Journal of
eISSN: 2373-4396


Research Article Volume 6 Issue 4
1Department of Cardiology, Faculty of medicine, Benha University, Egypt
2Department of Cardiology, Mahalla Cardiac Center, Egypt
Correspondence: Mohamed El-morshedy, Department of Cardiology, Faculty of medicine, Benha University, Egypt, Tel 1062150010
Received: July 18, 2016 | Published: September 14, 2016
Citation: Ammar SM, EL-Keshk ES, Tabl MA, El-morshedy MZ (2016) Relationship between Myocardial Performance Index and Severity of Coronary Artery Disease in patients with Stable Coronary Artery Disease. J Cardiol Curr Res 6(4):00213. DOI: 10.15406/jccr.2016.06.00213
Objectives: To investigate the relationship between severity of coronary artery disease (CAD) assessed with SYNTAX score (SS) and myocardial performance index (MPI) in stable CAD.
Methods: The study included 100 patients who were candidate for coronary angiography. All subjects underwent full history taking, complete clinical examination, echocardiographic examination for calculation of MPI, EF and E/A ratio, and coronary angiography for calculation of syntax score.
Results: Among study population 49 female (49.0%) and 51 male (51.0%) with mean age (48.96±7.30), 80 patients (80.0%) were had angiographically proven obstructive CAD, whereas 20 (20.0%) patients were had normal coronary angiography. There is statistically significant positive correlation between MPI and SS in patients with obstructive CAD (P-value < 0.001).
Conclusion: MPI showed the ability of being a sensitive marker of LV function in SCAD as its value was impaired in proportion to severity of coronary obstruction and it is correlated well with Syntax score as it is the most recent quantitative and qualitative tool that can characterizes angiographically obstructive lesions, risk stratification and prognostication of patients with CAD.
Keywords:stable coronary artery disease, myocardial performance index, syntax score
Coronary artery disease (CAD) is a leading cause of morbidity and mortality worldwide, and its incidence has been gradually increasing. CAD is a progressive inflammatory disease in which atherosclerosis plays a major role in its etiology.1 The SYNTAX score (SS) is a lesion-based angiographic scoring system originally devised to grade the complexity of coronary artery disease (CAD). It is able to aid revascularization decisions and predict mortality and morbidity in patients with CAD.2,3
There are various methods, both invasive and non-invasive, for assessing cardiac function and determining the heart’s performance. Echocardiography remains central in evaluating cardiac structure and function due to its non-invasive nature, high availability and minimal risk profile. The two most commonly used mathematical assessments of left ventricular systolic and diastolic function are ejection fraction and mitral inflow E/A ratio, respectively. Each of these methods has been shown to have considerable limitations.4 In 1995, Chuwa Tei described the myocardial performance index (MPI), defined as the sum of isovolumic contraction and relaxation times divided by the ejection time (ET). MPI has since gained acceptance as a reliable method for the combined evaluation of left ventricular (LV) systolic and diastolic performance, with potential advantages over other indexes in many cardiac diseases.5
MPI is more reflective of overall cardiac function than systolic or diastolic function alone, and applied to independently assess the myocardial performance of left and right ventricles. MPI has since been studied in several other cardiac disorders including heart failure, myocardial infarction (MI), systemic hypertension (HT) and diabetes mellitus (DM) and found to predict both worsened morbidity and mortality.6,7 Although alteration of MPI in patients with MI is well known, there were no satisfactory data about MPI in patients with stable CAD, and the relation between MPI and the severity of coronary atherosclerosis in patients with stable CAD has not been clearly determined yet.8
Study design
This is a prospective, randomized study that involved 100 patients referred to Cardiology Department Benha University Hospital and Mahalla Cardiac Center which were candidates for coronary angiography to determine the severity of coronary artery lesions. Patients with normal coronary arteriogram were also included as a control group. All patients has been previously diagnosed to be Ischaemic either by 12 lead ECG abnormalities, Positive exercise ECG test, RWMA detected by echocardiographic examination or CTA of coronary arteries, also all patients were clinically stable Thorough the study.
Exclusion criteria: Patients were excluded from the study if they were presenting with acute coronary syndrome or with previous myocardial infarction, heart failure, congenital heart disease, significant valvular heart disease, patients with atrial fibrillation (AF), previous percutaneous coronary intervention (PCI), coronary artery bypass graft surgery (CABG), advanced chronic kidney disease, advanced malignancy, myocardial, pericardial disease or recent major surgical operations.
Methods
All patients in this study were subjected to: Full history taking with stress on history of risk factors for coronary artery disease such as: Age, hypertension (HT), Diabetes Mellitus (DM), Dyslipidemia, Smoking or Positive family history for ischemic heart disease.
Complete clinical examination: Including General & local cardiac examination of the heart for cardiomegaly, pulsations, thrills, heart sounds and murmers.
Eleectrocardiography: 12 lead ECG for all patients to detect signs of ischaemia. Also to exclude patients with AF, previous MI or acute coronary syndrome.
Echocardiography: All patients were examined coronary angiography, the following measurements and calculations were obtained by using standard views for M-Mode, two dimensional and Doppler studies according to the guidelines of the American Society of Echocardiographic9: Left ventricular ejection fraction (EF) was calculated using left ventricular (LV) end systolic diameter (ESD) and end diastolic diameter (EDD) by using standard M-Mode technique in parasternal long axis view.
LV diastolic filling patterns were determined by the mitral inflow pulsed wave Doppler examination. In the apical 4-chamber view, the Doppler sample volume was placed in the middle of LV inflow tract 1cm below the plane of mitral annulus between the mitral leaflet tips, where maximal flow velocity in early diastole was recorded.
Peak velocities of early (E) and late (A) filling waves were derived from the mitral inflow velocity curve. The ratio of early to late peak velocities (E/A) were calculated. The LV outflow pattern was recorded from the apical 5-chamber view with the pulsed Doppler positioned just below the aortic valve. Doppler time intervals of MPI were measured from mitral inflow and LV outflow velocity as described by Tei et al.,4 1996 as following:
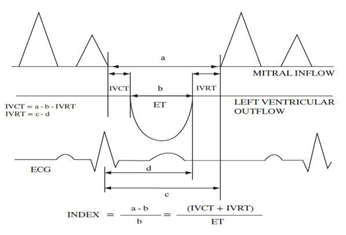
Figure 1 Schematic representation of the measurement of the Tei index, (a) time interval from the end to the start of transmitral flow, (b) left ventricular ejection time (also denoted by ET), (c) time interval from the peak of the R wave on the ECG to the start of transmitral flow, (d) time interval from the peak of the R wave on the ECG to the end of ejection time, (b) left ventricular ejection time.
Statistical analysis
Data management and analysis were performed using SPSS program; version 17. The numerical data were statistically presented in terms of mean and standard deviation. Categorical data were summarized as percentages. Comparisons between numerical variables were done by unpaired Student’s t-test. Comparing categorical variables were done by Chi-square test or Fisher exact test for small sample size. A probability value p < 0.05 was considered statistically significant, a P value < 0.001 was considered highly significant and P value > 0.05 was considered non-significant.
Baseline demographic data
This study included 100 patients in the period from February 2015 to March 2016 of both sex (51 males and 49 females) with mean age (48.96 ± 7.30).divided according:
Group I: 20 healthy with normal coronary angiogram (control group).
Group II: 80 patients with angiographically proven obstructive CAD (patients group).
In control group the mean age was significant lower than in patient group (42.00 ± 3.32 vs 50.72 ± 6.98, P-value < 0.001), there were (10) male and (10) female in control group while (41) male and (39) female in patient group, the difference as regard sex was non-significant (Table 1).
|
|
|
Groups |
|
|
|
|
|
|
|
|
|
|
Total N=100 |
Control N=20 |
Patients N=80 |
Tests |
|
|||
|
|
|
N |
% |
N |
% |
N |
% |
X2/t |
P-value |
|
Sex |
Female |
49 |
49 |
10 |
50 |
39 |
48.8 |
0.01 |
0.92 |
|
Male |
51 |
51 |
10 |
50 |
41 |
51.3 |
|||
|
Age (In years) |
Range |
36-66 |
36.0 - 49.0 |
36.0 - 66.0 |
5.42 |
<0.001* |
|||
|
|
Mean ± SD |
48.96±7.30 |
42.00 ± 3.32 |
50.72 ± 6.98 |
|
|
|||
Table 1 Demographic characteristics of the study population
Characteristics according risk factors
In this table comparison between study populations as regard coronary risk factors shows that there is statistically significant difference between them as regard hypertension and diabetes milletus (P-value < 0.05). Other risk factors showed no significant difference between studied groups (Table 2). According to risk factors the study population were classified into:-
|
|
|
MPI |
|
T-test |
|
|
|
|
|
Mean |
SD |
|
t |
P-value |
|
Family History |
No (n=66) |
49.59 |
7.46 |
1.135 |
0.259 |
|
|
Yes (n=34) |
47.76 |
7.93 |
||||
|
Hypertension |
No (n=59) |
46.15 |
6.55 |
4.92 |
0.001* |
|
|
Yes (n=41) |
53.02 |
7.3 |
||||
|
Diabetes Milletus |
No (n=63) |
47.6 |
8.08 |
2.392 |
0.019* |
|
|
Yes (n=37) |
51.3 |
6.24 |
||||
|
Smoking |
No (n=69) |
49.38 |
7.73 |
0.794 |
0.429 |
|
|
Yes (n=31) |
48.06 |
7.47 |
||||
|
Hyperlipidemia |
No (n=60) |
48.77 |
7.33 |
0.325 |
0.746 |
|
|
|
Yes (n=40) |
49.28 |
8.15 |
|
|
|
Table 2 MPI and coronary risk factors
High risk: patients with ≥3 risk factors (Table 3). In this table comparison between the studied sub-groups shows that there is statistically significant difference between them as regard ET, IVRT, IVCT and MPI (P-value < 0.05). There is gradual increase in MPI with the increase in the status of risk factors of CAD, the more risk factors the more impairment of MPI (Table 4, Figure 2 & 3). According to risk factors the study population were classified into:-
|
|
Low (N=30) |
Moderate (N=58) |
High (N=12) |
ANOVA |
|
|||
|
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
f |
P-value |
|
ET (msec) |
257.23 |
22.41 |
246.19 |
18.93 |
236.5 |
20.13 |
5.317 |
0.006* |
|
IVRT (msec) |
70.2 |
10.69 |
72.4 |
12.62 |
83.08 |
5.52 |
5.629 |
0.005* |
|
IVCT (msec) |
47.17 |
8.67 |
48.71 |
6.96 |
49.17 |
8.48 |
0.484 |
0.618 |
|
MPI |
45.6 |
6.59 |
49.28 |
7.71 |
55.92 |
4.17 |
9.268 |
0.001* |
Table 3 Relation between MPI and coronary risk factors status of studied population
|
|
One (N=20) |
Two (N=25) |
Three (N=35) |
ANOVA |
|
|||
|
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
f |
P-value |
|
ET (msec) |
252.1 |
18.6 |
243.76 |
20.1 |
239.06 |
20.22 |
2.763 |
0.069 |
|
IVRT (msec) |
72.45 |
9.43 |
72.32 |
9.17 |
82.34 |
7.86 |
12.965 |
0.001* |
|
IVCT (msec) |
48.5 |
6.59 |
50.24 |
6.46 |
50.71 |
7.39 |
0.672 |
0.514 |
|
MPI |
47.85 |
4.34 |
50.08 |
3.79 |
55.63 |
3.9 |
28.348 |
0.001* |
Table 4 Distribution of diseased vessels in each group of OCAD
This table shows that the more vessels diseased the more impairment of MPI as reflected by increase in the mean MPI. The difference between subgroups were significant (P-value <<0.001).
|
|
MPI |
|
|
|
r |
P-value |
|
Age |
0.658 |
<0.001* |
|
LVEDd (mm) |
0.135 |
0.233 |
|
LVESd (mm) |
0.452 |
<0.001* |
|
EF (%) |
-0.668 |
<0.001* |
|
ET (msec) |
-0.632 |
<0.001* |
|
IVRT (msec) |
0.658 |
<0.001* |
|
IVCT (msec) |
-0.155 |
0.169 |
|
E (cm/sec) |
-0.017 |
0.881 |
|
A (cm/sec) |
-0.046 |
0.685 |
|
E/A ratio |
0.011 |
0.921 |
|
Mean Syntax score |
0.718 |
<0.001* |
|
Number of vessels |
0.634 |
<0.001* |
Table 5 Correlation coefficient (r) between MPI and variable parameters in patient group
vBivariate relationships of the MPI values in OCAD group showed that MPI was:
Statistically significant positive correlation with:
Age (r = 0.658, P < 0.001).
SYNTAX score (r = 0.718, P < 0.001).
IVRT (r = 0.658, P< 0.001).
LVESd (r = 0.452, p < 0.001).
Vessel number (r = 0.634, p < 0.001)
Statistically significant negative correlation with:
ET (r = - 0.632, P= 0.002).
EF (r = - 0.668, P = 0.280).
|
|
Low (N=30) |
Moderate (N=58) |
High (N=12) |
ANOVA |
|
|||
|
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
f |
P-value |
|
ET (msec) |
257.23 |
22.41 |
246.19 |
18.93 |
236.5 |
20.13 |
5.317 |
0.006* |
|
IVRT (msec) |
70.2 |
10.69 |
72.4 |
12.62 |
83.08 |
5.52 |
5.629 |
0.005* |
|
IVCT (msec) |
47.17 |
8.67 |
48.71 |
6.96 |
49.17 |
8.48 |
0.484 |
0.618 |
|
MPI |
45.6 |
6.59 |
49.28 |
7.71 |
55.92 |
4.17 |
9.268 |
0.001* |
Table 6 Relation between MPI and coronary risk factors status of studied population
|
|
|
Normal (MPI ≤ 40) |
Abnormal (MPI ≥ 41) |
P-value |
|
|
|
(No + %) |
(No + %) |
|
|
Control group (N=20) |
17 (85%) |
3(15%) |
<0.001* |
|
|
Patient group (N=80) |
2 (2.5%) |
78 (97.5%) |
||
|
Number of vessel diseased |
One vessel (N=20) |
2 (10%) |
18 (90%) |
<0.001* |
|
Two vessel (N=25) |
0 |
25(100%) |
||
|
Three vessel (N=35) |
0 |
35 (100%) |
||
|
Syntax score |
Low (N=32) |
2 (6.25%) |
30 (93075%) |
<0.001* |
|
Mid (N=16) |
0 |
16 (100%) |
||
|
|
High (N=32) |
0 |
32 (100%) |
|
Table 7 Distribution of studied population according to prevalence of abnormal MPI
This table shows that most of patients with non-obstructive CAD (control group) had normal MPI values and most of those with obstructive CAD (patient group) had abnormal MPI values, the prevalence of abnormal MPI increased with the increase in number of vessels diseased and and syntax score severity status.
Echocardiographic assessment of LV systolic function plays a pivotal role in the diagnosis, risk stratification and therapeutic guidance of proven medical and interventional therapy in patients with suspected or known cardiac disease.11 EF has been widely used for decades for overall ventricular systolic function and has a central role in many guidelines. EF has a number of important limitations. Some of these such as the calculation of ejection fraction using a variety of geometric assumptions, as well as the error introduced by tangential tomographic planes, generally pose a greater problem to the evaluation of LV volumes than EF.12
The Tei index evaluates the LV systolic and diastolic function in combination and correlates well with invasive measures of systolic and diastolic LV function, and has been reported to correlate better with patient outcome than conventional echocardiographic parameters in various myocardial diseases.13
SYNTAX score is the most recent quantitative and qualitative tool that can characterizes the coronary vasculature with respect to the number, location, complexity, and functional impact of angiographically obstructive lesions in patient with CAD.14
Although alteration of MPI in patients with MI is well known,8 there were no satisfactory data about MPI in patients with stable CAD, and the relation between MPI and the severity of coronary atherosclerosis in patients with stable CAD has not been clearly determined yet.
The study included 100 patients 49 females (49.0%) and 51 males (51.0%) who were candidates for coronary angiography with mean age (48.96±7.30). 80 patients (80.0%) were found to have angiographically proven obstructive CAD (Patient group), whereas 20 patients (20.0%) were found to have normal coronary angiography (Control group).
In this work, there is a higher incidence of abnormal MPI (≥41) in patients compared to control group (85% vs. 15%, P-value <0.001), this mean that most patients with obstructive CAD had abnormal MPI and vice versa, most of those who had normal coronary angiogram had normal MPI.
There are many reports agree with our study confirmed the value of myocardial performance index in assessing patients with possible CAD. Turkan et al, measured the Doppler intervals and MPI in age-matched healthy subjects, and the results were compared with those of patients with previous MI. MPI values obtained were significantly higher in the patients with previous MI, the prolongation of IVCT and the shortening of ET were the alterations in the time intervals that resulted in the increase in MPI values in patients with MI compared to the findings in the healthy age-matched subjects.15
At the level of coronary risk factors, the present study showed that the more number of risk factors of CAD the more impairment of MPI, the mean MPI was 45.60±6.59 in patients with no or one risk factor, 49.28±7.71 in those with 2 risk factors and 55.92±4.17 in those having three or more risk factors, P-value <0.001. In a previous study Mishra and coworkers have shown a limited role for MPI in the assessment of cardiac function in populations with multiple coronary risk factors but free of clinical cardiovascular disease.16
While in various studies investigating CAD risk factors, including those from the Framingham database, have reported that up to 80% of diabetes subjects have hypertension. Hypertension accelerates diastolic and systolic dysfunction in diabetes and increases mortality by more than 7-fold as compared with non-hypertensive diabetics. Data from the Strong Heart Study and others have revealed the independent effect of diabetes on indices of left ventricular systolic function. Compared with non-diabetics, subjects with diabetes had greater left ventricular mass and lower left ventricular fractional shortening.17
Also, in this study, increased MPI values in the patient group may be related to frequencies of risk factors. The relationships between MPI with HT and diabetes were reported in previous studies. However, there was independent relation between MPI value and diabetes. It has been reported that patients with diabetes have a higher MPI values compared with normal subjects.18,19
At the level of angiography, patients with obstructive CAD (patient group) had a significantly higher mean MPI than those with normal coronary angiogram (51.95±5.18 in patient group vs. 37.05±2.25 in control group, P-value <0.001). As regard the number of diseased vessel, the present work demonstrated that the more number of vessel diseased the more increase in the mean MPI denoting more impairment of myocardial function (one vessel 47.85±4.34, two vessel 50.08±3.79, three vessel 55.63±3.90, P-value <0.001).In addition patients with multi-vessel disease and those with high Syntax score had a higher incidence of abnormal MPI compared to those with single vessel CAD or low Syntax score.
In the present work, when patients were classified into those with low, mid and high Syntax score, it is obvious that the mean MPI increase significantly from low to high scores (low 48.41±4.07, mid 51.81±4.39, high 55.56±3.99, P-value <0.001).
Correlation studies in the current study show a significant high positive correlations of MPI with Syntax score (r=0.718, P-value <0.001) and number of diseased vessels (r=0.634, P-value <0.001).
Coronary angiography is an important tool for the quantification of CAD burden in both clinical practice and scientific investigation.20 Researchers have attempted to define angiographic CAD burden using quantitative scoring systems. Historically, this was performed by designation of a single-, double-, triple-vessel and left main disease classification, with luminal stenosis of either ≥50 or ≥70% used to define significance. However, this simple scoring system was limited in its ability to stratify patients with different levels of disease risk, and led to the development of more comprehensive scoring systems for defining atherosclerotic burden and prognosis.21
In the present study, when all the results added to each other, it is evident that these is highly significant association of myocardial performance as reflected by MPI and CAD at many levels: history, clinical and angiographic (number of diseased vessel, Syntax score and presence of obstructive versus non-obstructive CAD).
The association of MPI and stable coronary artery disease has been also proven by Ling et al. who performed dobutamine stress echo testing in 27 individuals. MPI was significantly higher at peak dobutamine stress in the group with ischaemia (13 patients) than in the 14 subjects who had a negative test. More generally, MPI in the ischaemic subgroup showed an increase at peak stress, while in the remaining subjects the index showed no significant change as the test progressed. At the onset of ischaemia IVCT and IVRT were prolonged and the ET shortened, resulting in an increased, pathological MPI. The index appears to be useful in the recognition of myocardial ischaemia and the development of LV dysfunction during a stress echo examination.22
Similar results were reported by Michael et al. who investigated 90 patients with either established CAD or CAD risk factors with routine treadmill exercise stress testing and two-dimensional Doppler echocardiography using the standard Bruce protocol. Both resting and stress MPI values were measured for all 90 of the patients, the prevalence of an abnormal resting MPI was (72/90 or 80%) and the prevalence of an abnormal stress MPI was (48/90 or 53.33%). The average MPI observed in the resting portion of the stress test was (0.636 ± 0.182). The average MPI in the stress portion of the stress test was (0.530 ± 0.250), (P < 0.05). The previous findings reflect that the MPI (Tei) index assessed during exercise may be a sensitive indicator of occult coronary disease in an at risk group independent of wall motion assessment.23
In the present study, we found that MPI is significantly associated with other parameters of LV function as EF (r = - 0.668, P < 0.001), ET (r = -0.632, P= 0.002), IVRT (r = 0.658, P < 0.001), LVESd (r = 0.452, p < 0.001) and age (r = 0.658, P < 0.001).The present study reveals a significant negative correlation between LVEF and Tei index by conventional Doppler imaging and this matched with the results of Lacorte et al.,24 who demonstrated that MPI maintains a strong inverse relation with ejection fraction.24
Myocardial performance index is correlated well with severity of coronary obstruction in stable coronary artery disease. MPI showed the ability of being a sensitive marker of LV function in SCAD as its value was impaired in proportion to severity of coronary obstruction. Our results showed that MPI is significantly correlated with SYNTAX score in assessing severity of angiographically obstructive lesions in patients with SCAD.
Relatively small study sample.
Potential limitations of myocardial performance index as Pseudo-normalization Phenomenon, partial preload dependence and inaccurate measurement in some situations as in AF, tachycardias and conduction disturbances.
The medications including antidiabetic and antihypertensive treatments were continued during the study. These medications could possibly have influenced our results. However, medications were similar between groups in our study.
None.
Author declares there are no conflicts of interest.
None.

©2016 Ammar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.