Journal of
eISSN: 2473-0831


Research Article Volume 2 Issue 2
Correspondence: Marcellin Guiaro Ndoe, Department of Biomedical Sciences, Faculty of Science, University of Ngaoundere, Ngaoundere, Cameroon
Received: April 16, 2016 | Published: April 27, 2016
Citation: GuiaroNdoe M, Fak ODM, Mbarawa IKM, NestorOumarou J, Fadimatou DBH, et al (2016) Malaria and Biochemical Disorders among Patients Infected with HIV, under HAART at the Bertoua Regional Hospital (Cameroon). J Anal Pharm Res 2(2): 00017. DOI: 10.15406/japlr.2016.02.00017
The biochemical parameters are part of the follow-up care for patients with malaria bout as gravity markers allowing the biologist to inform the doctor about the progressive stage of the malaria bout. Among these markers, we have on the one hand; the ions Sodium, Potassium and Chloride and on the other hand; the blood sugar, the bilirubin and the proteins, which represent the biochemical parameters more used during the biological check-up of the malaria. Indeed a non negligible fraction of deaths occurring during the malaria among patients infected with HIV under HAART is associated to biochemical disorders, from where the interest of this transversal survey carried out at the Regional hospital of Bertoua, aimed at evaluating the variations of biochemical parameters associated to the malaria bouts, due to P. falciparum among these patients. We included in our survey, all HIV positive patients under HAART since at least one year and presenting a malaria bout. We excluded from our survey, all HIV positive patients, unregistered in our study place for the follow-up care for antiretroviral therapy; all HIV positive patients presenting a preexisting hepatic, renal or cardiovascular pathology before the intake of the HAART; and the pregnant women. We analyzed the socio-demographic parameters (Age and Sex), the Biological parameters (parasitic charge, Blood sugar, ions potassium, sodium and chloride, urea, creatinine, bilirubin, protein, HIV serology, rate of hemoglobin and level of CD4) and the therapeutic parameters (therapeutic protocol, length of hospitalization and treatment evolution). During this survey, we noticed that the ionic disorders as the decrease of sodium ion and the increase of the potassium ion and chloride ion in the blood were more frequent during the malaria bouts among our patients infected with HIV under HAART. The blood sugar was also decreased in the blood. The bilirubin and protein were increased in the blood and also present in the urine. The increase of the creatinine and urea had the incidence rates of 100% among these patients. The frequency of these biochemical disorders varied with a meaningful manner according to the gravity stage of illness (simple or serious malaria bout) and was also influenced by the intake of the HAART.
Keywords:malaria, HIV, HAART, biochemical disorders
The malaria is a disease due to the presence and to the development in the liver then in the red blood cells, of a parasite called Plasmodium. It is transmitted by the infesting sting of the mosquito female belonging to the kind Anopheles. This affection constitutes a major problem of public health in the world, especially in the tropical regions. According to the world organization of health, more of 2 billions of people are exposed to the malaria bouts and about 112 million cases of malaria are counted in the world. One estimates to 1 death by malaria all 20 to 25 seconds in the world. In Cameroon, the malaria stays the major endemic and the first reason of morbidity and mortality in the most vulnerable groups, to know the children of less than five years and the pregnant women. The sanitary statistics reveal that it is responsible for 35 to 40% of deaths in the sanitary formations: 50% of morbidity at the children of less than 5 years, 40 to 45% of the medical consultations and 30% of the hospitalizations. The malaria is also the reason of 26% of the absences in professional environment and 40% of the expenses of health of the households.1 This infectious illness has a death rate at the present time similar to the one of the AIDS. In the literature that we have had, very little study has been achieved on the different epidemiological, clinical and biological aspects of the association of the malaria with VIH/SIDA. The malaria at the time of its febrile bout also comes with a decrease of lymphocytes in particular a fall of CD4, as is the case with the AIDS.2 A few isolated cases of publications conclude the absence of influence of the malaria on the HIV status.3 Several other studies made in the population of born children of seropositive mothers, in a population seropositive adults in general, showed that the malaria could not be considered like an opportunist infection to the AIDS, and that no difference exists between these two infections in the incidence, the severity, or the answer to the anti-malaria treatment.4 The malaria at the time of its pathogenesis, come with the biochemical disorders which are at the basis of major physiopathological problems during the malaria bouts. Indeed, in the simple malaria bout, they announce its aggravation toward the serious access; and during the serious access, they are the markers of the bad prognosis taking in danger the patient’s life. Among them, we have on the one hand; the ions Sodium, Potassium and Chloride and on the other hand the Blood sugar, the bilirubin and the Proteins, which represent the biochemical parameters more used during the biological check-up of the malaria. This work is a transversal survey, carried out at the Regional hospital of Bertoua, aimed at evaluating the variations of biochemical parameters associated to the malaria bouts, due to P. falciparum, among patients infected with HIV, under HAART.
We performed a prospective transversal survey from June 2015 to November 2015 at the service of adult medicine of Bertoua regional hospital on a study population constituted of two groups of patients, which one group only presented a coinfection parasitic HIV-Plasmodium and the other group, the malaria without HIV. The general objective of this study was to determine the impact of the HAART on the biochemical parameters of patients presenting a coinfection parasitic HIV-Plasmodium. We included in our survey, all HIV positive patients under HAART since at least one year and presenting an affection of malaria. We excluded from our survey, all HIV positive patients, unregistered in our study place for the follow-up care for antiretroviral therapy; all HIV positive patients presenting a preexisting hepatic, renal or cardiovascular pathology before the intake of the HAART; and the pregnant women. We analyzed the socio-demographic parameters (Age and Sex), the Biological parameters (parasitic charge, Blood sugar, ions potassium, sodium, and chloride, urea, creatinine, bilirubin, protein, HIV serology, rate of hemoglobin and level of CD4) and the therapeutic parameters (therapeutic protocol, length of hospitalization and treatment evolution). The HIV positive patients in addition to their tritherapy which was constituted of 2 INTI+ 1 INNTI (AZT+3TC + Efavirenz, that is 34.4% or AZT + DDI+ Nevirapine, that is 29.6%) or of 2 INTI + 1 IP/r (D4T+3TC+Lopinavir/Ritonavir, that is 36%) received also the same anti-malaria treatment that the group of non-infected patients with HIV to know: PO quinine (37.2%), Artemether (19%), salts of quinine in drip (43.8%). The participants to the survey signed an informed consent after have been informed verbally on the aim of the survey as well as on its advantages and inconveniences. The gotten results have been analyzed with the help of the 2.13 version of R software. The ANOVA and Chi-Square tests have been used to compare the averages and percentages and P < 0.05was considered significant.
We collected 353 cases of malaria during our period of survey. 121 (34.3%) cases answered our inclusion criteria’s which 64 (52.9%) cases had a positive serology to the HIV associated with a malaria bout and 57 (47.1%) cases had a negative serology to the HIV associated with a malaria bout.
Distribution of the 2 groups of patients according to the age groups
The average age was 39.29 years ±12.05 with ages ranging between 10 to 50 years. The age group of 20 to 30 years was the most represented; with 45% and 41% respectively for the patient’s group with malaria and HIV and the patient’s group with malaria without HIV (Figure 1). The percentage differences were statistically meaningful with a P value = 0.0002 (P <5%).
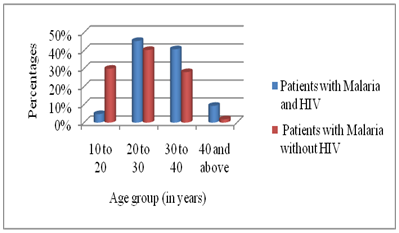
Figure 1 Graphical representation showing the distribution of the 2 groups of patients according to the age groups.
Distribution of the 2 groups of patients according to the gender
The feminine sex was the most represented in patient’s two groups with 59.3% for the patient’s group with malaria and HIV and 56.1% for the Patient’s group with malaria without HIV (Table 1). Their sexes ratio respective were 0.68 and 0.78 in favor of women.
|
Group of Patients Gender |
Patients with Malaria and HIV |
Patients with Malaria without HIV |
|
Men |
26 (40.7%) |
25 (43.9%) |
|
Women |
38 (59.3%) |
32 (56.1%) |
|
Total |
64 (100%) |
57 (100%) |
Table 1 Showing the distribution of the 2 groups of patients according to the gender
P value= 0.15 (P>5%)
Distribution of the 2 groups of patients according to the type of malaria
The simple malaria bout was the most represented in the patient’s group with malaria without HIV with 66.7%, contrary to the patient’s group with malaria and HIV where the serious malaria bout was more represented with 79.7% (Table 2).
|
Group of Patients Malaria’s type |
Patients with Malaria and HIV |
Patients with Malaria without HIV |
|
Serious Malaria |
51(79.7%) |
19 (33.3%) |
|
Simple Malaria |
13 (20.3%) |
38 (66.7%) |
|
Total |
64 (100%) |
57 (100%) |
Table 2 Showing the Distribution of the 2 groups of patients according to the type of malaria
P value= 3.915e-12 (P <5%)
Comparison of hemoglobin rates among the 2 groups of patients
We didn’t notice any rate of hemoglobin >10 in the patient’s group with malaria and HIV (Table 3). The average of hemoglobin rates of these patients was 6g/dl±1.09 and the one of patient’s group with malaria without HIV was 8g/dl±6.01 (Table 3).
|
Rate of Hemoglobin (g/dl) Group of Patients |
< 5 |
5-10 |
> 10 |
Total |
|
Patients with Malaria and HIV |
36(56.2%) |
28(43.8%) |
0 |
64(100%) |
|
Patients with Malaria without HIV |
18(31.6%) |
25(43.9%) |
14(24.5%) |
57(100%) |
|
Total |
30(24.8%) |
54(44.6%) |
14(24.5%) |
121(100%) |
Table 3 Showing the Distribution of the 2 groups of patients according to the hemoglobin rates
P value= 0.001(P <5%)
CD4 level of our patients under HAART
The biggest part of our patients had a rate of CD4 found between 150-50 Lymphocytes/mm3 of blood that is an enrollment of 40 patients with a rate of 62.5% (Table 4).
|
CD4 (Lymphocytes/mm3) |
Numbers |
Percentages |
|
250-200 |
13 |
20.30% |
|
200-150 |
8 |
12.50% |
|
150-100 |
18 |
28.10% |
|
100-50 |
22 |
34.40% |
|
Inferior to 50 |
3 |
4.70% |
|
Total |
64 |
100% |
Table 4 Showing the patients' distribution under HAART according to the CD4 level
P value=0.06 (P>5%)
Correlation between Biochemical disorders and malaria
The increase of creatinine and urea, were the biochemical disorders most represented in the patient’s group with malaria and HIV, with incidence rates of 100%; contrary to the patient’s group with malaria without HIV, where the decrease of blood sugar and potassium ion were the biochemical disorders most represented with respective incidence rates of 71.9% and 66.7% (Table 5).
|
Parameters |
Sodium Ion (mmol/L) |
Potassium Ion (mmol/L) |
Chloride Ion (mmol/L) |
Blood Sugar (g/l) |
Creatinine (mg/dL) |
Urea (mg/dL) |
Bilirubin (urine) |
Protein (urine) |
||||||
|
Patient’s Group |
<N |
>N |
<N |
>N |
<N |
>N |
<N |
>N |
<N |
>N |
<N |
>N |
P |
P |
|
Patients with Malaria and HIV |
84.30% |
14.80% |
89.10% |
89.10% |
6.20% |
81.30% |
11% |
68.70% |
0 |
100% |
0 |
100% |
-90.60% |
-70.30% |
|
133±86.13 |
151±36.86 |
2.96±1.05 |
7.08±2.56 |
92±38.95 |
125±42.03 |
0.7±0.16 |
2.42±0.65 |
1.86±0.15 |
52±10.13 |
|||||
|
Patients with Malaria without HIV |
64.90% |
3.50% |
66.70% |
8.80% |
17.60% |
21% |
71.90% |
19.30% |
0 |
21% |
0 |
(24.6) |
(73.6%) |
(59.7%) |
|
129±15.99 |
154±64.20 |
2.68±1.52 |
6.05±2.01 |
93±13.02 |
116±35.42 |
0.62±0.24 |
0.8± 0.24 |
1.3±0.25 |
45±8.23 |
|||||
|
P value |
0.009 |
0.005 |
0.82 |
0.02 |
0.0002 |
1.72E-12 |
0.002 |
0.0008 |
||||||
|
r |
0.05 |
|
-0.004 |
|
0.009 |
|
0.03 |
|
0.01 |
|
0.06 |
|
0.003 |
0.12 |
Table 5 Showing the distribution of the 2 groups of patients according to the biochemical disorders linked to the malaria
<
N, superior to the normal; P, positive; Accepted significance=5% for P.value; r, correlation coefficient/p>
Comparison of the length of hospitalization of our patients
The average length of hospitalization of the patient’s group with malaria and HIV was 37±12 days with extremes from 3 to 112 days and the one of the patient’s group with malaria without HIV was 33±15 days with extremes from 2 to 60 days (Table 6).
|
Length of Hospitalization (in Days) Group of Patients |
1-50 |
51-100 |
>100 |
Total |
|
Patients with Malaria and HIV |
6 (9.3%) |
13 (20.3%) |
45 (70.4%) |
64 (100%) |
|
Patients with Malaria without HIV |
13 (22.8%) |
29 (50.9%) |
15 (26.3%) |
57 (100%) |
|
Total |
19 (15.7%) |
42 (34.7%) |
60 (49.6%) |
121 (100%) |
Table 6 Showing the distribution of the 2 groups of patients according to the length of hospitalization
P value= 0.004 (P <5%)
Comparison of treatment evolutionof our patients
The biggest part of our patients had a health improved with 95% of cases (Table 7).
|
Treatment Evolution Group of Patients |
Improved |
Lost of View |
Death |
Total |
|
Patients with Malaria and HIV |
58 (90.6%) |
1 (1.6%) |
5 (7.8%) |
64 (100%) |
|
Patients with Malaria without HIV |
57 (100%) |
0 |
0 |
57 (100%) |
|
Total |
115 (95%) |
1 (1%) |
5 (4%) |
121 (100%) |
Table 7 Showing the distribution of the 2 groups of patients according to the treatment evolution
P value= 0.41 (P>5%)
Our survey returns a sample size of 121 cases of malaria bout, divided between 2 patient’s group, which 64 cases presented a positive serology to HIV (52.9%) and 57 cases had a negative serology to HIV (47.1%).
In our survey, The feminine sex was more represented in the two groups of patients with 59.3% for the patient’s group with malaria and HIV and 56.1% for the patient’s group with malaria without HIV (P value = 0.15). Their respective sexes ratio were 0.68 and 0.78 in favor of women (Table 1). The young adults were more represented in the two groups of patients, with a general average age of 39.29 years ±12.05 and the extremes from 10 to 50 years. The most represented age group was the one of 20 to 30 years with respective rates of 45% for the patient’s group with malaria and HIV with and 41% for the patient’s group with malaria without HIV (P value = 0.0002) (Figure 1). These results could justify themselves by the fact that these young adults represented the biggest part of our survey population. The women represent 57% of people living with HIV in Sub-saharan Africa.5 These results come closer to those found by BIAPO KAYO in Mali in his survey on the coinfection HIV/AIDS with Malaria at the point “G” hospital, which returned a average age included between 26 to 36 years for these two groups of patients with 58.3% for the feminine sex and a sex-ratio of 1.39 in favor of women.6
The serious malaria bout was more represented in the patient’s group with malaria and HIV with 79.7% contrary to the patient’s group with malaria without HIV where the simple malaria bout was more represented with 66.7% (P value = 3.915e-12) (Table 2). The average of hemoglobin rate of the patient’s group with malaria and HIV was 6 g/dl±1.09 and the one of the patient’s group with malaria without HIV was 8 g/dl ± 6.01 (P value = 0.001) (Table 3). This average difference to the level of hemoglobin rates among the patient’s group with malaria and HIV, could explain itself by the intake of the hematotoxic ARV drugs (toxic for the blood cells) as the zidovudine (AZT) which is added to the presence of malaria which also affects the red blood cells of these patients. The HAART has an impact on the hemoglobin rate of patients infected with HIV. This hypothesis could give an explanation to the survey made by BIOPO KAYO in Mali.6 This result is also comparable to the one obtained by Kone, who found 70% of anaemia among patients affected with HIV in his survey on the coinfection malaria with HIV at the point “G” hospital in Mali.7 The survey made by Moyle, showed that the AZT has a negative impact more important on the hematological parameters compared to d4T.8 It come to reinforce our results because the Zidovudine (AZT) has been used with a rate of 64% by our HIV positive patients with malaria.
We noted an important decrease of the sodium ion in the blood of patients belonging to the patient’s group with malaria and HIV (Table 5). The potassium ion, chloride ion, urea and creatinine were also very increased in this patient’s group (Table 5). The averages of these different biochemical disorders among this patient’s group with malaria and HIV were very superior to those observed in the patient’s group with malaria without HIV. These results are comparable to those obtained by Bagnis in his survey on the Prevalence of the hydroelectrolytic and acido-basic disorders among patients infected with HIV.9 The biggest part of the electrolytic disorders observed in the cases of malaria could be in relation with acortico-suprarenal insufficiency. Indeed these suprarenal glands undergo a lipidic depletion, edema, thrombosis, hemorrhage, necrosis and cellular infiltration.10 Among the HIV positive patient with malaria, these electrolytic disorders are more accentuated with the intake of nephrotoxic ARV drugs (toxic for the kidney) as the Ritonavir, the Didanosine and the Efavirenz, which have been used in our survey.
The hypoglycemia was more represented in the patient’s group with malaria without HIV with 71.9% and an average of 0.62 g/l ± 0.24, contrary to the patient’s group HIV positives where the hyperglycemia was more represented with 68.7% and an average of 2.42g/l ± 0.65 (P value = 0.02) (Table 5). We noted during this survey that the blood sugar of the patients under HAART which was increased before their malaria bout and who presented an increased parasite charge, has known an important reduction (nearly close to the normal) during their hospitalization follow from the malaria. The hyperglycemia observed among the patient under HAART, is more often caused by the long-term intake of the protease inhibitors, which disrupts the working of the insulin and provoke diabetes due to medicaments.11 The hypoglycemia observed in case of malaria, would probably be linked to factors as: the consumption of glucose by the parasite,12 an increase of insulin in the blood stimulated by some factors derived from the parasite and also by the treatment to quinine,13 the inhibition of the gluconeogenesis and production of cytokines.10 The presence of these factors among these HIV positive patients with malaria under HAART, could give an explanation to this return of the blood sugar nearly close to the normal.
The incidence rate of bilirubin in the urine (Bilirubinuria) was more increased in the group of HIV positive patients with malaria, that is 90.6% (P value = 0.002) (Table 5). The presence of bilirubin excess in blood observed in case of malaria is generally secondary to a hemolytic icterus (destruction of red blood cells by the parasite), however its presence in the urine doesn’t necessarily translate a hemolysis, but generally a hepatitis or an obstruction of the biliary ways. Among the patient under HAART this presence of the bilirubin in the urine would be linked to the presence of the plasmodium, malaria’s parasite which develops itself in hepatic cells, also coupled to the intake of hepatotoxic ARV drugs (ARV drugs toxic for Liver). This result is comparable to the one gotten in the survey made by Busti on a same survey population, who returned an incidence rate of 49% for this biochemical disorder.14
The incidence rate of the protein in the urine (Proteinuria) was also increased in the patient’s group with malaria and HIV, that is a rate of 70.3% (P value=0.0008) (Table 5). Generally among patients with serious malaria bout, we can observe an overload proteinuria which doesn’t translate a renal attack. It results from the presence of an important quantity of low molecular weight proteins in the plasma, which exceeds the tubules reabsorption capacity.15 Among HIV positive patients with malaria, this overload proteinuria is coupled to a renal attack caused by the intake of nephrotoxic ARV drugs (ARV toxic for kidney). It could explain the increase of the incidence rate of proteinuria among these patients in case of malaria. This justification is similar to the one given by Schwartz in his survey entitled highly active antiretroviral therapy and the epidemic of HIV+ end-stage renal disease.16
The average hospitalization length of HIV positive patients with malaria was 37±12 days with extremes from 3 to 112 days and the one of the patient’s group with malaria without HIV was 33±15 days with extremes from 2 to 60 days (Table 6). This long hospitalization length observed in the patient’s group with malaria and HIV could be due to the presence of the pathologies associated to their serological status. The patient’s group with malaria without HIV had a clinical recovery rate of 100%, contrary to the patient’s group with malaria and HIV, where we had recorded 58 cases of clinical recovery of the malaria (90.6%), 1 case of lost of view (1.6%) and 5 cases of death (7.8%) (Table 7). We had not done a malaria control at the end of treatment to attest the absence of the parasite among the patients who had a clinical recovery. Kone during his survey on an identical population to ours returned a mortality rate of 23.3%.7
This study aimed at evaluating the variation of the biochemical parameters during the malaria bouts due to P. falciparum among patients infected with HIV, under HAART since at least one year. During this survey, we noticed that the ionic disorders as the decrease of sodium ion, the increase of potassium and chloride ions, were frequent during the malaria bouts among our patients infected with HIV under HAART. The increase of the creatinine and urea had incidence rates of 100% among these patients. The frequency of these biochemical disorders varied with a meaningful manner according to the gravity stage of the illness (simple or serious malaria bout) and was influenced also by the intake of the HAART. This survey has also known limits as the financial resources, which didn’t allow us to explore the malaria impact on the other biochemical parameters as: Magnesium, iodine and calcium ions, the transaminases, cholesterol, uric acid etc…. among these patients. We also noticed that all our patients under HAART, who presented a hyperglycemia before their malaria bout (serious), have known an important decrease of their blood sugar due to an elevated parasitic load, as if the parasite consumed the glucose. This hypothesis could be used in the fight against the insulin dependency from the diabetic patients. We could use in the future the molecular biology techniques to create a transgenic plasmodium which consumes the glucose as being protected of the pharmacological effects of the antimalarial drugs and which will be put in the blood circulation of the diabetic patients.
All authors contributed to the designing, preparation, editing, and final review of the manuscript.
Authors thank the collaborators of their respective institutions for the comments on the manuscript.
Authors declare that there is no conflict of interest.

©2016 GuiaroNdoe, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.