Journal of
eISSN: 2373-4396


Review Article Volume 3 Issue 2
1Department of Radiology, Azerbaijan
2Department of Cardiac Surgery, Azerbaijan
Correspondence: Eyvaz Abbasov, M Topchubasov Surgical Research Center, Sharifzadeh 196 str., Baku, Azerbaijan, Tel 994503229299
Received: July 12, 2015 | Published: July 31, 2015
Citation: Abbasov E, Manafov S, Abdullayev F. Dual LAD – contemporary review. J Cardiol Curr Res. 2015;3(2):1-6. DOI: 10.15406/jccr.2015.03.00095
Dual LAD had been reported to occur with an incidence of 1% by Morettin1 as well as Spindola-Franco et al.,2 There is a lot of case reports on dual left anterior descending (LAD) coronary artery. The first description of a type IV dual LAD distribution was made in 1939, by Waterston et al.,3 in the case of Sir James Mackenzie, who had this type of distribution. By now six types of this anomaly have been described in the literature. But there is no any review article describing this anomaly in general, so we decided to write one.
Keywords: dual LAD, coronary anomaly
LAD, left anterior descending coronary artery
Dual LAD had been reported to occur with an incidence of 1% by Morettin1 as well as Spindola-Franco et al.,2 There is a lot of case reports on dual left anterior descending (LAD) coronary artery. The first description of a type IV dual LAD distribution was made in 1939, by Waterston et al.,3 in the case of Sir James Mackenzie, who had this type of distribution. By now six types of this anomaly have been described in the literature. But there is no any review article describing this anomaly in general, so we decided to write one.
According to the literature, incidence of the coronary artery anomalies in general population is approximately 1%.4 They are often not associated with clinical signs and symptoms, but some of them can lead to sudden cardiac death. According to the Sudden Death Committee of the American Heart Association, coronary anomalies are responsible for 19% of death in athletes.5 However, these anomalies are usually discovered as incidental findings at the time of coronary angiography or autopsy.
In this anomaly LAD is «divided» into two parts – proximal (short) and distal (long). Each of them comes from different sites and it determines a type of this anomaly. Usually short LAD gives rise to main septal perforator and main (first) diagonal. Dual LAD is usually a benign anomaly. No cases of sudden cardiac death related to it have been described. Spindola-Franco et al.,2 have proposed an angiographic classification for dual LAD in 1983, consisting of four types of LAD anomaly.
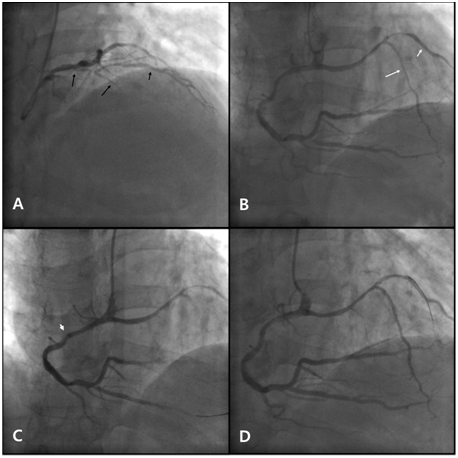
Figure 1 Coronary angiography and percutaneous coronary intervention.
LAD: Left Anterior Descending Artery; LMCA: Left Main Coronary Artery; D1: First Diagonal Artery; RCA: Right Coronary Artery; PDA: Posterior Descending Artery; D2: Second Diagonal Artery; 6 Fr: 6 French; MP: Multipurpose; JR: Judkins Right.
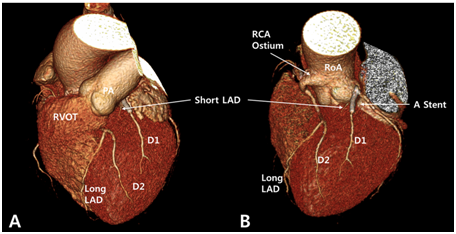
Figure 2 Computed tomographic coronary angiography.
LAO: Left Anterior Oblique; LAD: Left Anterior Descending Artery; LMCA: Left Main Coronary Artery; RCA: Right Coronary Artery; AIVG: Anterior Inter Ventricular Goove; D1: First Diagonal Artery; D2: Second Diagonal Artery; RVOT: Right Ventricular Outflow Tract; PA: Pulmonary Artery; RoA: Root of Aorta.
In the case presented by Maroney J & Klein LW,7 they described another new variant (type VI) of dual LAD. The long LAD arose from the right coronary artery and followed a unique route underneath the right ventricular outflow tract in the interventricular septal area to the interventricular groove. Some authors think that this type may have greater clinical significance than other types because compression of the coronary artery between the right ventricular outflow tract and the aortic root in situations of increased pulmonary blood flow could cause coronary blood flow restriction and sudden cardiac death.8,9
As we may see, there are numerous variants of long LAD course. And it is possible that more types of this anomaly will be described in the future. But all of them have in common LAD territory supplied by two different vessels.
None.
Author declares there are no conflicts of interest.
None.

©2015 Abbasov, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.