Journal of
eISSN: 2373-4396


Editorial Volume 2 Issue 2
Department of Clinical & Experimental Cardiology, USA
Correspondence: Francisco R Breijo-Marquez, Department of Clinical & Experimental Cardiology, East Boston Hospital, School of Medicine, 02136 Boston, Massachusetts, USA
Received: March 02, 2015 | Published: March 4, 2015
Citation: Breijo-Marquez FR. An overview on the short qt interval in childhood. J Cardiol Curr Res. 2015;2(2):36-40. DOI: 10.15406/jccr.2015.02.00052
The QT interval on the electrocardiogram involves both the electrical depolarization (QRS complex) as the electrical repolarization of the ventricles (T wave). Any significant change in the length or voltage of the same could have serious consequences. Classically, the short QT interval is defined as an alteration in the ECG in which such interval is shortened to its normal length; therefore, it is a sign and not a symptom. So much so that, there may be patients with such electrical disturbance and without showing any symptoms throughout their lives.
The short QT syndrome (SQTS) is the set of symptoms presented by a patient who has a shortening of the QT interval on the ECG. It is therefore the set of symptoms and signs, in this case the QT interval shortening. (Whenever we speak of "syndrome”, we mean to the set of symptoms (subjective appreciation) and signs (objective appreciation) observed in any disease. This syndrome is a cardiac channelopathy associated with a predisposition to atrial fibrillation and sudden cardiac death.
The diagnostic hallmark of the condition remains a short ECG QT interval; however, consensus on an appropriate cutoff value and diagnostic criteria sufficient to establish a diagnosis of SQTS have yet to emerge in the literature. Therefore, newborns are already carriers of such genetic alterations (channelopathies) though they still not show any symptom. It is curious to seeing how in the overwhelming majority of studies on the topic, fall upon adulthood people and not upon childhood. Especially if we consider that short QT syndrome is considered as a genetic disease and, therefore, of affected newborns by such genetic alteration: The newborns could suffer from the beginning of their lives the consequences of such disease (sudden cardiac death in infants, mainly).
That is true: Despite how much that has been written about the short QT interval in the past 14years, most of them fall on patients older than 15years. (We have not found any clinical work in which the individual studied was a newborn or a person under 15years; effectively very little has been written about this event during childhood. And yet such an event is considered a genetic and heritable event, since it is widely accepted its definition as an inherited disease with a dominant pattern). The short QT syndrome is considered a "rare disease", maybe it is because is being diagnosed little. To date, many aspects of this electrocardiographic event are still very dark and many more medical studies over this topic are needed.
It was a discovery very important when thanks to sagacity of Gussak et al.,1 and Gaita et al.,2 was showed the existence of a shortening in the QT interval on the ECG. This shortening could be the cause of a sudden cardiac death in carrier patients. The authors called this event as a "short QT Syndrome”. Since that time (2000) much has been written about this kind of event, however little is known about which is the best handling and treatment of the same to date.2,3
Currently, there is not any unanimity among different authors on what should be the limits of the length of the QT interval so that it can be considered as short. For the majority of the authors, a length of corrected QT interval that be equal to or less than 0.350seconds should be considered as "short QT interval". Nor is there unanimity among authors about whether a short QT interval on the ECG isolated in patients without symptoms should be follow-up or not. On whether the isolated presence of a short QT interval on the ECG should be considered worthy of being studied and follow-up, there are too many discrepancies between different authors. A long-term follow-up study of healthy Finnish individuals with short (<340ms) and very short (<320ms) QTc values who had no documented arrhythmic events after an average follow-up of 29years. Additional studies examining subjects with short QT intervals from the general population have revealed similarly benign outcomes with no evidence of increased arrhythmic risk. These findings suggest that the presence of a short QT interval in isolation is not always predictive of an increased arrhythmic risk and therefore should not invariably lead to a diagnosis of Short QT Syndrome. However, these circumstances should not ignore clinical follow of all patients with a short QT interval isolated, since at any moment in their lives could have symptoms and, in many cases, debuting with cardiac arrest or sudden death.
In 2000, Gussak et al.,1 described a shortening of the QT interval in three members of a family whom had several episodes of paroxysmal atrial fibrillation. Similar ECG changes were seen in an unrelated patient and he was associated with sudden cardiac death. The authors have denominated to that electrocardiographic phenomenon as "Idiopathic short QT interval".
The QT interval must include the length from the beginning of the Q wave (in its descending branch) until the end of the T wave on the electrocardiogram (Figure 1).

Figure 1 A complete cardiac cycle can be seen; QT-interval has been written in red. It is not possible to see Q wave. It is necessary to note that the Q-wave is not always present in the ECG.Moreover, Q wave can be ≥ 0.08 seconds in its length- on infarcted patients especially. This fact would distort the true measure of the interval in question andaccordingly, QT-interval measure could be overestimated or underestimated. According to correction formulas, (Bazett and Fridericia are the most used) in relation to heart rate, normal values in the length of the QT interval would be between 0.400 and 0.440 seconds. However, for most authors the interval length should be ≤ 0350 seconds before being considered as shortened.
Antzelevitch et al.,3 suggest as a "normal QTc" when the average QTc in healthy individuals is within a range of 0.350-0.450 seconds for males and 0.360 - 0.460 seconds for women; Therefore, QTc ≤ 0.350seconds for men and for women ≤ 0.360 seconds is to be considered as short QT interval. We agree with these considerations, we consider a shortening of the QT interval on the electrocardiogram when the seconds obtained in the measurement of its length reaches these data.
Bjerregaard et al.,4 says the role of a short QT interval in these settings is so far not known. Hypercalcemia (for example) often leads to shortening of the QT interval, but there are no data in humans to suggest an increased risk of sudden cardiac death in this setting. In addition, a shorter-than-usual QT interval has beenreported in patients with Chronic Fatigue Syndrome and in response to atropine, catecholamine and Hyperthermia. When a short QT interval is encountered in daily clinical practice, these various scenarios needs to be considered, but it is still not possible to come up with clear guidelines for how to work up and risk stratify such individuals. Genetic testing is only useful in very few cases.
Gollob and al.,5 have written over 61 cases of Short QT Syndrome. Their cohort of 61 cases was predominantly male (75.4%) and had a mean QTc value of 0.306seconds with values ranging from 0.248 to 0.381seconds in symptomatic cases. For Gollob et al.,5 the overall median age at clinical presentation was 21years(adulthood)[ IQR: 17 to 31.8 years) with a value of 20 years (IQR: 17 to 29years) in males and 30years (IQR: 19 to 44years) in females.]
These authors developed, in reference to the ECG characteristics of the general population, and in consideration of clinical presentation, family history and genetic findings, a highly sensitive diagnostic by means of a scoring system.3
This "scoring system" includes:
|
QTc in milliseconds |
|
|
<370 |
1 |
|
<350 |
2 |
|
<330 |
3 |
|
J point-T peak interval |
|
|
<120 |
1 |
|
Clinical History |
|
|
Sudden cardiac arrest |
2 |
|
Polymorphic VT or VF |
2 |
|
Unexplained syncope |
1 |
|
Atrial fibrillation |
1 |
|
Family History |
|
|
1st or 2nd degree relative with SQTS |
2 |
|
1st or 2nd degree relative with sudden death |
1 |
|
Sudden infant death syndrome |
1 |
|
Genotype |
|
|
Genotype positive |
2 |
|
Mutation of undetermined significance |
1 |
|
Patients are deemed high-probability (≥ to 4 points), intermediate probability (3 points) or low probability (≤ 2 points). |
|
Typically and until now, has been considered a short QT syndrome, as long as the following conditions are met:
Hyperkalemia |
Hypercalcemia |
Hyperthermia |
Acidosis and Effect of catecholamine |
Effects of drugs such as digitalis and some antibiotics (especially macrolides) |
Activation of KACh |
Activation of KATP |
Table 1 Secondary Causes for Short QT interval
We also think is worthy to be mentioned an interesting paradoxical ECG phenomenon called deceleration-dependent shortening of QT interval (shortening of QT interval associated with a decrease in heart rate) should also be considered in a differential diagnosis 5. In the present written, we present a short QT interval on a 7-year-old girl with very vague and imprecise, symptoms without a family history for a "short QT interval”, nor genetic alterations.
QT-Interval, short QT syndrome, dizziness, arrhythmias, syncope, cardiac arrest, sudden cardiac death
A7-year-old girl was studied. She is a Caucasian. She is an only daughter. Her father is 36years old and her mother is 35years old. The medical history of both mother and father has no clinical interest. In the paternal family nor is there antecedents to cardiac problems. The maternal grandmother has had problems with cardiac ischemia at age 55. The maternal grandfather is a non-insulin dependent diabetic. The pregnancy and childbirth were normal. Birth weight was 3,650kg. Birth height was 52cm. The childbirth was performed by cesarean. The Apgar test was 10/10 in the first minute of life. Ponderal growth disorders have not been observed. Her current weight is 42kgs. Her current height is 152cms.Her vital signs include a pulse of 80-90bpm, respiratory rate of 18 breaths/min, Temperature of 98.2° F (36.8° C), and Blood Pressure of 1107/621mm Hg. She is not currently on any medications and has no history of any known allergies.She is not a "medication taker" usually (Throughout her short life, she has not taken many medications since she has not been problematic from a medical viewpoint). The young girl was born with a severe bilateral dacrocystitis, which was resolved by surgery.
For two years, she tells her mother that she wakes up at night with much sweat and nightmares. Her mother went to the cardiologist with her daughter because observed how the girl is always very tired when she was running, with intense fatigue and her face is very red due to a minimum exercise. Sometimes, the girl referred to her mother that when she was running felt dizziness, palpitations and needed to stop and sit downbut she is recovered without further incident by means of rest.
A Battery of Test on the girl was performed:
Cardiac auscultation: The heart sounds are rhythmic with a slight increase in frequency according to her age. The cardiac tones are synchronous with the peripheral pulses (radial and carotid). The lung fields are clear, without pathological sounds added. Thoracic Radiology was considered as normal. There is no evidence of cardiomegaly.
Blood analysis: Comprising the classical cardiac biomarkers and ion profile was normal (within range for her age and sex). The last analytical results were:
|
Sodium: 139 meq / L (136-146 mmol / L) |
|
Potassium: 3.9 meq / L (3.5 to 5.0 mmol / L) |
|
Chloride: 105 (102-109 mmol / L) |
|
Calcium 9.1 mg / dL (2.2 to 2.6 mmol / L) |
|
Magnesium: 1.9 mg / dL (0.62 to 0.95 mmol |
|
Bilirubin: Total 0.5 mg / dL (5.1 to 22 mmol / L), Indirect: 0.4 mg / dl (3.4 to 15.2 mmol / L), Direct 0.1 mg / dL (1.7 to 6.8 mmol / L). |
|
Alkaline phosphatase 46 U / L (0.56 to 1.63 kat/ L) |
|
Glutamic-oxaloacetic transaminase (GOT) 17 U / L (0.20 to 0.65 ĩkat / L) |
|
Gamma glutamyltransferase (GGT) 13 U / L (0.15 to 0.99 ĩkat / L) |
|
Glutamic-pyruvic transaminase (GPT) 18 U / L (0.12 to 0.70 ĩkat / L) |
|
Albumin 3.6 g / dL. |
|
Globulin (total): 2.7 g / dl |
|
Alpha1 globulin 0.2 g / dL |
|
Alfa2 globulin 0.6 g / dL |
|
Beta globulin 0.6 g / dL |
|
Gamma globulin 0.9 g / dL |
|
Troponin I: 0 ng / ml |
|
Troponin T: 0 ng / mL |
|
(CK-MB) mass: 0.1 ng / ml |
|
Creatine kinase (CK) (Total): 56 U / L |
|
LDH 123 U / L |
The Main Test was the electrocardiographic study with 12 leads (Figure 2).
The ECG was taken from her hospital. It was considered as a normal ECG tracing by cardiologists. No other test was prescribed to consolidate such diagnosis.
In an overview of ECG, it gives the impression of normality:

Figure 3 Detail on VF.
QT interval = 0.303 seconds
RR interval = 0.750 seconds (HR. to 80 bpm, approx.)
According Bazett formula, would result a value of 0.349 seconds: a short QT interval for women.
According Fridericia formula would result a value of 0.333 seconds.
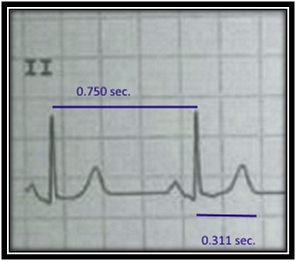
Figure 4 Detail on D2 lead.
QT interval = 0.311 seconds.
RR interval= 0.750 seconds. (HR. to 80 bpm, approx.)
QTc Bazett: 0.359 seconds. (Lesser than 0.360 for women)
QTc Fridericia: 0.342 seconds.
If we value data from QT and RR interval on the V6 (Figure 5), these are the results.
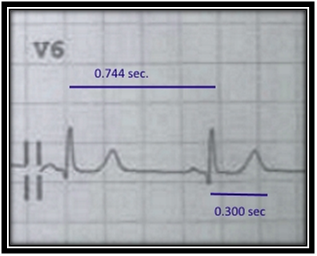
Figure 5 Detail On V6.
QT interval= 0.300 seconds.
RR interval= 0.744 seconds. (HR. to 80, 6 bpm, approx.)
According Bazett formula: QTc =0.347 seconds.
According Fridericia formula: QTc= 0.331 seconds.
By means of both formulas, a shortening of QT interval can be confirmed.
We have previously commented that there is no consensus among authors in many points with reference to this event:
How much should be the length of QTc, (Bazett and Fridericia, mainly), for to be considered as a "Short QT interval?
QTc ≤ 0.350seconds for men. QTc ≤ 0.360 seconds for women.
Clinical follow-up in patients with short QT interval on ECG but who are asymptomatic is necessary?
We think that such clinical follow up is absolutely necessary. Typical symptoms of short QT syndrome can occur at any age. Having the diagnosis of short QT interval on ECG and don'ts clinical follow up would be foolhardy.
What are the best methods of management and treatment?
Have been invoked several drugs as preventive treatments; to date, several antiarrhythmic drugs have been evaluated in patients with a gain-of-function mutation in HERG (KCNH2). The antiarrhythmic effects of IKr blockers such as sotalol and ibutilide have beentested among many others.6 However, the results have been very poor or absent in the overwhelming majority of cases. Facing the high risk for ventricular tachyarrhythmias, the implantable cardioverter defibrillator (ICD) is to date the therapy of choice in patients with a short QT syndrome with symptoms.
But what should we do when the patient has had no symptoms yet?
For parents, when there are no symptoms, there is no disease. Such thing can cause much anguish on them,and for cardiologists is a real challenge. For us this last point is the biggest problem within all the previously mentioned disparities. If we do not make a follow-up to patient on the basis that the person does not has any symptoms, the individual could have sudden severe symptoms. Moreover, if we implant an ICD, the person's life quality can be greatly diminished.
The exposed young girl does not has true symptoms, nor family history and nor genetic disturbances. She just has a short QT interval on her ECG. However, if we ignore such circumstance, the life of the girl could take a sudden and unexpected serious danger at any time.
Therefore, we are able to say without fearing the equivocation how in patients with a shortened QT interval:
How to handle and make a follow-up of these patients (with a demonstrated short QT interval on the electrocardiogram, without symptoms nor genetic alterations, nor family history) is a huge problem for all cardiologists. Once confirmed the electrocardiographic diagnosis of a short QT interval, it results wrenching to comment to parents about it. Besides, the normal life qualityof the infant can be greatly diminished. Clinical events such as exposed herein, cause great ethical problems in all cardiologists who have to comment the obtained results to the parents. It is however our duty to do it.
None.
Author declares there are no conflicts of interest.
None.

©2015 Breijo-Marquez. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.