Journal of
eISSN: 2373-6437


Mini Review Volume 5 Issue 1
Consultant Intensive Care Medicine at Private practice clinic, Iraq
Correspondence: Fadhil Zwer, Consultant Intensive Care Medicine at Private practice clinic, Iraq
Received: April 22, 2016 | Published: June 1, 2016
Citation: Zwer F (2016) Definition, Incidence and Evolution of Sepsis & Septic Shock. J Anesth Crit Care Open Access 5(1): 00171. DOI: 10.15406/jaccoa.2016.05.00171
Sepsis is not just a disease of the intensive care unit, and approximately half of cases are diagnosed in the emergency department and on wards throughout the hospital. Given that sepsis accounts for about 2% of all hospital admissions, it is inevitable that all medical personnel will encounter a septic patient. It is of the utmost importance that practitioners are able to recognize this clinical entity promptly. The first few hours of resuscitation of the septic patient are known as the “Golden Hour” of sepsis because early recognition and treatment of sepsis leads to improved survival outcomes. Although the details of resuscitating the septic patient may be more limited to the ICU, first line physicians have essential roles in the rapid recognition of sepsis and the initiation of treatment.
Definitions
Sepsis historically has been a condition that is difficult to identify and diagnose. As far back as 100 BC, Marcus Terentius Varro, the ancient Roman scholar and writer (116 BC–27 BC), was speculated as noting that [small creatures, invisible to the eye, fill the atmosphere, and breathed through the nose cause dangerous diseases]. Perhaps the most prescient description of sepsis was by the historian, philosopher, humanist and Renaissance author Niccolo Machiavelli (1469–1527), as reported in his treatise, The Prince, in 1513. Early in the book, he very clearly stated that, [hectic fever, at its inception, is difficult to recognize but easy to treat; left unattended it becomes easy to recognize and difficult to treat]. Although hectic fever is not the name by which we know sepsis now, the description of a disease that is difficult to recognize in its early stages, at a time when the condition may be amenable to treatment, and more difficult to treat in its later more obvious stages is a clear description of the more severe forms of sepsis.
In an attempt to better clinically understand sepsis, in the past century, a variety of definitions have been developed. Among the earliest concepts was to consider sepsis as a systemic host response to an infection. In fact, it was classically described by the eminent American physician William Osler (1849–1919) in his seminal observation that the patient appears to die from the body’s response to an infection rather than from the infection itself. Closer to the modern era, in 1972 this concept was reinforced in a medical review, noting that “it is our response that makes the disease”.1 The general concept has long been considered a form of poisoning, often considered as blood poisoning, but more practically representing the presence of pathogenic organisms or their toxins in the blood or tissues. It was the failure of these medical definitions, and so many attempts at developing diagnostic tools and assays to identify sepsis, that led to a consensus conference focusing on a way to clinically define sepsis. In 1992, the American College of Chest Physicians (ACCP) and the Society of Critical Care Medicine (SCCM) jointly published the consensus definitions of sepsis (Table 1). These are among the most frequently cited definitions in Critical care and they have become second nature to many critical care physicians (intensivists) and other intensive care providers throughout the world. Their novel description of the systemic inflammatory response syndrome criteria and specific definitions for sepsis, severe sepsis, septic shock and multiple organ dysfunction syndromes were all critical developments in the field of sepsis (Figure 1). Since these consensus definitions had limitations in clinical use, they were revisited in 2001. Although there were many limitations recognized of the current definitions, there was no superior alternative identified. There was significant consideration to expanding the foundational systemic inflammatory response syndrome criteria to include other parameters that may be associated with sepsis.
ACCP/SCCM condition |
Defining criteria |
SIRS |
Core body temperature >38°C or <36°C, HR ≥90 bpm, Respirations ≥20/min (or PaCO2 <32 mmHg), WBC ≥12,000/μl or ≤4000/μl or >10% immature forms |
Sepsis |
At least two SIRS criteria caused by known or suspected infection |
Severe sepsis |
Sepsis with acute organ dysfunction (including hypoperfusion and hypotension) caused by sepsis |
Septic shock |
Sepsis with persistent or refractory hypotension or tissue hypoperfusion despite adequate fluid resuscitation |
MODS |
The presence of organ dysfunction in an acutely ill patient such that homeostasis cannot be maintained without intervention |
Table 1 Defining criteria of ACCP/SCCM named conditions2
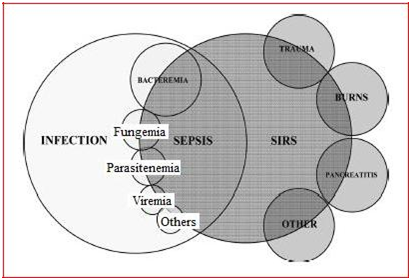
Figure 1 Relationship between systemic inflammatory response and infection, where the overlap indicates sepsis.2
However, these represented a broadening of the potential diagnostic criteria that would, if anything, make the sepsis definition less specific than it was previously. In addition, some of the criteria overlapped with the definitions developed for identifying organ dysfunction, which is a critical component of distinguishing severe sepsis and septic shock. Perhaps the most important result from the 2001 Consensus Conference was the proposal for a Predisposition, Infection, Response and Organ dysfunction (PIRO) system for staging sepsis. The concept of PIRO was analogous to staging cancer or other medical conditions, and it appears that these criteria do allow for differentiating groups of patients with sepsis.2
Sepsis is the presence of infection in the setting of a systemic inflammatory process, more formally termed systemic inflammatory response syndrome (SIRS). As its name implies, SIRS occurs in a wide range of inflammatory states in addition to infection, such as burns and surgery (Table 2). The diagnosis of SIRS requires alterations in two of the following four parameters, including temperature, heart rate, respiratory rate and white blood cell count (Table 3).3 When SIRS is the result of a confirmed infectious etiology, the clinical scenario is termed sepsis. This is distinct from the confusing term “septicemia” which is used without a clear definition and probably has little place in academic circles.
Pacreatitis. |
Ischemia. |
Multiple trauma. |
Hemorrhagic shock. |
Immune-induced organ injury. |
Exogenous inflammatory mediators (TNFα). |
Systemic infection. |
Table 2 Causes of systemic inflammatory response syndrome1
Term |
Definition |
Infection |
Microbial phenomenon characterized by an inflammatory response to the presence of microorganisms or the invasion of normally sterile host tissue by those organisms. |
Bacteremia |
The presence of viable bacteria in the blood. |
SIRS |
Two or more of the following criteria present: |
1) Temperature of > 38oC OR < 36oC. |
|
2) Heart rate > 90 beats per minute.* |
|
3) Respiratory Rate > 20 breaths per minute OR a PaCO2< 32 mm Hg OR mechanically ventilated. |
|
4) Leukocyte count > 12,000/μL OR < 4,000/μL OR > 10% immature bands. |
|
Sepsis |
SIRS in the presence or presumed presence of an infection. |
Severe sepsis |
Sepsis plus organ hypoperfusion AND/OR organ dysfunction. |
Septic shock |
Sepsis with either: |
1) Refractory hypotension as defined by: |
|
a) Systolic blood pressure < 90 mm Hg OR a mean arterial pressure of < 65 mm Hg OR a 40 mm Hg drop in systolic blood pressure below patient’s baseline. |
|
b) Pressure unresponsive to a fluid challenge of 20-40 ml/kg. |
|
2) Vasopressor dependency after adequate fluid resuscitation. |
Table 3 Definitions of sepsis and related terms1
*Criteria fails if the patient is rate controlled (such as with beta-blockers or calcium-channel blockers) or the heart is paced
As organ hypoperfusion and organ dysfunction develop, severe sepsis ensues. This may manifest clinically as altered mental status or oliguria, with accompanying laboratory results like lactic acidosis (Table 4). Septic shock occurs when there is a drop in systolic or mean arterial blood pressure despite adequate volume resuscitation. Shock, in general, is defined as an abnormality of the circulatory system that results in inadequate organ perfusion and tissue oxygenation. There are several causes of shock in addition to sepsis, including hypovolemia and cardiac dysfunction. Though it is clinically relevant to differentiate between the different causes of shock, in reality they are essentially stages along a continuum. While SIRS may be self-limiting in the setting of sepsis, it may progress to concomitant organ hypoperfusion and dysfunction. When cardiovascular collapse occurs, septic shock results from hypotension.3
Organ hypoperfusion |
Organ dysfunction |
Elevated blood lactate level. |
Hematologic: disseminated intravascular coagulation, thrombocytosis. |
Oliguria. |
Respiratory: acute respiratory distress syndrome. |
Poor peripheral circulation. |
Renal: acute renal failure. |
Altered mental state. |
Gastrointestinal system: hepatic dysfunction. |
CNS: delirium. |
Table 4 Clinical and laboratory manifestations of severe sepsis1
Changes in incidence
The clinical consensus definition of sepsis has allowed for a number of studies of epidemiology to be conducted. At present, there have been studies in most developed and in many developing countries using this clinical definition. In general, sepsis occurs in approximately 2% of all hospitalizations in developed countries.
Sepsis may occur in between 6% and 30% of all intensive care unit patients, with substantial variation due to the heterogeneity between ICUs. For example, sepsis may occur in a very high proportion of medical or trauma ICU patients in a large urban hospital but may comprise a relatively small proportion of ICU patients in a community cardiac or surgical ICU. In general, more than 50% of severe sepsis patients will require intensive care services. There has been less attention on the incidence of sepsis than there is on the incidence of severe sepsis and septic shock. This is perhaps appropriate given that sepsis may be present in nearly all patients requiring hospitalization with an infection, while severe sepsis is present in between half and three-quarters of critically ill patients.4 Furthermore, it is the patients with organ dysfunction and high severity of acute illness that consume much of the resources and are at high risk for complications and death. In most developed countries, the incidence of severe sepsis has been identified as between 50 and 100 cases per 100,000 people in the population. In general, the incidence of sepsis is three to four-times higher, reflecting the relative percentage of patients who develop organ dysfunction and thus meet more severe definitions (severe sepsis or septic shock). In the past decade it have been realized that there have been significant longitudinal changes in the incidence of sepsis, most obviously in the USA. A two-decade study of US hospitalizations identified an increase in the incidence of sepsis among hospitalized patients by 8.7% per year. At present, it is estimated that there are more than 1,000,000 cases of sepsis among hospitalized patients each year in the USA. Numerous reports have shown the incidence of sepsis and severe sepsis increasing in excess of the growth of the population. Similar reports exist from the UK, Australia and from Croatia. It is important to mention that these numbers of incidence are mostly higher in developing countries.
The incidences of sepsis, severe sepsis and septic shock are less well-described in the developing world. There are more data available on the incidence of infectious diseases, which remains a constant battle for which there are many high incidence conditions. As infectious diseases are inevitably the cause of sepsis, sepsis presumably is of similar or even greater importance in these areas of the world than in the most developed nations. Sepsis is more frequent in younger individuals in the developing world and the responsible organisms are more likely to be Gram-negative enteric pathogens and atypical pathogens such as malaria. It should also be noted that patients dying of infectious diseases inevitably die of sepsis and sepsis -related organ dysfunction. As stated earlier, it is not the infection that kills people but rather it is the host immune response attempting to fight the infection that ultimately may cause the fatal outcome. With that in mind, it is apparent that it inevitably underestimates the incidence of the more severe forms of sepsis in areas where more attention is given to infectious diseases and to their causes and complications.
Nevertheless, the incidence of sepsis is affected by a variety of patient-specific factors. It have been long recognized that age is an important component of someone’s risk for developing sepsis, as are a variety of comorbid medical conditions. Perhaps most obvious are conditions like HIV, cancer and diabetes, each of which may alter the immune system. These conditions result in a significantly elevated risk for developing sepsis, and may also increase the risk of nosocomial sepsis given these individuals’ frequent interactions with healthcare systems. More recently it has been recognized that race, ethnicity and gender may also contribute to the differential risk for developing sepsis. In general, males have a higher risk for developing sepsis than females, regardless of age. The mechanisms behind differential incidence based on race and ethnicity are less clear, but in general non-Caucasian races are at higher risk for developing sepsis compared with Caucasians.
Evolution of pathogens
The causative organisms for sepsis have evolved over many years. Originally sepsis was described, and strongly considered to be, a disease specifically related to Gram-negative bacteria. This is because sepsis was considered to be a response to endotoxin - a molecule that was thought to be relatively specific for Gram-negative bacteria. In fact, some of the original studies of sepsis bore out that Gram-negative bacteria were among the most common causes of sepsis. This resulted in a number of trials that focused on Gram-negative therapies, and even highly specific therapies for endotoxin, which were felt to be potentially useful treatments for sepsis. However, it is now recognize that sepsis may occur from any bacteria, as well as from fungal and viral organisms. More recent epidemiology studies reveal that Gram-positive bacteria have become the most common cause of sepsis in the past 27 years. According to the most recent estimates in sepsis, there are approximately 200,000 cases of Gram-positive sepsis each year, compared with approximately 150,000 cases of Gram-negative sepsis. Anyhow, while bacterial causes of sepsis have increased with the general increases in incidence, fungal causes of sepsis have grown at an even more rapid pace. This may represent a general increase in nosocomial cases of sepsis, or it may reflect the effective treatment of bacterial infections, thus promoting fungal infections to a more leading role. While there has been an overall increase in the number of fungal nosocomial infections, it have been also observed shifts away from the most common Candida albicans organism to the more recalcitrant torulopsis, glabrata and krusei subspecies.
Sepsis tends to occur from specific and consistent sources. Respiratory infections are invariably the most common cause of sepsis, severe sepsis and septic shock. Overall, respiratory infections account for approximately half of all cases of sepsis. The next most common causes are genitourinary and abdominal sources of infection with primary bacteremia and unknown sources being the next most common causes. The occurrence of acute organ dysfunction (i.e. severe sepsis) is related to the source of infection, as in patients with respiratory infections who are at higher risk for developing respiratory organ dysfunction.
Regardless of the era and the organisms, the treatment of infection is the cornerstone of antisepsis therapy. There are two particular components of antimicrobial therapy that are important. The first is early antimicrobial therapy, with initiation of antibiotics in an appropriate time interval depending on the location of the patient. There are particular data from patients with pneumonia, and from those with septic shock, that show that delays in antimicrobial therapy lead to a significantly increased risk of dying. Especially critical for septic shock, the risk of dying increases by approximately 10% for every hour of delay in receiving antibiotics. The other important component of antimicrobial therapy is appropriateness of the antimicrobial regimen. It may be intuitive that coverage of the appropriate organisms is critical, as failure to cover the appropriate organisms is synonymous with delays of antimicrobial therapy. A variety of studies of infected and septic patients show that inappropriate antimicrobial therapy is a consistent predictor of poor outcomes. From a clinical perspective this means that the antimicrobial therapy must almost always be empiric. The choice of antibiotics, and the timing of their administration, cannot wait for isolation and identification of the causative organism and determination of the organism’s sensitivity to various antibiotics. These principles underlie the observation that combination antimicrobial therapy may be superior to monotherapy. In addition, in certain circumstances antibiotic therapy alone is not sufficient to treat the infection causing sepsis, in which case source control is also necessary to eradicate the infection.2
None.
Author declare that there is no conflict of interest.
None.

©2016 Zwer. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.