Journal of
eISSN: 2373-6437


Case Report Volume 9 Issue 1
1Surgery, Om Surgical Center & Maternity Home, India
2Thoracic Surgery, Sir Ganga Ram Hospital, India
Correspondence: Pankaj Srivastava, Laparoscopic, Thoracic, Thoracoscopic & VATS Surgeon, Om Surgical Center & Maternity Home, SA 17/3, P-4, Sri Krishna Nagar, Paharia, Ghazipur Road, Varanasi, UP, India, 221007, Tel +91-542-2586191, Fax +919415226817
Received: October 23, 2017 | Published: October 25, 2017
Citation: Srivastava P, Kumar A, Asaf BB (2017) Tracheal Reconstruction under Cross-Field Anesthesia. J Anesth Crit Care Open Access 9(1): 00331. DOI: 10.15406/jaccoa.2017.09.00331
Tracheal stenosis often has an iatrogenic origin and results from artificial ventilation combined with intubation or tracheostomy employed as a life-saving, emergency procedure. In spite of a considerable improvement in the conditions of managing patients with life-threatening conditions, the issue of tracheal stenosis is ever present. We present a case of tracheal reconstruction under the cross-field anesthesia in a 20-year-old male having tracheal stenosis following endotracheal intubation and tracheostomy as well in his due course of treatment for the alleged gunshot injury.
Keywords:tracheal reconstruction, tracheal stenosis, cross-field anesthesia, gunshot injury, tracheostomy, intubation
ET, endotracheal tube; PTTS, post-tracheostomy tracheal stenosis; PITS, post intubation tracheal stenosis
Tracheal reconstruction often presents as challenging job to surgical team specially the anesthesia. Keeping patient’s lung oxygenating during the operation is very critical in the absence of cardiopulmonary bypass. Complete tracheal resection with reconstruction by using endotracheal tube oxygenation is quite troublesome as one has to put patient without ventilatory support many times for a time being during reconstruction is being done. The present case deals with the same situation and elaborates successful outcome by using cross-field anesthesia and avoiding the use of cumbersome cardio-pulmonary bypass.
A 20-year-old male presented to us with the diagnosis of post-intubation/post-tracheostomy tracheal stenosis for maxillofacial injury sustained as a result of alleged gunshot injury. In March 2012, he shot himself with a gun just below the chin to upward direction as an attempt to suicide after which, he approached to nearby hospital where he underwent maxillofacial (mandible, palate and nasal reconstruction) and neurosurgery. In intensive care unit, patient developed severe sepsis with chest infection on ventilator. After weaning, tracheostomy was done and patient was managed with regular suctioning of trachea and nasogastric feeding at home for nearly two months thereafter. The tracheostomy tube was then removed and the patient was allowed to take semi-solids and liquids. Following tracheostomy tube removal, the trachea-cutaneous fistula started healing but concurrently patient also started developing grunting sound on inspiration leading to occasional respiratory difficulty due to secretions. After fifteen days of tracheotomy tube removal, he sudden developed severe respiratory distress and was referred to the tertiary center for further management where he was put on mechanical ventilation and the tracheostomy was again performed. He was weaned off from ventilator after three days with tracheostomy tube in place and was then referred to us for further management.
The patient was thoroughly evaluated with computed tomography scan of chest (Figure 1) and video bronchoscopy (Figure 2) and found to have severe tracheal stenosis and therefore, was planned for Tracheal Resection with end-to-end anastomosis under cross-field general anesthesia. The patient was placed supine with extended neck. The procedure was started with a transverse neck incision involving tracheostomy wound. The tracheostomy tube was removed and replaced with a sterile Flexometallic endotracheal (ET) tube with ventilatory circuit by one of the assistant through which general anesthesia was continued. Peristomal dissection was carried out and trachea freed from the skin. Cervical part of the trachea was mobilized. To reach the stenosed segment of trachea, upper median sternotomy was done. The diseased stricture segment was approximately 2cms in length and about 1.5cms from the stoma. The intervening area between the tracheostomy stoma and strictured segment was unhealthy with thinned out tracheal wall. Decision was taken to resect the trachea from proximal to stoma to distal to stenosis including the intervening unhealthy segment which amounted to nearly 4.5cms of tracheal length. In order to achieve adequate length for anastomosis, laryngeal drop was performed by extending the neck and raising the flaps. Trachea was mobilized completely and the diseased segment as described was resected. Airway was established by passing the flexometallic ET tube into the distal tracheal segment. However, adequate length for tension free anastomosis was still not achieved.
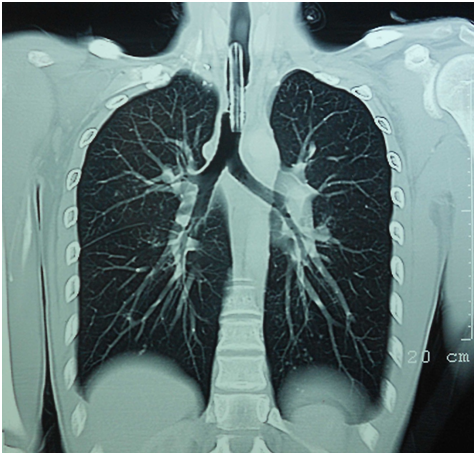
Figure 1 Coronal section of the chest computed tomography scan revealed narrowing of the tracheal lumen well above the carina with tracheostomy tube in situ.
Decision of conversion of upper median sternotomy incision into the right thoracosternotomy was then taken. To mobilize the right main bronchus up, right inferior pulmonary ligament was divided and so as the pericardial attachments of right pulmonary artery, superior pulmonary vein and inferior pulmonary vein by giving U-shaped incision of the pericardium underneath the hilum. This maneuver provided adequate length to achieve a tension free end-to-end anastomosis of trachea which was carried out by 3-0 polydiaxone interrupted sutures.
During the anastomosis, a close cooperation subsisted between the anesthetist and surgeon with intermittent ventilation of the lung alternating with temporary removal of the tube for precise placement of anastomotic sutures. Ventilation during this period was maintained with apneic oxygenation. A keen observation on end tidal carbon dioxide (ETCO2) and oxygen saturation levels helped to keep the respiratory and hemodynamic parameters in acceptable range. After posterior and lateral wall anastomosis, the nasotracheal flexometallic single lumen tube (6.5mm ID) was advanced beyond the anastomotic line under vision and then remaining anastomosis completed.
Hemostasis was secured. The pleural cavity was washed with normal saline and the sternothoracotomy was closed after placing the 28F chest tube drain at the base. Neck was also closed in layers after putting multifenestrated 10F vacuum drain. The patient was deliberately ventilated for 48hours postoperatively thereafter extubation was done but patient was unable to maintain the saturation and therefore was reintubated under bronchoscopic guidance. He was kept ventilated for another 48hours and then extubated. This time the patient tolerated extubation well. He was subsequently shifted back to the ward where on fourth postoperative day, chest tube and neck drains were removed. He was finally discharged from the hospital after 5days with normal respiratory function and healthy wound site.
The post-intubation and/or post-tracheostomy tracheal stenosis was considered rare until a prospective study of patients after intubation or tracheostomy using bronchoscopy revealed a 20% incidence of tracheal stenosis in patients who survived the initial period of ventilation.1 We have labeled the present case as post-tracheostomy tracheal stenosis (PTTS) because patients with post-intubation stenosis tend to develop web-like fibrous stenosis at the cuff site while tracheostomy patients develop stenosis due to granulation tissue around the stoma site, and frequently there is an associated cartilage fracture or malacia of the trachea wall. Also patients with tracheostomy remain intubated for longer periods, thus exposed to more trauma at the tracheal stoma site, and risk of infection. Stenosis that developed as a web around an endotracheal tube cuff is longer and more uniform than the stenosis around a tracheal stoma where granulation tissue can extent from a fissure in the anterior trachea or grow into a bulky granulomatus formation surrounding a fracture cartilage.2 Our patient fulfills most of the criteria for the diagnosis of PTTS as described above.
PTTS is an iatrogenic lesion caused by cicatricial healing of an area of transmural injury to the airway. Tracheostomy most commonly for ventilatory support can result in local ischemia or necrosis and subsequent stenosis during the phase of healing by secondary intention. Necrosis induced by pressure related loss of regional blood flow is the central injury leading to PTTS.3 The blood supply of the trachea is segmental. Blood vessels perforate the tracheal wall at each interannular space and arborise within the submucosa. The tracheal rings receive their blood supply solely from this submucosal plexus.4,5 Compression of submucosa by the cuff of an ET tube or tracheostomy tube (especially when the cuff pressure exceeds the mucosal capillary pressure i.e. 30mmHg of the trachea) can thus cause regional ischemia of the cartilaginous rings leading to ulceration and chondritis of the tracheal cartilage followed by fibrotic healing and progressive tracheal stenosis typically within 3-6weeks.3,6 Various factors (Table 1) can facilitate these circumstances.3 This etiopathogenesis explained our case also as well defined granulation tissue caused tracheal narrowing (Figure 2). The lesion is usually within 3-4cms of the cricoids cartilage i.e. the site of tracheostomy. In our case also thee lesion was 2cms below the tracheostomy opening extending for 2.5cms and ending 4cms above the carina.
|
|
|
Table 1 Factors facilitating regional ischemia in trachea
Grillo said that any patient who develops symptoms of airway obstruction, who has been intubated and/or ventilated in the recent past, must be considered to have an organic lesion until proved otherwise.7 A patient with such a history, who presents with wheezing, stridor or exertional dyspnea is much more likely to have a post intubation tracheal stenosis PITS.3 The airway cross-sectional area must decrease to less than 30% of normal for the patient to be symptomatic at least. A sedentary post-intubation patient with wheezing or stridor from PITS lesion will thus have an airway diameter 5 mm or less and is at risk for acute obstruction with minimal amount of secretion.3 The same picture had shown by our patient who had also presented with grunting respiration, stridor and respiratory failure due to accumulation of secretion after first post intubation period that finally lend up into the second emergency tracheostomy and mechanical ventilation. On chest-X-ray, the tracheal air column, however, is frequently overlooked by radiologists and surgeon alike and deserves careful inspection in a symptomatic post intubation and/or post tracheostomy patients. The precise nature, length, and severity of the PTTS or PITS lesion(s) however are ideally determined by bronchoscopic evaluation.
The optimal treatment of PITS or PTTS is one stage, primary resection and reconstruction.8,9 Circumferential dissection of the trachea is confined to the region of the stenosis and no more than 1-1.5cms of normal trachea proximal and distal to the lesion. Mobilization of the airway proximal and distal to the stenosis is done solely by dissection in the anterior midline. This approach preserved the segmental, lateral blood supply of the proximal and distal airway segments.
Nearly all PITS/PTTS lesions can be approached through a long collar incision or a collar incision in conjunction with a partial upper sternotomy. We had also approached in the same fashion to start with but due to insufficient length of tracheal segments for tension free anastomosis we had converted upper sternotomy to sternothoracotomy to mobilize the right main bronchus. Most commonly, the length of resection required for these lesions is less than 3.5cms which is achieved by cervical flexion performed by anesthesiologist. However, suprahyoid laryngeal release, described by Montgomeray adds 1.0-1.5cms length while minimizing the difficulties in swallowing that attended earlier techniques for release.10 If laryngeal release is also proved insufficient than mobilization of the main bronchus by first freeing the hilum of the right lung and dividing the inferior pulmonary ligament, second freeing of pulmonary vessels from pericardial attachments permits additional 3cms and 0.9cms length to the distal trachea.11 We had to perform the same maneuver owing to the large gap between the tracheal segments.
It is well known that the ability to provide adequate ventilation throughout the perioperative period is a major predictor for better outcome during tracheal surgery. Different anesthetic techniques have been described for tracheal resection, spontaneous ventilation throughout the procedure using total intravenous anesthesia, low frequency jet ventilation, high frequency jet ventilation, distal tracheal intubation, intermittent positive pressure ventilation and cardiopulmonary bypass.
Conclusively, the anesthetic maneuvers and surgical approach differed in relation with the site of the tracheal lesions, the degree of the obstruction and the emergency of the surgical intervention. Ventilatory support during anesthesia involved special equipments adapted to the particular techniques used in this type of surgery. Cross-field intubation of trachea or a main stem bronchus and high frequency jet ventilation have been frequently used. Perfect coordination of the anesthetic technique with every surgical step is mandatory and for good long term results special anesthetic equipment and thorough preoperative anesthetic and surgical assessment of the strategy is needed.
None.
Author declares there are no conflicts of interest.
None.

©2017 Srivastava, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.