
Proceeding Volume 3 Issue 1
V course on adult congenital heart disease
Rosaria Barracano
Regret for the inconvenience: we are taking measures to prevent fraudulent form submissions by extractors and page crawlers. Please type the correct Captcha word to see email ID.

Department of Cardiology, Italy
Correspondence: Rosaria Barracano, Department of Cardiology, Majoring in cardiology at AORN Monaldi, Avellino Area, Italy
Received: March 19, 2015 | Published: June 26, 2015
Citation: Barracano R. V course on adult congenital heart disease. J Cardiol Curr Res. 2015;3(1):9-11. DOI: 10.15406/jccr.2015.02.00088
Download PDF
Proceeding
Absence of symptoms and clinical events until 14.08.2014 when he felt palpitation during strenuous physical activity (running).
ECG recorded at Sessa Aurunca Hospital showed monomorphic ventricular tachycardia
Successful Electrical Cardioversion with 200 J DC Shock
Ecg After Electrical Cardioversion
Asymptomatic
- 63 KG, 171 CM, B.P. 86/50 MMHG.
- Systolic Murmur: 4/6 over the left third and fourth intercostal spaces along the sternal border.
- ECG: HR 57 BPM. PR = 180 MSEC. QRS = 150 MSEC. Complete Right Bundle Branch Block With Secondary Abnormalities Of The Ventricular Repolarization.
Residual mild VSD.
No residual RVOT obstruction.
Echocardiography
- Residual mild VSD.
- No residual right outflow tract obstruction.
- Good biventricular size and function.
- Slight biatrial dilatation.
What guidelines says
ESC Guidelines for the management of grown-up congenital heart disease (new version 2010).
Sudden cardiac death (SCD) in GUCH
- SCD is of particular concern IN GUCH patients.
- Five defects with greatest known risk:
- Repaired Tetralogy of Fallot,
- TGA with atrial switch,
- Congenitally corrected TGA,
- Aortic Stenosis,
- Univentricular syncope is a warning event requiring careful evaluation of arrthythmia.
- Although various risk factors have been defined, algorithms for risk assessement and indications for ICD implantation have so far not been well established.
Atrial/ventricular tachycardia and SCD in TOF
This is related to progressive haemodynamic problems and/or surgical scarring, and thus is seen with increasing frequency with longer follow-up. SCD is reported in 1-6% of cases [in most instances due to VT/ventricular fibrillation (VF)], accounting for approximately a third to a half of late deaths.
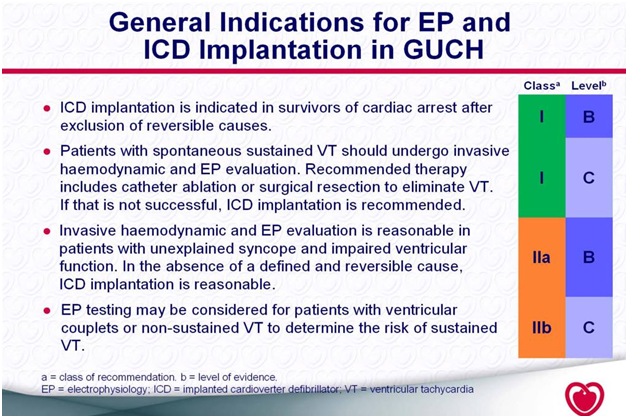
Current guidelines for the prevention of scdgive the following recommendations for patients with CHD: ICD
- Implantation is indicated in survivors of cardiac arrest after exclusion of reversible causes (IB9).
- Patients with spontaneous sustained ventricular tachycardia (VT) should undergo invasive haemodynamic and EP evaluation.
- Recommended therapy includes catheter ablation or surgical resection to eliminate VT. If that is not successful, ICD implantation is recommended (IC9).
- Invasive haemodynamic and EP evaluation is reasonable in patients with unexplained syncope and impaired ventricular function. In the absence of a defined and reversible cause, ICD implantation is reasonable (IIaB9).
- EP testing may be considered for patients with ventricular couplets or non-sustained VT to determine the risk of sustained VT (IIbC9).
- Prophylactic antiarrhythmic therapy is not indicated for asymptomatic patients with isolated premature ventricular beats (IIIC9).

“The complex anatomy and history of multiple previous surgeries in adults with congenital heart disease pose many limitations and technical challenges related to the placement of a pacemaker or AICD.”
Aicd implantation increases thromboembolic risk
202 patients with documented intracardiac shunts
- Baseline risk of systemic thromboemboli in pts with intracardiac shunts was 0.5% to 0.7% per year.
- Transvenous PMK or ICD leads increased this risk >2 fold.
- Importance of an epicardial approach.
Acknowledgment
Conflicts of interest
Author declares there are no conflicts of interest.
Funding

©2015 Barracano. This is an open access article distributed under the terms of the,
which
permits unrestricted use, distribution, and build upon your work non-commercially.


