Journal of
eISSN: 2373-4396


Research Article Volume 1 Issue 7
1Division of Cardiac Surgery, Policlinic of Monza, Italy
2Division of Cardiovascular Anesthesia and Intensive Care, Policlinic of Monza, Italy
Correspondence: Paata Kalandadze, Division of Cardiac Surgery, Policlinico di Monza, via Amati 111, Monza (20052), Italy, Tel 39-039-2810362, Fax 39-035-0779235
Received: November 24, 2014 | Published: December 24, 2014
Citation: Spagnolo S, Kalandadze P, Kalandadze V, et al. Aortic root remodeling and valve sparing “new-old” technique. J Cardiol Curr Res. 2014;1(7):1-6. DOI: 10.15406/jccr.2014.01.00041
Objectives: Different surgical approaches have been suggested for aortic root aneurysm repair. We have developed our technique of aortic root remodeling, based on the plication of the wall of the sinuses of Valsalva and sinotubular junction, and covering the aortic root with tree patches in bovine pericardium.
Methods
Operative procedure: Aorta is resected above the sinotubular junction. The sinuses of Valsalva and the sinotubular junction are plicated. Three patches in bovine pericardium (one for each sinus) are used to cover the aortic root. The patches are fixed to the annulus by three sub annular stitches placed under the nadir of the commissures. The distal end of these patches are fixed at the level of sinotubular junction between one another and commissural aortic wall.
Results: From January 2000 to February 2011 130 patients underwent this operation. There were two hospital deaths. Aortic valve insufficiency was not significant in all but four patients for severe aortic insufficiency required aortic valve replacement during the procedure. In the follow up no significant enlargement of the aortic root was detected. Three patients were reoperated for aortic valve replacement.
Conclusion: With our technique, we remodel the sinuses of Valsalva and sinotubular junction to achieve the normal functioning of the aortic valve, by fixing the aortic annulus and covering the aortic root with three patches of bovine pericardium. We have found advantages in our new method compared with valve sparing and Florida Sleeve procedures.
Keywords: valve sparing, aortic root, aortic ectasia
Forty years ago, Bentall and De Bono1 described a technique for composite aortic valve and root replacement with reimplantation of the coronary arteries. For many years, this operation was the only option for patients with aneurysm of the ascending aorta. In the mid 1990s Yacoub and David independently developed techniques for valve sparing approach with the goal of preserving morphologically intact cusps of the aortic valve.2˗7 In valve sparing surgery preservation of the sinuses of Valsalva which reduces the cusp stress and prevention of dilatation of the aortic annulus are both necessary to obtain long term durability. In last 10years “Florida Sleeve” repair become increasingly popular,8,9 even if this technique was first published by Ergin and Griepp.10 This procedure is more simple and could avoid valve degeneration or annulus dilatation, but it has yet to be established whether this procedure is suitable for patients with specific indications or it is more widely applicable.
We developed our own technique for aortic root repair. Even if this procedure was used for aortic dissection and first published in 1984 by Spagnolo et al.,11 This operation was based on 3 steps: annulus reduction, valve sparing and reinforcement of the aortic root by Dacron patch. Unfortunately the publication was not considered and for many years remains unknown for international audience. Our operation is an alternative to valve sparing and Florida Sleeve operations. This technique allows to repair the sinuses of Valsalva and sinotubular junction, and to stabilize the aortic annulus and aortic root. There is no need for graft sizing and the learning curve for this type of operation is not significant.
Since January 2000, 130 patients with aortic root aneurysm have been operated using our aortic root remodeling technique. Patients mean age was 65, 4years. 127 patients were suffering from aortic root ectasia and three patients had acute aortic dissection. Table 1 shows the clinical profile of the patients. As shown in Table 1 there was significant dilatation of the sinuses of Valsalva and sinotubular junction, which causes severe aortic insufficiency in 12 patients, moderate in 58, mild in 60 and trivial in 11 patients.
Number fo patients |
130 |
Mean age (years) |
65,4(29-84) |
Male/Female |
80/50 |
Aortic ectasia |
127 |
Marfan |
0 |
Aortic dissection |
3 |
Bicuspid valve |
0 |
LVEF(%) |
60.5 ± 6.8 |
Annulus diameter (mm) |
25.2 ± 3.8 |
Sinuses diameter (mm) |
52.4 ± 4.5 |
STJ diameter (mm) |
43.3 ± 4.3 |
Aortic insufficiency (AOI) severe |
12 |
Ao I moderate |
58 |
Ao I mild |
60 |
Ao I trivial |
11 |
Table 1 Patient characteristics
Operative procedure
The patient is monitored with TEE. A standard sternotomy is performed. The arterial cannulation site can be the distal ascending aorta or rarely the femoral artery, depending on the extent of the ascending aortic resection. Venous drainage is provided using a single cannula, unless surgical maneuvers are required on the mitral or tricuspid valves. The heart is arrested in diastole using 750cc of integrate cold blood hyperkalemic cardioplegia. Cardiac arrest is maintained during the operation using cold blood retrograde cardioplegia delivered through a coronary sinus catheter. The aorta is transected distal to the sinotubular junction. The right and left coronary arteries are identified for the underlying tissues (Figure 1). Separation of the right ventricular fibers from the left ventricular outflow tract, at the level of the right commissure, is then performed, to allow the placement of the sub annular stitches later in the procedure. Then the aortic valve is inspected, assessing the thickness and coaptation of the leaflets and prolapse of the cusps. If the leaflets appeared morphologically normal, aortic root remodeling is performed. Our technique consists of four steps:
Covering of the aortic root with three patches in bovine pericardium: Three pericardial patches (one for each sinus) are fixed to the annulus by three subannular stitches, placed under each commissure. The patches are fixed to one another with the same subannular stitch. The distal end of these patches are fixed at the level of sinotubular junction between one another and with commissural aortic wall (Figure 6) (Figure 4 & 7) creating a periaortic wall of the aortic root. The patches are incised over the left and right coronary arteries not to cause compression. Direct end-to-end anastomosis between neo aortic root and ascending aorta is then performed.
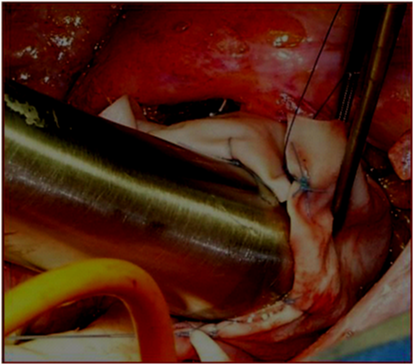
Figure 4 The size of sinotubular junction after the plication must be 15-20% less than the aortic annulus diameter.
Short-term and mid-term outcome
In the 130 patients operated, there were two hospital deaths, one for low cardiac output and another for gastric complications and multi organ failure. Four patients suffered a stroke with complete recovery. Five patients required reoperation for bleeding. There were no coronary complications. Aortic valve insufficiency was not significant in all but in four patients severe aortic insufficiency was detected by TEE in operating room and in these patients aortic valve was replaced during the same operation. Operative results are shown in (Table 2).
Variable |
n |
% |
Hospital deaths |
2 |
1.5 |
Low cardiac output |
1 |
0.7 |
Bleeding |
5 |
3.8 |
Aortic insufficiency |
4 |
3.0 |
TIA |
4 |
3.0 |
Sternal infection |
4 |
3.0 |
Endocarditis |
1 |
0.7 |
Permanent pace-maker |
2 |
1.5 |
Atrail filtration |
30 |
23 |
Prolonged Ventilation |
5 |
3.8 |
Pneumonia |
3 |
2.3 |
Renal complications |
3 |
2.3 |
Table 2 Postoperative complications
No enlargement of the aortic annulus, sinuses of Valsalva or sinotubular junction were detected during the follow-up (mean 6,4years). Three patients were reoperated for aortic valve insufficiency. Post operative and follow up results are shown in (Table 3).
Pts n 124* |
Post-op |
Follow up |
AoI severe or moderate |
0 |
3** |
Ao I mild |
3 |
10 |
Annulus diameter (mm) |
24.8 ± 2.4 |
24.3 ± 2.2 |
Valsalva diameter (mm) |
38.7 ± 3.2 |
38.3 ± 4.2 |
STJ diameter (mm) |
26.3 ± 3.0 |
25.5 ± 5.2 |
EF (%) |
55.7 ± 7.6 |
62.6 ± 4.3 |
Table 3 Results after operation and at follow – up (6.4 years)
*From 130 patients remains 124 (2 death and 4 aortic valve replacement)
**3 patients were re-operated for aortic valve replacement
Comment
Various techniques have been developed for aortic root reconstruction. Bentall operation was used for many years. For 20years, valve sparing operations are valid alternative of Bentall procedure. Valve sparing operations are technically demanding with a small margin of error, both techniques needs coronary reimplantation and aortic root replacement by prosthetic material. Recent publications regarding valve sparing procedures show a trend toward the reimplantation rather than to remodeling technique, because this technique allows stabilization of the annulus. Although reimplantation technique seems to achieve more satisfactory results, according to some authors, it damages the sinus of Valsalva and in long times also the aortic valve.12˗17 In last 10years “Florida Sleeve” operation is becoming popular. Florida Sleeve procedure is easily reproducible and may represent an improvement in aortic root surgery in terms of annulus stability and aortic valve durability. Florida Sleeve procedure seems to be a good alternative to valve sparing operations but its validity needs to be verified by follow up.18
We described our technique for the first time in 1989 19. This procedure is very similar to the Florida Sleeve one, but with some differences:
In our operation, we are remodeling the aortic root in order to obtain normal sized aortic root and sinotubular junction and to ensure aortic valve competence, simply shaping each sinus in the right size and covering neo aortic root with tree patches in bovine pericardium. We are using bovine pericardium instead of Dacron graft because we believe that there is less tissue stress between bovine pericardium and aortic wall rather than between Dacron and aortic wall.
For the patients with aortic root ectasia this operation is a good alternative to Florida Sleeve procedure. Our technique is simple to perform and it gives the possibility to achieve the remodeling of the native aortic root and the stabilization of the valvular annulus and aortic root, by covering the aortic root with pericardial patches. Initial results are satisfactory, showing aortic annulus and root stability. Long-term follow up is necessary to check its validity.
None.
Author declares there are no conflicts of interest.
None.

©2014 Spagnolo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.