Journal of
eISSN: 2373-4396


Case Report Volume 6 Issue 5
Cardiac Catheterization Laboratories,
Correspondence: Pablo Avanzas, Cardiac Catheterization Laboratories, Area del Corazón, Hospital Universitario Central de Asturias, Oviedo, Spain
Received: July 23, 2016 | Published: October 4, 2016
Citation: Pascual I, Martinez-Fernandez L, Pun-Chinchay F, Valle R, Moris C, et al. (2016) Angina Equivalent and Revascularization in a Diabetic Patient with a Chronic Total Occlusion of a Single Coronary Artery. J Cardiol Curr Res 6(5): 00222. DOI: 10.15406/jccr.2016.06.00222
A diabetic and hypertensive 75-year-old woman with a previous history of osteoporosis and arthrosis in both knees was referred to the Cardiology outpatient clinic due to the development of exertional dyspnea. The symptoms had progressively worsened in the previous two months. She did not have dyspnea at rest, orthopnea, paroxysmal nocturnal dyspnea, syncopes or chest pain. She was taking enalapril and metformin. Physical exploration was normal, with the exception of central obesity, with a body mass index of 31.2 Kg/m2. The blood analysis revealed a normal hemogram, with glycaemia of 145mg/dL, total cholesterol 200mg/dL, LDL 120mg/dL, HDL 60mg/dL, HbA1C 5,9% and a serum creatinine of 0.95 mg/dL. The electrocardiogram showed sinus rhythm with left bundle branch block (Figure 1).
The initial test performed was an echocardiogram that showed a non dilated left ventricle with mild concentric hypertrophy, preserved LVEF (left ventricle ejection fraction) with normal wall motion, diastolic dysfunction (alteration of the ventricular relaxation). Valvular morphology and function were normal. We then decided to perform a SPECT stress test on a cyclo-ergometer, that showed development of significant hipoperfusion in all inferior wall segments with extension to posterior wall (Figure 2) with partial recovery with rest (Figure 3). During the test, the patient developed progressive dyspnea and vegetative symptoms that disappeared with rest. Following these results, a coronary catheterization was indicated. Left main coronary artery had no significant lesions, circumflex artery had a non severe lesion in the second marginal branch and the right coronary artery was chronically occluded in the proximal segment, with the presence of collateral circulation (Rentrop 3). SYNTAX Score was 12 points.
After beginning medical treatment with atorvastatin, carvedilol and acetylsalicylic acid the patient presented only a slight improvement, so we decide to add clopidogrel and perform a percutaneous revascularization of the total chronic occlusion. Angioplasty was successfully performed (Figures 4-6), with the implantation of two everolimus DES (drug-eluting stents). The patient had a good clinical evolution with total disappearance of the symptomatology.
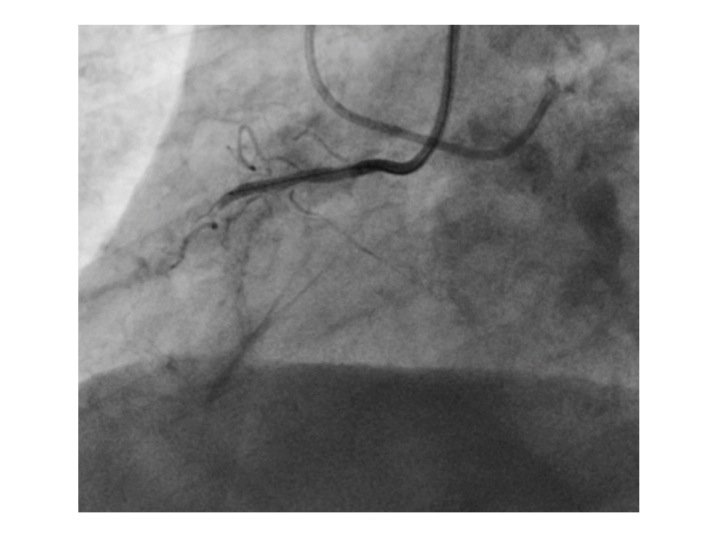
Figure 4 Coronary angiography showing chronic total occlusion of proximal right coronary artery with the coronary wire.
This case presents a 75-year-old diabetic patient with exertional dyspnea as an angina equivalent, with an important ischemic load, preserved LVEF and a chronic total occlusion (CTO) of a single coronary artery with a low SYNTAX score. Conventional medical treatment was initiated and due to the persistence of symptoms, percutaneous revascularization was then indicated.
Diabetic patients are globally at a greater risk of long-term mortality compared to non-diabetic patients. Cardiovascular diseases are the main cause of morbidity and mortality.1‒4 The prevalence of diabetes mellitus is also especially high in patients with ischemic cardiopathy. According to different published studies, this prevalence can reach 40%, considering together a previous well-known diabetes or a new hospital detection. Cardiovascular disease in diabetic patients has some few particular characteristics. Clinical worsening is faster compared to non-diabetic patients. Regarding coronary artery disease severity and extension, it is more frequent the involvement of the left main coronary artery and the presence of multivessel and diffuse disease.1‒4 A key point to consider is that symptoms of myocardial ischemia in diabetic patients can present as angina equivalents without chest pain,4 as happened in the presented case.
Regarding revascularization management in diabetic patients, current guidelines from the European Society of Cardiology1 recommend revascularization in stable patients with multivessel coronary artery disease and/or evidence of ischaemia, in order to reduce cardiac adverse events. With respect of the revascularization method, guidelines endorse coronary artery bypass grafting (CABG) over percutaneous coronary intervention (PCI) in patients with stable multivessel coronary artery disease and an acceptable surgical risk; however, PCI with DES can be considered as a treatment alternative among diabetic patients with multivessel disease and low SYNTAX score (≤ 22).
CTO is defined as complete vessel occlusion with TIMI 0 flow within the occluded segment and an estimated occlusion duration of ≥3months. Among all patients who undergo coronary arteriography, CTO is present in at least one coronary artery in approximately one-third.5 Our patient had an isolated CTO, what represents a challenging patient subset in which to make revascularization decisions. Medical treatment may not be sufficient to relieve symptoms or to improve long-term outcomes, and CABG may be deemed too invasive for single-vessel disease,6 therefore PCI is usually the preferred option in these cases. Current European Society of Cardiology guidelines endorse percutaneous recanalization of CTOs in patients with expected ischaemia reduction in a corresponding myocardial territory and/or for angina relief,1 with a IIa class of recommendation and a B level of evidence. As a final remark, regardless of the strategy chosen, the optimization of the medical therapy and the adoption of suitable lifestyle modifications are essential before proceeding with revascularization.
None.
Author declares there are no conflicts of interest.
None.

©2016 Pascual, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.