Journal of
eISSN: 2373-4396


Research Article Volume 1 Issue 1
1East Boston Hospital, School of Medicine, USA
2Catholic University of Murcia, Campus Jeronimos, Spain
Correspondence: Breijo Marquez FR, East Boston Hospital, School of Medicine, 02128 Trenont St. Boston (MA), USA
Received: April 14, 2014 | Published: April 29, 2014
Citation: Marquez FRB, Rios MP. Shortening of electrical cardiac systole: a new electrical disturbance? short pr and qt intervals in the same electrocardiogram tracing (Breijo pattern). J Cardiol Curr Res. 2014;1(1):6-11. DOI: 10.15406/jccr.2014.01.00002
interval, QT-interval, electrical cardiac systole, tachycardias, syncope, epileptic seizures, short PR, short QT
Despite the convulsive times that we are living as well as the discrepancies and controversies about whether a technique or a drug is better than another is for a specific heart disease, the knowledge of the heart and its mechanical and electrical function is higher every day. For some authors, the electrical cardiac systole only includes the QT interval. That is, the ventricular depolarization and repolarization. For us, must also include atrial depolarization and repolarization (although the latter cannot be seen since it is masked by QRS complex) because if there is not an atrial contraction, ventricular contraction would be impossible. Namely, electrical cardiac systole comprises the full space occupied from the beginning the P wave to the end of the T wave when it reaches the isoelectric line of the ECG.
The discovery of genetic alterations (ionic channelopathies) producing some alterations especially for the electrical cardiac system is being encouraging, although we have not could manipulate the altered genes so far. The management of known altered genes for these diseases types is still far from a reality. Moreover, we can know its genetic cause, the altered gene, but still is away the causal treatment of cardiac diseases; therefore, we have to use conventional handling yet: This is true hitherto. Alterations of the P-R interval (or PQ-interval for others) is well known, both in its shortening as in its elongation (short and long- or atrioventricular block), nevertheless we are discovering new electrocardiographic patterns that can give more light to the true functioning and the processing there of. The P- wave reflects atrial depolarization (contraction).
The PR- interval corresponds to the delay between the end of atrial depolarization (contraction) and the beginning of ventricular depolarization (contraction); its length must be between 0.120 seconds and 0.200 seconds. The Q wave is a negative deflection in the ECG resulting of beginning of ventricular depolarization (first wave in QRS complex).The T wave is a reflection of ventricular repolarization. The QT interval includes a complete ventricular depolarization and repolarization (complete ventricular cycle); its length must be between 0.400 and 0.450 seconds (depending of authors and their conveniences, these values may vary; for us and with a broader context, the normal QTc values are between 0.400 and 0.450 seconds in length). There are many formulas to measure the value of these lengths; the most used are Bazett and Fridericia yet.Like the R-R interval, the QT interval is dependent on the heart rate in an obvious way (the faster the heart rate the shorter the R-R Interval and QT interval) and may be adjusted to improve the detection of patients at increased risk of ventricular arrhythmia.
There are several correction formulas Table 1.
|
Exponential |
Formula |
|
Bazett |
QT/ RR1/2 |
|
Fridericia |
QT/ RR1/3 |
|
Linear |
|
|
Framingham |
QT + 0.154 (1-RR) |
|
Hodges |
QT + 1.75 (HR- 60) |
Table 1 QT Heart Rate Correction Formulas Formulas for QTc measure
The standard clinical correction is to use Bazett's formula and Fridericia’s formula,calculating the heart rate-corrected QT interval: QTc. Bazett's formula QTb= QT-interval / √ 2R-R interval. (The normal values are between 0.400 and 0.450 seconds.) Fridericia’s formula QTf = QT-interval / √ 3R-R interval.(The normal values are between 0,400 and 0, 450 seconds.) The author and his collaborators published a shortening of PR- interval (< 0.12 seconds) alongside a shortening of the QT- interval (< 0.400 seconds) on the same ECG tracing on 2008. We will present in this writing the presence of this pattern, some authors call it Breijo pattern, either alone or associated with other heart pathologies such as Wellens syndrome (or Wellenspattern).
Shortening Of the P-R and Q-T Intervals in the Same Electrocardiographic Tracing. (Breijo Pattern)
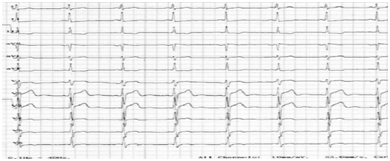
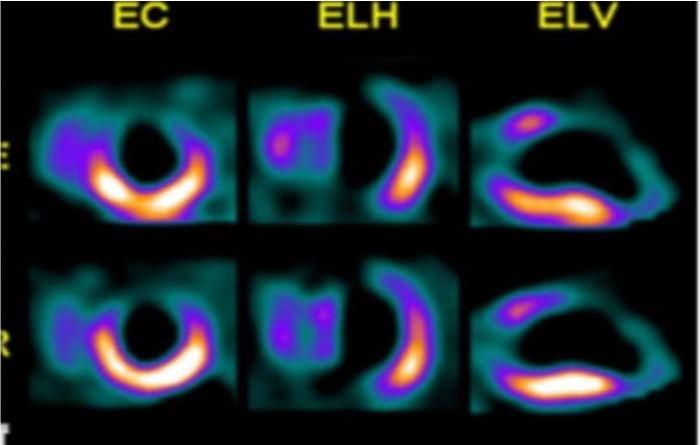
In 2008, Breijo-Marquez and colleagues published an electrocardiographic tracing in which both features could be seen.The PR interval was lower than 0.120 seconds and the corrected QT interval was lower than 0.350 seconds.They called it "Decrease of electricalcardiac systole".1 also has been entitled as “Accelerated atrioventricular stimulation with an early and shortened ventricular repolarization in the same individual.2 People who had this kind of electrocardiographic pattern, had also suffered from a wide variety of symptoms. Nocturnal tachycardias, dizziness, seizures, and unexplained syncopal accesses were the main symptoms common to all patients. Were diagnosed as epileptics and treated with specific drugs for epilepsy all patients; the results with such treatment were null. However, the electroencephalographic registers did not provide any visualization for epileptogenic focus in any of assessed patients. The patient age ranged from 16 to 40 years. The male gender was predominant. All previous electrocardiographic studies were considered within normal ranges. A plentiful study with specific tests for the heart was done at our hospital: Blood Analysis (with electrolytes); Electrocardiography; Holter study; Stress test (Bruce protocol), Echocardiography, EEF, Angiography, and SPECT were done with informed consent of both patient and hospital. Calcium; Chlorine;Magnesium;Phosphorus; Potassium; Sodium, CK-MB; LDH (1.2); CPK; Troponins (nIc, nTc) were assessed. We also added determinations of blood levels of lithium. All parameters analyzed were within normal ranges except Lithemy: All patients had very low levels of lithium in blood (100%), with lower values than 0.1 mEq / l. Stress test (Bruce protocol), Angiography, Echocardiography and SPECT also were within of normal ranges. In electrocardiography and Holter study we can be seen a shortening of PR and QT intervals (Figure 1).
Abstract
We will present a clinical condition characterized by the presence of a short PQ interval and a short QT interval in the same individual. The Short PQ syndrome is characterized by a duration <0, 120 seconds. We know its variants. The short QT syndrome has been described recently (2000-03). We speak of short QT if its length is < 0.400 second. Both are known individually. However, there is an electrocardiographic pattern little known until today: A pattern with short "PQ-interval and QT-interval” in the same ECG tracing.
The QT interval is a reflection of ventricular repolarization.3–5 Its upper normal limits are well known, and the prolongation of QT interval above these limits, it is considered an independent risk factor for sudden death. There are many information on syndromes congenital and acquired long QT and its relationship to mortalit.3,4 By contrasting, little is known about the causes and prognostic value of Short QT interval.5–7 It is difficult to know the index of this syndrome. Although only a few cases have been reported, the rate may be underestimated, because, until now, little attention has been focused on the diagnosis of short QT electrocardiogram.6,7 Patients with short QT syndrome have a wide clinical spectrum including palpitations, tachycardia, episodes of syncope and sudden cardiac death, and a family history of it through several generations.5–7 We have demonstrated the presence of this pattern in several persons with symptoms of childhood convulsions-diagnosed as epilepsy despite not display any epileptic focus on studies of electroencephalography (EEF)–as well as nocturnal tachycardia crisis and syncope events related to repetitive physical effort.8–10
For some authors, the electrical cardiac systole comprises only the QT interval (ventricular cycle),11 but we think that the depolarization atrial must be included.1–10
Electrical cardiac systole comprises
Atrial depolarization (P wave). PQ-interval. Ventricular depolarization (QRS complex). ST Segment. Ventricular repolarization (T wave). In many cases, the determination of the end of the T wave is very difficult to calculate. In Medicine and specifically in Cardiology, QT interval is a measure of time between the start of the Q wave and the end of the T wave (the heart's electrical cycle). The presence of this configuration with a shortening of intervals PQ and QT represent a major cardiac instability, and consequently a high risk for serious cardiac arrhythmias (ventricular fibrillation fundamentally) and therefore also for sudden cardiac death.7
A thorough compilation of patients with this kind of symptoms such as infantile convulsions non-responders to conventional treatments, bouts of nocturnal tachycardia with sudden character, and syncopal events related to the effort. An exhaustive study of personal antecedents as well as yours current clinical situation. An exhaustive measurements of intervals, segments and electrocardiographic waves. Measurement technique: MioLaserTool ®, Pixruler ® &Cardiocaliper®.
By way of example,we will expose the following case:
A 37-year-old man with many nocturnal tachycardia crisis (since childhood) and three syncopal events observed and related with physical stress. In his family background, two sudden deaths were found: father died at age 55 yearsfor sudden cardiac and a brother died at 22 months by sudden infant death. He was diagnosed in his Reference Hospital (where he was transferred by emergency services) with supraventricular tachycardia to 195-200 beats per minute(Figure 2), with narrow QRS complexes. Severe diaphoresis, with paleness of skin and mucosa. A severe arterial hypotension to 90/50 mm. Hg. Cardiac auscultation was in normal ranges but with a rapid rhythm. Tachypnea to20 cycles/minute. A grade Stuporous (Glasgow 15/15). The neurological examination was within normal ranges without focalizations. Central and peripheral pulses were palpable, symmetric and synchronous in "frecuens". Supraventricular tachycardia disappeared by means of the administration of two doses of Adenosine i.v. in bolus, with six mgrs. each one in 1 minute (Figure 3). A Hospital discharge was made after full stabilizing of acute process and patient was derived to your cardiologist outpatient, with the follow diagnosis:
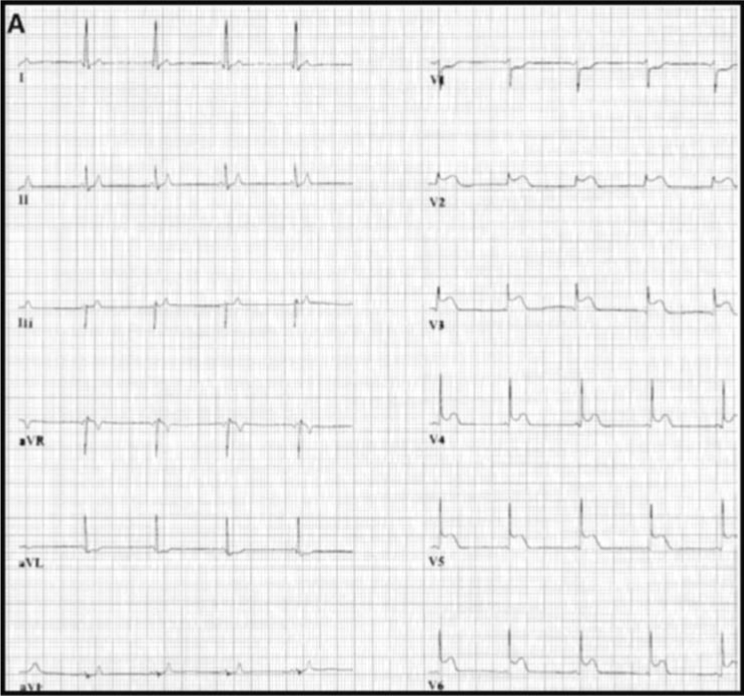
A paroxysmal supraventricular tachycardia and Crisis of anxiety. The patient was transferred to our Hospital because he had had a similar event as the exposed, after the first visit with his outpatient cardiologist. There, the patient was adequately assessed with electrocardiogram, echocardiogram, blood levels of ions and cardiac markers as well as electro-physiological study (EEF) (Figure 4). He was negative for high levels of Troponin (I-T), CK, CPK-MB and however he was positive for a low levels of lithium ion (<0.1 mEq/L) In a detailed assessment on ECG, we can note that the patient has a short PQ- interval with a short QTc in the same ECG tracing (Bazett and Fridericia formulas) with a risk of sudden cardiac death, according to the Schwartz scale12 of 4.5 points: High risk for sudden cardiac death. At first glance, the ECG tracing interpretation suggests a syndrome Lown - Ganong - Levine, but in a more detailed checkup we see as the QTc interval in the LGL syndrome is normal while in this patient, the QTc interval is short (<0.350 s). We have therefore two possibilities: an unknown variant of LGL Syndrome or a new electrical cardiac disease.
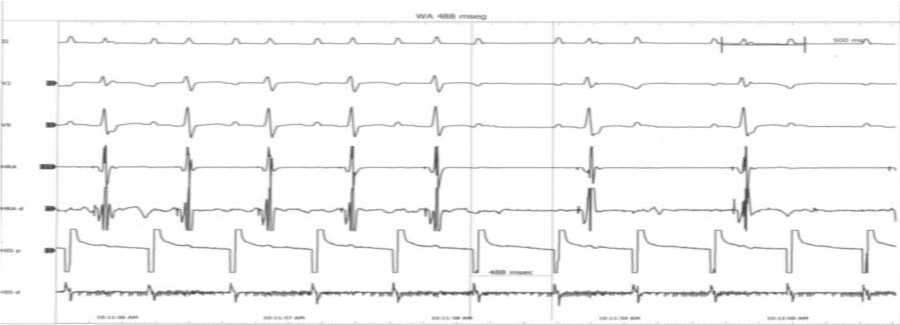
Both PQ and QT intervals are short (Figure 3-5).

PQ- interval: 0.10 - 0.11 seconds. RR- interval: 0.862- 0.900 seconds. QT- Interval:0.322-0.330 seconds. Bazett’s formula: 0.339-0.343 seconds. Fridericia’s formula: 0.330-.337 seconds.
An electrical heart feature that has not been described at present with decreased duration of electrical cardiac systole: PQ and QTc-intervals are short (for some authors, it has been called "Breijo Pattern").
To reduce its more than likely underdiagnosis, all doctors should measure segments, intervals and waves electrocardiographic in all ECG tracings. A new electrical cardiac disease or pattern may have been discovered. Thisdescribed patient is not the only one in our collection, but just one example. Raising awareness among doctors of the existence thereof is prescriptive. Avoid preventable sudden deaths is the duty of all doctor, therefore knowledge of this characteristic electrocardiogram alongside clinical features patient should be a commandment.
Presence of a critical stenosis of the left anterior descending coronary artery alongside a short "pr and qt" pattern, in a single electrocardiogram record
(wellens pattern together to breijo pattern)
wellens syndrome, short, PR-interval, short QT-interval, electrical cardiac disturbances
The knowledge on the heart and its functions is greater and better, day after day. Nevertheless, many cardiological entities are undocumented yet.
The knowledge on the heart and its functions is greater and better, day after day. Nevertheless, many cardiological entities are undocumented yet.One of them might be the presence of Wellens's syndrome together with a pattern of shortened “PR and QT “(Breijo Pattern) in a single electrocardiography record.Both have a great incidence of an underdiagnosis. The risk that can bring the above mentioned sub-diagnoses could have lethal consequences, because to the problems inherent of the Wellens’s Syndrome, could be added the own ones of a short "PR-QT" (Figure 6).
Here, we show to readers so much the clinical description as ECG recording of a male who have the previously mentioned association.He is 42 year-old male, unmarried, occasional smoker, arterial hypertension in treatment with felodipine (5 mgrs/day) and ramipril (5 mgrs/day), who was diagnosed of unstable angina (Prinzmetal’sAngor).He was immediately hospitalized because the patient had commented an intense, oppressive and progressive chest pain without relation with the physical effort. The pain was radiating towards both jaws. It was accompaniedof a great vegetativesymptom.
The administration of sub-lingual nitrites turned out to be effective, so much in the improvement of the pain as in ECG's alterations that the patient was presenting (elevation of the segment ST for more of 2 mm. in all the precordial leads). The enzymatic tests in blood were positives for a coronary ischemia:LDH: 1.220 UI/L. CK: 560 U/L. CPK-MB: 580 U/L. AST: 376 U/L. ALT: 121 U/L. Troponine I: 3, 5 µg. /L. These parameters together to the features of the ECG recording and of the clinical picture were catalogued like an unstable angina variant (Prinzmetal'sAngor). As soon as, according your physicians, was stabilized so much clinically, as of the enzymatic levels, was recommended to come back his home and to return to the hospital in ten days for a new valuation (the anomalies in the ventricular repolarization were catalogued like an evolutionary variation of the common unstable angina by the doctors). Nevertheless, before of the ten days recommended, the patient returns describing a similar clinical picture to the previous one but of more intensity and duration.It is for it that, the patient goes on to the services of intensive care and was diagnosed for Wellens's Syndrome because he fulfils the criteria for it (the patient was submitted to a diagnostic battery, including, an angiographic study, an echo-cardiogram and a study with SPECT, like we can see below, in the iconography).It would be interesting to comment that, in his personal precedents, there were documented three accesses of syncope(of short duration) with a complete recovery, as well as several accesses of nocturnal palpitations, whichwere diagnosed of supraventricular tachycardias. In his familiar precedents, one sudden death (not catalogued) was documented in his paternal uncle at the age of 46 year-old. His father has also suffered a heart attack of antero-lateral localization. So-called Wellens syndrome is a variant of unstable angina.13Clinically, patients suffer similar symptoms: severe chest pain, oppressive and pain radiations to different sectors, of short duration and responding to the administration of nitrites.
Electrocardiographically, patients have very characteristic patterns: symmetrical inversion and, sometimes, deep T-waves in precordial leads, especially in V3-V4, although these features may extend to all precordial leads. Wellens syndrome is associated with a critical stenosis of the left anterior descending coronary artery (LAD) (Figure 7).13,14
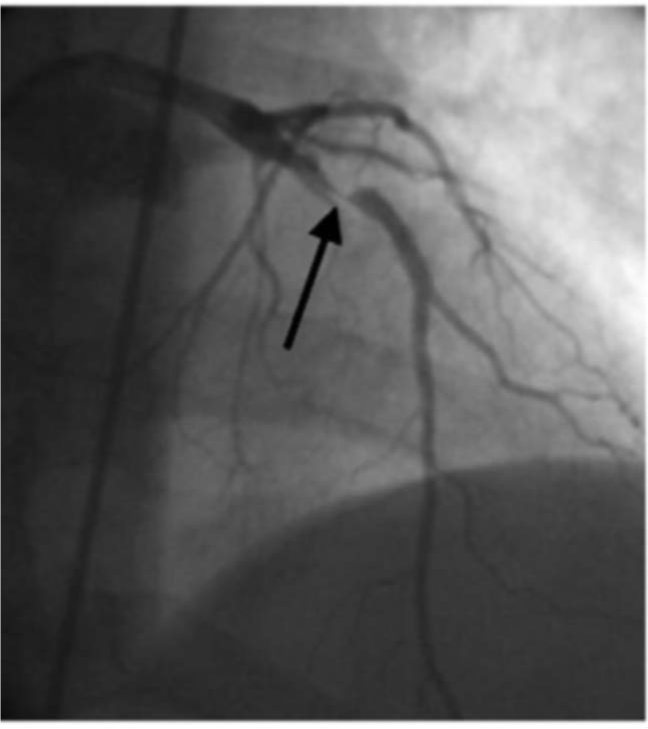
Perhaps the most important aspect of this pattern or syndrome is the great capacity it has to develop in less than 10 days (after identification by electrocardiogram) a massive myocardial infarction in the anterior wall of the ventricle (Figure 8). The electrocardiographic pattern of "short PR interval alongside a short QT interval” was described by Breijo et al. in 2008.1,2 It ischaracterized by the presence in the electrocardiogram of a PR interval of less than 0.120 seconds alongside a QT interval of less than 0.400 seconds (Ie, a reduction in the duration of cardiac electric systole1 and that over 80% cases, are accompanied by syncopal events, nocturnal tachycardias and, sometimes, ventricular fibrillation and, even, sudden death.
The key to accurate diagnosis for both entities must begin with a detailed analysis of all symptoms reported by the patient; the ECG recording provides almost definitive confirmation: The features of the T wave in precordial leads. The length of PR and QT intervals.
None.
Authors declare that there is no conflict of interest.

©2014 Marquez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.