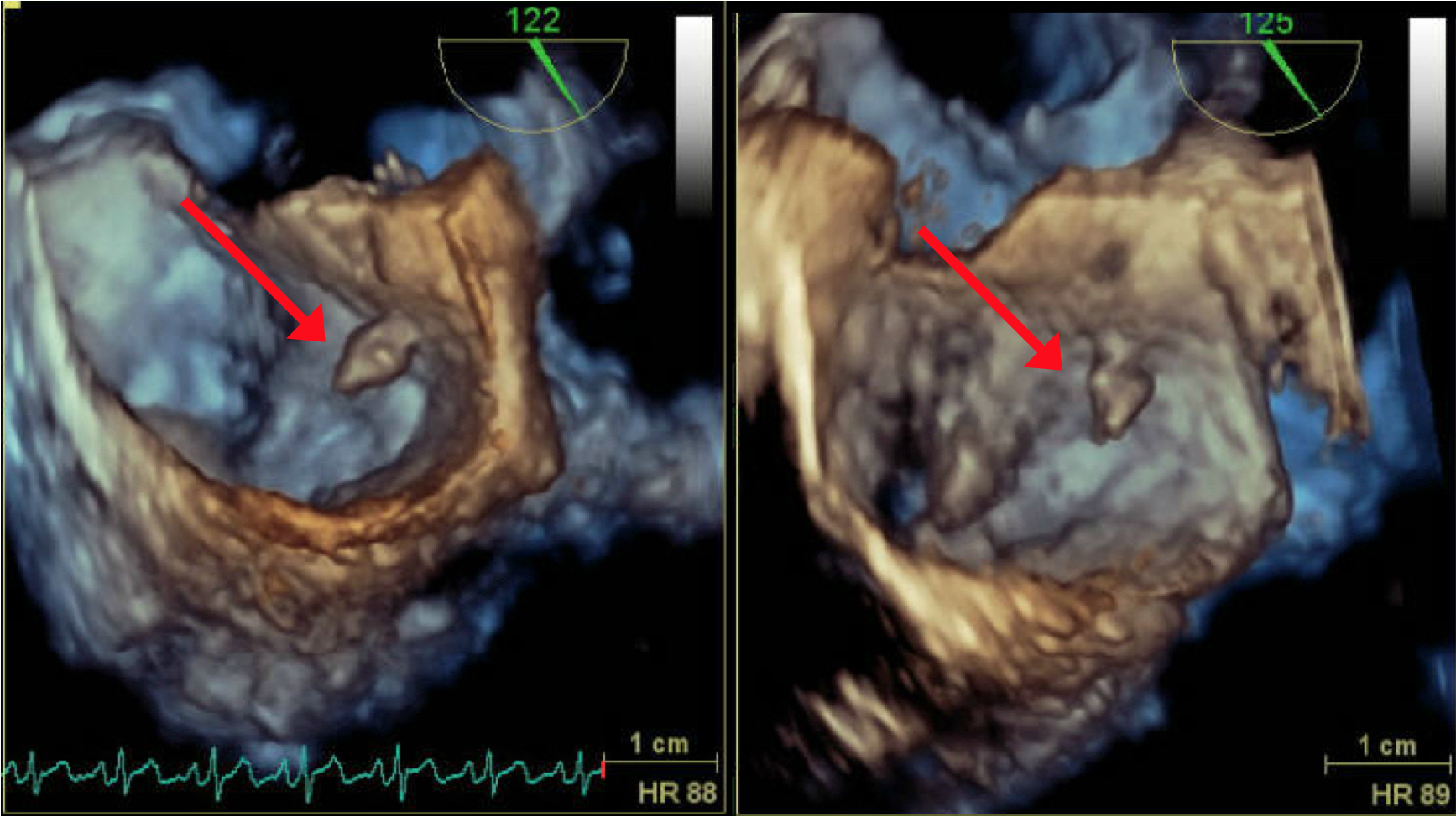
Patient was assessed with Transthoracic echocardiography (TTE) which showed mild left ventricular dysfunction (with ejection fraction of 40%) and a small mass attached to the lower interatrial septum (Figure 8). The findings were confirmed in transesophygeal echocardiography (TEE) study that described a pedunculated mass seen at the lower interatrial septum measured 0.8x0.6x0.5 cm (Figure 9 and 10) close to mitral aortic continuity. This was consistent with left atrial myxoma.
Differential diagnosis
Treatment
The patient underwent urgent embolectomy from left femoral artery and right popliteal artery along with fasciotomy of the left leg. The embolic mass from both the arteries were sent for histopathology. Post-operatively the examination revealed presence of pedal Doppler signals in both lower limbs. Patient was intubated and treated in surgical intensive care unit for six days, when his creatinine phosphokinase shot up to a maximal of 63380 U/L. During the course of his illness he developed acute renal failure, where his creatinine went up from 1.2 mg/dL to a peak of 6.9 mg/dL and that required a short-term renal replacement therapy in the form of hemodialysis. Then the patient recovered and his creatinine went down to 1.4 mg/dL. He was extubated and was treated with injection enoxaparin and then switched to oral anticoagulant tablet warfarin. His TTE/TEE showed remnants of left atrial cardiac myxoma. He was assessed by cardiac surgery team, who advised him to go for surgical excision of the remnant of the myxoma, however he refused the surgery.
Outcome and follow-up
The patient was discharged in a stable condition and mobilizing well with walking frame. He was discharged on tablet warfarin for 6 months, and to keep international normalization (INR) between 2.5 to 3.0. He was advised to do follow up echocardiography study after 6 months, and if results did not change, then yearly.
An atrial myxoma (AM) is a result of proliferation of primitive mesenchymal cells, which would differentiate into endothelial, smooth muscle cells and fibroblasts [1]. Cardiac tumors are very rare with an incidence rate of 0.28% on autopsied adults, 50% of which are diagnosed as atrial myxomas, marking them as the most common benign cardiac tumors [2], affecting middle-aged population (40 – 60 years), with slightly higher prevalence in females [3].
Arising from within the left atrial wall, AMs are often solitary, pedunculated fragile tumors, loosely attached with a fibro-vascular stalk, fixed with a fibrous endocardial base. These tumors can vary in diameter and can go up to 8cm. Due to the frail form of AMs and loose attachment to the base, incidents of embolization of small myxomatous particles, or rarely, the whole body of the myxoma, to the peripheral body parts can occur and causing a wide range of complications, depending on the site of embolization [4].
In earlier literature, reports of cerebral, renal and cardiac complications of AM have been documented, [5,6]. Hofer A et al. [3] has reported a case of bilateral lower limb weakness caused by complete infrarenal occlusion of abdominal aorta due to embolization of cardiac myxoma. That mass was removed by laprotomy [3]. In our case the patient present with lower limb weakness and CT angiography showed partial occlusion of aorta.
The clinical presentation of atrial myxomas varies widely. About 50% of such cases presents with features of mitral valve obstruction. Systemic embolization occurs among one third of patients. 20% of patients will have constitutional symptoms like fever, fatigue, myalgia or weight loss. One fifth of the patients remained asymptomatic [7,8].
The main diagnostic method of choice of AM is the Echocardiography. MRI and CT scans can be used for further evaluation of the mass and its involvement. The treatment of atrial myxoma is surgical resection, where total excision of the mass is performed along with debridement of some of the healthy tissue. Follow up echo is required to monitor for recurrence. Recurrence rate is up to 17%, possibly at the same site of the excised tumor or at other site [9]. Conservative management is advised with regular echocardiography monitoring in selected group of patients including those with high operative risk, asymptomatic patients and in slow growing cardiac myxomas [10].
Nicholls GM and Clearwater G published a similar case of atrial myxoma presented with multiple site of embolization. The patient presented with back pain and confusion, he was diagnosed as acute lower limb arterial ischemia and myocardial infarction. His CT scan mass in his left atrium, there were renal and splenic infarct and embolism in left iliac artery. Urgent embolectomy and fasciotomy was done, but his left leg could not have been rescued. Then he underwent excision of the atrial myxoma [11]. As for our patient, who arrived with a sole presentation of bilateral lower limb ischemia and that also had urgent embolectomy and fasciotomy and beholdenly, both limbs were saved. The patient was offered an option for total excision for the remnant of the myxoma but the patient refused to do surgery. He was advised follow up echocardiography. He was prescribed anticoagulation Warfarin tablets for 6 months. Atrial myxoma is a rare cardiac condition with variable presenting symptoms, thus a high index of suspicion is required for diagnosis. Echocardiography plays a key role in the diagnosis of myxomas. Cardiac surgery is the main stay of treatment of these masses. However, the myxoma has risk of recurrence therefore; follow up echo monitoring is required.

©2017 Rajani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.