Journal of
eISSN: 2373-4396


Research Article Volume 7 Issue 3
1Department of Medicine, Cardiology Service, Cardiovascular Exploration Unit
2Department of Cardiology, Instituto de Investigaciones Cardiovasculares, Universidad de los Andes, Venezuela
Correspondence: Roberto Carlo Correa Bastidas, Avenida Juan de Villegas, Centro Médico de Caracas, Anexo A, Piso 1, Consultorio 176, Caracas, Distrito Capital, ZIP 1011, Venezuela, Tel +58-212-5525262, Fax +58-212-5500076
Received: November 28, 2016 | Published: November 30, 2016
Citation: Correa RC, Condado JA, Abecasis N, Lairet A, Sanabria T (2016) Clinical Follow-up of Octogenarian Patients Undergoing Percutaneous Coronary Revascularization in the Last 5 years, 2010-2015, At Centro Médico de Caracas. J Cardiol Curr Res 7(3): 00248. DOI: 10.15406/jccr.2016.07.00248
Elderly or very old patients are often excluded from randomized studies and therefore are subject to individualized treatment according to their clinical status. Octogenarians constitute a high-risk age group due to the high complexity of coronary disease, more frequently, multi-vessels and associated co-morbidity. In this sense, we to carry out a descriptive clinical follow-up study of patients ≥ 80 years of age treated at our Hemodynamic Unit (Cath Lab), at Centro Médico de Caracas, in the last five years. Since January 2010 to June 2015. Clinical events such as total mortality, cardiovascular and non-cardiovascular mortality, angina, new revascularization, myocardial infarction, and stroke were evaluated. Clinical follow-up was done through an interview with a treating physician, contact the patient or family members directly, clinical history review was made on the database of Cath Lab. Sixty-one patients were followed up, forty-one were male and twenty were female. Total mortality was 23%, cardiovascular mortality was 15% and non-cardiovascular mortality was 8%. In-hospital mortality was 5%, associated with severe cardiovascular complications such as cardiogenic shock and acute pulmonary edema. An average follow-up time was 30.4 ± 16 months. The mean age at baseline, was 83 ± 2.5 and the mean age at the time of completion was 85 ± 2.8. Of the 61 patients 74% remained cardiovascular asymptomatic. There were no major renal complications at the follow-up and there were no significant bleedings.
In conclusion, in a selected sample of octogenarian patients, a total mortality of 23%, with cardiovascular mortality of 15% and non-cardiovascular mortality of 8% was observed. In-hospital mortality was 5% and there were no patients with end-stage renal disease (ESRD) required dialysis during the follow-up period of 30.4 ± 16 months.
Keywords: Elderly; Octogenarian; Stent; Angioplasty; Coronary Artery Disease
DES: Drug-Eluting Stents; BMS: Bare Metal Stent; CAT: Computer Axial Tomography; Cath Lab: Cardiac Catheterization Laboratory; DM: Diabetes Mellitus; CAD: Coronary Artery Disease; LMCAD: Left Main Coronary Artery Disease; ESRD: End-stage Renal Disease
Elderly patients, over 75 years of age, are often excluded from coronary revascularization procedures [1]. Age is a poor prognostic factor that poses patients to be chosen for conservative treatment compared to those patients who are re-vascularized [2,3]. Most randomized studies include patients up to 65-70 years of age [1]. Records provide further information on the clinical course of patients with coronary artery disease since they refer to the real world and usually include more complex patients [3]. Studies which include patients over 75 years of age are very few [2,3] and those who include people over 80 years of age are even scarce. De Carlo et al, show elder women 75 years of age who went in for acute coronary syndrome without ST elevation have similar short-term results to men and better clinical outcome at one-year follow-up. Women undergoing coronary revascularization had a 1/3 lower mortality rate in relation to women without revascularization and without high rates of severe bleeding. Such a lower rate of hemorrhage is attributed to greater use of radial access. According to this study elderly women should not be denied the possibility of revascularization under the pretext of higher rate of in-hospital mortality and more severe bleeding as has been described in previous studies [2].
Randomized studies including octogenarian patients comparing coronary revascularization versus pharmacological treatment and evaluation of Long-term clinical follow-up do not exist in the literature. There are few randomized studies that compare Drug-Eluting Stents (DES) and aortocoronary bypass surgery, showing a higher rate of revascularization in the long term, after 36 months of follow-up for octogenarian patients submitted to Percutaneous revascularization with medicated stent against bypass surgery [4]. Age alone has been considered a risk factor for patients who go in for acute coronary syndrome. However, there is a paradox that elderly patients > 75 years of age are frequently under-represented in clinical trials, whereas in clinical practice and they constitute a significant proportion of the patient population. Although treated to a lesser extent based on available medical evidence, which delays the reference for early diagnostic angiography [5,6]. The evidence supports the concept of greater benefit in reducing cardiovascular events and mortality the earlier an invasive strategy is applied compared to conservative one in elderly patients [5]. Less favorable outcomes in the elderly population may be associated with more complex coronary artery disease, associated co-morbidities, and a higher risk of complications from revascularization procedures. Despite this, recent studies and large international records have shown that the elderly population has substantially improved outcomes with early invasive management [5].
Octogenarian patients’ records and clinical follow-up are even rarer in the literature, and life expectancy has increased in recent decades, making it imperative to know the results of the age group with the new techniques of endovascular revascularization, such as percutaneous angioplasty with stent implantation in this age group [7,8]. In this sense, this study intends to evaluate by clinical follow-up elderly patients, over 80 years of age, undergoing percutaneous coronary revascularization, at the Hemodynamics Unit at Centro Médico de Caracas in Caracas, Venezuela in the last 5 years.
Prior evaluation and approval of institutional Committee the protocol and once informed consent was obtained, clinical follow-up of patients ≥ 80 years of age who underwent coronary revascularization due to acute coronary syndrome or stable angina or positive ischemia induction tests attended the Cath Lab at Centro Médico de Caracas since January 2010 to June 2015. This to achieve clinical evolution at least 1 year post-angioplasty and stent implantation.
To establish a diagnosis of myocardial infarction, it was necessary to confirm it by verifying the patient's medical history or through questioning the occurrence of chest pain greater than 30 minutes in duration with electrocardiographic changes expressed in ST-segment depression 0.1 mV or inversion of T wave 0.1 mV Or by elevation of ST or by elevation of biochemical markers: Isoenzyme Creatine Kinase MB fraction greater than the reference laboratory limit, Troponin I greater than the limit established as normal in reference laboratory.
Unstable angina was classified when the patient merited emergency chest pains assessment for at least 12 hours of observation with simultaneous cardiac enzymes and at least one electrocardiogram. New myocardial revascularization if the patient merited a new angiography in order to re-vascularize the treated vessel or other artery not related to the culprit vessel object to clinical follow-up. Stroke was classified if the patient presented any episode of motor or acute language compromise, with or without sequelae that warranted medical evaluation or performing a CAT scan study or confirmatory nuclear magnetic resonance study.
Statistical analysis
Because this study is essentially descriptive, categorical variables are presented and analyzed as frequencies and percentage, and continuous variables are reported as means plus standard deviation.
Clinical follow-ups were carried out by means of an interview with treating physicians or telephone calls, as well as obtaining information from the registry database of the Cath at Centro Médico de Caracas in Caracas, and the personalized medical history of the attending physicians of the patients subject to clinical follow-up. The follow-up time was 30.4 ± 16 months. The total mortality was 23% during this period of study, corresponding to 8% of non-cardiovascular mortality and 15% of cardiovascular mortality. In-hospital cardiovascular mortality was 5%, which was disaggregated in 3 of 61 patients and these patients attended cardiogenic shock and acute pulmonary edema. Out-of-hospital mortality during the follow-up period was due to ischemic stroke (2 cases, equivalent to 3.3%), one of them with cerebral stem stroke, others due to acute pulmonary edema and sudden death. It was not possible to confirm myocardial infarction as a cause of cardiovascular death. Cardiovascular mortality was 15% including both in-hospital and extra-hospital cases at follow-up. New myocardial revascularization occurred in one case, corresponding to 2% of the observed events (Table 1). 74% of the studied patients remained asymptomatic during the clinical follow-up period (Table 1). The mean age at the time of revascularization was 83 ± 2.5 years and the mean age at follow-up was 85 ± 2.8 years (Figure 1). According to the sex distribution, the male group was more frequent in this selected sample of cases, 67% versus 33%, respectively (Figure 2). During follow-up, no significant hemorrhagic events were recorded. None of the patients required renal replacement therapy during the study period. When the cardiovascular risk factors involved in the study subjects were evaluated, hypertension was the most frequent factor with an occurrence rate of 98%, followed by dyslipidemia with 76%, Diabetes Mellitus 37%, smoking 33% And less frequent overweight and obesity with 26 and 11%, respectively (Table 2). As for the severity of Coronary Artery Disease (CAD), 33% had 1-vessel disease, 36% had 2 vessels, and 21% had 3-vessel CAD. Eight of the patients had a 3-vessel CAD plus left main coronary artery disease (LMCAD) and 2% had CAD 1 vessel plus LMCAD 67% of the patients had multi-vessel disease (Table 3).
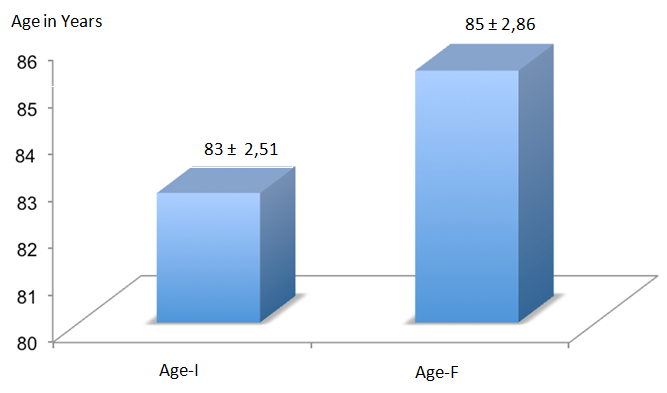
Figure 1: Mean age at the time of the interventional procedure (Age-I) and after clinical follow-up in patients > 80 years undergoing percutaneous angioplasty in the last 5 years (2010-2015) at the Centro Médico de Caracas. n=61.
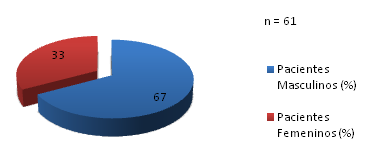
Figure 2: Distribution by gender of patients > 80 years undergoing percutaneous angioplasty in the last 5 years (2010-2015) at the Centro Médico de Caracas.
Cardiovascular Event (CE) |
n = 61 |
% |
Cardiovascular Asymptomatic |
45 |
74 |
CV Death |
9 |
15 |
Non CV Death |
5 |
8 |
Angina |
2 |
3 |
New revascularization |
1 |
2 |
Ischemic Stroke |
2 |
3 |
Table 1: Cardiovascular events in 61 patients > 80 years after percutaneous myocardial revascularization through stent implantation.
CV: Cardiovascular.
Cardiovascular Risk Factors |
n=46 |
% |
High Blood Pressure |
45 |
98 |
Diabetes |
17 |
37 |
Dyslipidemia |
35 |
76 |
Smoking |
15 |
33 |
Overweight |
12 |
26 |
Obesity |
5 |
11 |
Table 2: Cardiovascular risk factors in patients > 80 years of age who underwent angioplasty in the last 5 years at Centro Médico de Caracas (n = 46).
CAD Type |
n=61 |
% |
CAD1V |
20 |
33 |
CAD2V |
22 |
36 |
CAD3V |
13 |
21 |
CAD3V + LMCAD |
5 |
8 |
CADV1V + LMCAD |
1 |
2 |
Table 3: Type of coronary artery disease 1,2,3 vessels and/or left main stem in patients > 80 years of age who underwent percutaneous angioplasty in the last 5 years at Centro Médico de Caracas (n = 61).
CAD: Coronary Artery Disease; 1V: 1 Vessel; 2V: 2 Vessels; 3V: 3 Vessels; LMCAD: Left Main Coronary Artery Disease
In relation to the clinical presentation at the time of intervention, 51% had acute coronary syndrome, 31% had no ST elevation, and 20% with ST elevation, and 49% with stable angina or positive ischemia induction test (Figure 3).
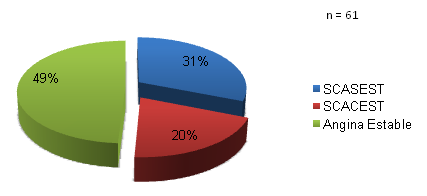
Figure 3: Clinical diagnosis in patients > 80 years old who underwent percutaneous angioplasty in the last 5 years (2010-2015) at the Centro Médico de Caracas.
NSTE-ACS: Non-ST-Segment Elevation Acute Coronary Syndrome; STE-ACS: ST-Segment Elevation Acute Coronary Syndrome.
Regarding drug intake during the follow-up period, emphasis was placed on antiplatelet therapy, anticoagulant therapy, antihypertensives and use of statins (Tables 4-6). Statin consumption remained at 61% and 39% of patients were not taking statins at the time of being contacted for clinical follow-up purposes. Of the 25 patients who used statins, 21 of them (84%) had statins of moderate to low intensity and the remaining 16%, (4 out of 25) patients, had high-intensity statins. More specifically Atorvastatin 80 mg.
Type of Drug |
N |
% |
ARA II |
20 |
49 |
ACEI |
4 |
10 |
Beta-blockers |
15 |
37 |
Calcium antagonists |
11 |
27 |
Spironolactone |
4 |
10 |
Hydrochlorothiazide |
5 |
12 |
Furosemide |
4 |
10 |
Table 4: Type of antihypertensive drug included diuretics received by patients > 80 years of age, undergoing percutaneous angioplasty in the last 5 years (2010-2015) at Centro Médico de Caracas (n = 41).
ARA II: Angiotensin II Receptor Antagonists; ACEI: Angiotensin-Converting Enzyme Inhibitors.
Type of Consumption |
n=41 |
% |
|
Consumption of Statins |
25 |
61 |
|
Moderate and low intensity statins |
21 |
51 |
|
High intensity Statins |
4 |
10 |
|
Non consumption of statins |
16 |
39 |
|
Table 5: Consumption of statins in patients > 80 years of age, who underwent percutaneous angioplasty in the last 5 years at Centro Médico de Caracas (n = 41).
Drug Type |
n = 41 |
% |
Aspirin + Clopidogrel |
21 |
51 |
Aspirin + Prasugrel |
2 |
5 |
Aspirin |
5 |
12 |
Clopidogrel |
9 |
22 |
Warfarin |
1 |
3 |
New oral anticoagulants (Rivaroxaban, Dabigatran, Edoxaban) |
3 |
7 |
Table 6: Antiplatelet and anticoagulation therapy in patients > 80 years of age, undergoing percutaneous angioplasty in the last 5 years (2010-2015) at Centro Médico de Caracas (n = 41).
In relation to the use of antiplatelet therapy and anticoagulant therapy, 21 patients (51%) out of 41 who were able to specify the medications they were habitually receiving continued to receive dual antiplatelet therapy with Aspirin and Clopidogrel during the average follow-up of 30.4 ± 16 months; 12% received Aspirin alone and 22% only Clopidogrel. Only 5% of patients were receiving dual therapy with Aspirin and Prasugrel and 7% were consuming new oral anticoagulants, either combined with Clopidogrel in 2 cases or as monotherapy in a single case. Triple therapy with Warfarin, Aspirin and Clopidogrel alone was used in one patient of the 41 patients who could comply with current therapy (Table 6).
With reference to antihypertensive drugs, 49% of the patients received an antagonist of angiotensin II and 27% took a calcium antagonist. 37% of the patients studied were beta-blockers and 12% had a thiazide diuretic. Only 10% of patients were taking angiotensin-converting enzyme inhibitors and 10% received a furosemide-type loop diuretic. Spirinolactone was received by 10% of the patients studied (Table 4).
The interventional procedure on the cases treated was successful in 95% and the angioplasty failed in 5% of the cases. 95% of patients who successfully received percutaneous stenting treatment benefited from medicated stents and the remaining 5% from untreated stents (Table 7). The left main coronary disease was of 10% (Table 3).
Stent Type |
n=61 |
% |
DES |
53 |
87 |
BMS |
4 |
7 |
Non-Angioplasty performed by FFR> 0.8 |
1 |
1 |
Failed Angioplasty |
3 |
5 |
Table 7: Implanted stents types in patients > 80 years old who underwent angioplasty in the last 5 years (2010-2015) at the Centro Médico de Caracas (n = 61).
Procedure Success 95%
FFR: Fractional Flow Reserve; DES: Drug Eluting Stent; BMS: Bare Metal Stent.
Out of the 14 deceased patients, a total of (23%) during the follow-up period of 30.4 months ± 16 months. Four of the patients were female and 10 were male which represents 29% and 71% respectively in relation to the group of deceased (Figure 4). In relation to the total sample of deceased patients, 7% were female and 17% were male. Thus, we observed a trend of higher mortality in favor of males.
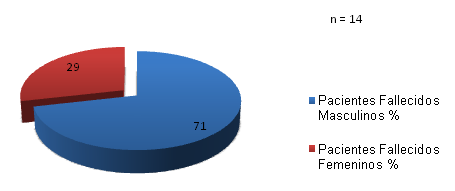
Figure 4: Distribution of total mortality by sex in patients > 80 years undergoing percutaneous angioplasty in the last 5 years (2010-2015) at Centro Médico de Caracas.
Information from 4 patients with onset or presence of atrial fibrillation who required the use of 3 new anticoagulants was obtained; one of them was receiving warfarin. A single patient received triple therapy including aspirin, clopidogrel, and warfarin. Patients receiving new oral anticoagulants included one with Edoxaban 60 mg OD as a single drug, and the other two patients received Rivaroxaban and Dabigatran, respectively (Table 6).
Endovascular treatment through coronary intervention techniques with stent implantation in octogenarian patients is one of the challenges that modern cardiology currently faces [7,8]. The lack of randomized controlled studies that create ways to decide the best behavior to follow requires to make individualized decisions with each patient according to their clinical context. A long-term clinical follow-up was performed in order to determine the total mortality and cardiovascular mortality of this age group and a total mortality of 23%, cardiovascular mortality of 15% and in-hospital mortality of 5% was found. There are no other series studies in our country to compare the mortality observed in our center. The complexity or degree of the severity of coronary disease was expressed in 67% of patients with multi-vessel disease and 69% who received 2 or more Stents (Tables 3, 8). It is of interest to find out that in patients who were successfully treated with stents, 93% of them were medicated and only 7% of the patients received BMS (Table 7). The positive implications for new revascularization were evident when only 1 patient was available for a new myocardial revascularization. In this age group, with a selected sample of cases, the number of patients who were deceased due to cardiovascular causes seem low, (9 patients 15%), and of these 2 were as a consequence of ischemic stroke. The sample is small so it is not possible to perform statistical comparison between groups of patients, however, it was noticed that of the 14 patients who were deceased, 10 of them were males and only 4 were females. In addition, it should be noted that the occurrence of patients in this selected sample of cases, the male sex doubled the female sex (Figure 2). One should be aware of the possibility that the male sex is a factor of a worse prognosis in the group of octogenarians. Of the patients who died in hospital, the severity of the complication was a determining factor in the fatal outcome of the clinical evolution coursing on cardiogenic shock and acute pulmonary edema. The high percentage of multi-vessel coronary artery disease observed in this series study corresponds to some reports in the literature. It should be noted that a non-negligible 10% percentage of the cases studied patients had significant left main trunk disease and were successfully resolved by percutaneous revascularization techniques. It seems that remarkable high usage of medicated stents in these patients, which is 95% of all implanted stents, could guarantee a better clinical evolution with very little requirement for revascularization (Tables 1,7).
Number of Stents |
n=57 |
% |
1 Stent |
32 |
56 |
2 Stents |
18 |
32 |
3 Stents |
4 |
7 |
4 Stents |
3 |
5 |
Table 8: Number of implanted stents in patients > 80 years old who underwent angioplasty in the last 5 years (2010-2015) at the Centro Médico de Caracas (n = 57).
An element to highlight in our study is the use of statins. While it is true that statins in octogenarians is not clearly defined as a formal indication; but treating high risk patients with high intensity statins, Atorvastatin 80 mg or Rosuvastatin 40 mg, is an indication that could carry greater benefits than risks. In our patients only 10% were receiving high-intensity statins. If this behavior could influence a better clinical evolution for octogenarian patients we consider that it should be the object of results obtained from randomized studies at least during 5 years of clinical follow-up. It should be noted that none of the patients undergoing this clinical follow-up merited renal replacement therapy. This can be considered an achievement to be highlighted given the complexity of risk factors, including high blood pressure in 98% of cases and diabetes mellitus in 37%.
In conclusion, in a selected sample of octogenarian patients, a total mortality of 23%, with cardiovascular mortality of 15% and non-cardiovascular mortality of 8% was observed and there were no patients with end-stage renal disease (ESRD) required dialysis during the follow-up period of 30.4 ± 16 months. There was a trend towards higher male mortality during the study period, a finding that must be confirmed in series with a larger sample volume.
Limitations: This is a retrospective study of a selected sample of cases that can only offer us exploratory information in order to design better longitudinal prospective and if possible randomized studies to establish better interventionist concepts and tools in such a select age group. Off 76 patients revascularized with stents 15 were lost in the follow up. They are not included in the analysis of the data.
I would like to thank the following institutions for their sponsorship: Sociedad Venezolana de Cardiología (Venezuelan Cardiology Society), Sociedad Españoala de Cardiología (Spanish Society of Cardiology), Universidad Católica San Antonio de Murcia, España, Menarini Group, Leti Laboratory.

©2016 Correa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.