International Journal of
eISSN: 2574-9889


Research Article Volume 9 Issue 6
1Department of Pediatrics, Ruby Hall Clinic, India
2Department of Pediatrics, Zydus Medical College & Hospital, India
Correspondence: Kanchankumar Bhagyawant, Department of Paediatrics, Zydus Medical College & Hospital, Dahod, Gujrat, India
Received: December 15, 2023 | Published: December 29, 2023
Citation: Vineela P, Bhagyawant K, Venkatramani V. Prevalence of iron deficiency anaemia in congenital heart disease in children. Pregnancy & Child Birth. 2023;9(6):183-187. DOI: 10.15406/ipcb.2023.09.00300
Background: Congenital heart disease (CHD), out of all congenital anomalies, is the leading condition of mortality and morbidity in children under 5 years of age. Iron deficiency anaemia (IDA) has been clearly shown to be an important risk factor that increases morbidity and mortality in such patients. The present study is thus conducted to find out the prevalence of iron deficiency anaemia in children less than 15 years with congenital heart disease at a tertiary care centre and compare them with cases without CHD.
Methods: Prospective study over a period of 2 years, included 60 cases of children below 15 years of age with echocardiographicaly confirmed CHD, investigated by serum ferritin to diagnosed IDA using cut off 12ng/ml. These cases compared with similar age controls.
Results: 51cases (82%) were of acyanotic heart disease and 18% were of cyanotic heart disease. Iron deficiency or storage depletion was seen in 90% cases as compared to 75% controls. Iron deficiency anaemia was seen in 55% cases as compared to 30% controls, the difference was statistically significant.
Conclusions: Present study observed higher prevalence of IDA among cases with CHD as compared to general population of children. The prevalence was found to be more in cases with cyanotic heart disease as compared to cases with acyanotic heart disease. We thus conclude that routine screening for iron deficiency should be done for these children and those found to be deficient should be treated.
Keywords: congenital heart disease, iron deficiency anaemia
Gross anatomical abnormalities of the heart or intrathoracic great vessels that are functionally significant are referred to as congenital heart disease (CHD). Between 4 to 50 per 1000 live births, congenital cardiac disease affects around 1% of the general population.1 CHD was found to affect 2.25–5.2 out of every 1000 children in India. Congenital cardiac disease is the most common cause of death and morbidity among congenital abnormalities in children less than five.2
In 2020, the prevalence of Iron deficiency anaemia (IDA) in Indian children is reported as 56%. The most frequent cause is a nutritional iron deficiency, with school-age children being the most susceptible.3 Adults with iron deficiency anaemia perform less physically, while children and adolescents are particularly negatively impacted in terms of their psycho-motor development.4,5 Significantly, adolescent behavioural and social issues are linked to iron deficiency, with or without anaemia, in infancy.6 Notably, it has been amply demonstrated that IDA is a significant risk factor that raises morbidity and mortality in individuals with CHD.7
The right-to-left shunt causes chronic arterial desaturation in children with CHD, which raises the erythrocyte count and causes high blood viscosity. Moreover, red blood cells are less permeable in patients with cyanotic CHD who are anaemic, particularly in those who have hypochromic anaemia from an iron deficit. The elevated incidence of embolism and other cardiovascular mishaps is partly explained by this phenomenon.8 A normal haemoglobin (Hb) in children with cyanotic congestive heart failure (CHD) may indicate that the patients are relatively anaemic, which could have a detrimental impact on morbidity and mortality.9,10 It is highly advised that individuals with acyanotic heart disease who develop heart failure have early detection and proper treatment for their anaemia. Furthermore, it has become more important to prevent thromboembolic episodes and cyanotic spells in kids with cyanotic CHD.10
Nowadays, cyanotic CHD are treated in industrialised nations with the best possible nutritional support. However, a sizable portion of children with complicated congenital heart disease (CHD) in underdeveloped nations like India do not receive surgery. Furthermore, the high rate of malnutrition remains a significant public health concern.11 We would anticipate that this susceptible group has a higher incidence of IDA. Everyday practice often overlooks or underdiagnoses anaemia in children with congenital heart disease (CHD), particularly in cyanotic youngsters who exhibit elevated haematocrit values as a result of persistent hypoxia.12,13
The present study is thus conducted to find out the prevalence of iron deficiency anaemia in children less than 15 years with congenital heart disease at a tertiary care centre and compare them with cases without congenital heart disease.
Study area
Department of Paediatrics of a tertiary care centre
Study population
Children below 15 years with confirmed diagnosis of congenital heart disease, coming at our hospital.
Study design
Prospective Study
Sample Size
Sample size was calculated using formulae:
n= (Zα/2 + Zβ) x PQ * 2 /d2
Where;
n- 55
So, by rounding off, we will be taking 60 subjects in each group i.e. children with CHD and children without CHD.
Study duration
2 years
Inclusion criteria
Age < 15 years
Both gender
Diagnosed cases of CHD on Echocardiogram
Exclusion criteria
Cases with previous corrective surgery
Taking Iron Supplementation
Patient with anemia due to thalassemia or other unknown mechanisms.
Statistical analysis
A prepared study proforma contained all of the data. The frequency and percentage representations of the qualitative data were used. For every 2 X 2 table, the Fisher's exact test and the Chi-Square test were used to evaluate the association between the qualitative variables. Mean ± SD was used to represent quantitative data. When analyzing quantitative data comparing the two groups, the Mann-Whitney test was used if the data failed the "Normality test," and the unpaired t-test was used if the data passed. A p-value of less than 0.05 was considered significant. When it was thought necessary, the results were displayed graphically. For most analyses, SPSS Version 21.0 was utilized, and Microsoft Excel 2010 was used for graphical depiction.
|
Group |
N |
% |
|
Cases |
60 |
50.00% |
|
Controls |
60 |
50.00% |
|
Total |
120 |
100.00% |
Table 1 Distribution of number of cases as per study groups
Present study included 60 cases of congenital heart disease and 60 controls without congenital heart disease.
|
Cases of CHD |
|
N |
% |
|
Acyanotic (n-51) |
ASD |
20 |
40.00% |
|
VSD |
25 |
50.00% |
|
|
PDA |
6 |
12.00% |
|
|
Cyanotic (n-9) |
TOF |
8 |
16.00% |
|
|
TGV |
1 |
2.00% |
Table 2 Distribution of cases as per type of congenital heart disease
51(82%) cases were of acyanotic CHD and 9 (18%) were of cyanotic CHD. Among acyanotic heart disease, 50% were VSD cases and 40% were ASD. Tetralogy of fallot (16%) was the most common cyanotic CHD observed in present study. 70% of the studied cases were between 1 to 5 year age group, with 26.7% under 1 year.
|
Gender |
Group |
|
Total |
|
Case |
Controls |
||
|
Female |
32 |
31 |
63 |
|
53.30% |
51.70% |
52.50% |
|
|
Male |
28 |
29 |
57 |
|
46.70% |
48.30% |
47.50% |
|
|
Total |
60 |
60 |
120 |
|
100.00% |
100.00% |
100.00% |
|
|
p- value - 1.0 |
|
|
|
Table 3 Distribution of study groups as per gender
Overall 53.3% cases of CHD were females and 46.7% were males.
Evaluation of anthropometric indices showed that among CHD cases, 26.7% were underweight, 21.7% were stunted and 15% were wasted as compared to 15%, 10% and 5% controls. Low mid arm circumference was seen in 26.7% cases and 13.3% controls.
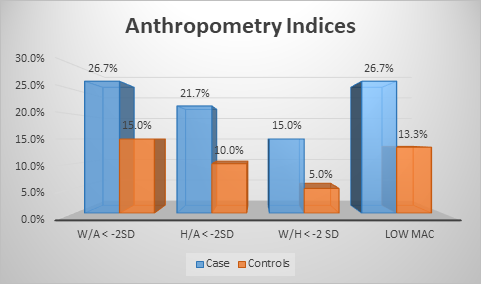
Figure 2 Distribution of study groups as per anthropometry indices.
Iron deficiency anaemia was seen in 55% cases as compared to 30% controls, the difference was statistically significant (p<0.01).
|
Variables |
Group |
N |
Mean |
SD |
p- value |
|
Hb (gm%) |
Cases |
60 |
12.76 |
2.02 |
0.69 |
|
Controls |
60 |
13.12 |
1.22 |
||
|
S. Ferritin (ng/ml) |
Cases |
60 |
21.63 |
26.32 |
<0.01 |
|
|
Controls |
60 |
32.38 |
34.26 |
|
Table 4 Mean comparison of haemoglobin and serum ferritin levels as per study groups
Mean haemoglobin levels (12.76 vs. 13.12 gm %) were comparable between cases and controls while serum ferritin levels were significantly less in cases (21.63 vs. 32.38; p<0.01 ng/ ml).
|
Variables |
Type of CHD |
N |
Mean |
SD |
p- value |
|
Hb (gm %) |
Cyanotic |
9 |
14.66 |
3.31 |
0.09 |
|
Acyanotic |
51 |
12.25 |
1.51 |
||
|
S. Ferritin (ng/ml) |
Cyanotic |
9 |
16.46 |
23.83 |
<0.01 |
|
|
Acyanotic |
51 |
24.82 |
26.95 |
|
Table 5 Mean comparison of haemoglobin and serum ferritin levels as per type of CHD
Mean haemoglobin levels in cyanotic and acyanotic heart disease cases was 14.66 gm% and 12.25 gm% (p-0.09). Mean serum ferritin levels were significantly less in cyanotic cases (16.46 vs. 24.82;p<0.01 ng/ ml)
Iron deficiency or storage depletion was seen in 90% cases as compared to 75% controls (p<0.01).
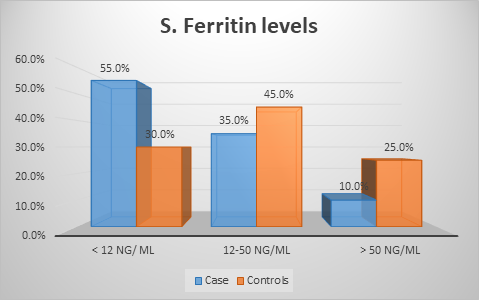
Figure 3 Distribution of study groups as per serum ferritin levels.
Iron deficiency was seen in 51% cases of acyanotic CHD as compared to 77.8% in cyanotic CHD (p-0.16).
|
Group |
IDA at baseline |
IDA at follow up |
% |
|
Cases |
25 |
2 |
3.30% |
|
Controls |
14 |
0 |
0.00% |
Table 6 Prevalence of iron deficiency anaemia after follow up
All cases of IDA were managed as per standard hospital protocol. On follow up examination, 2 cases (3.3%) had IDA as compared to none in control group.
The purpose of this study was to determine the prevalence of iron deficiency anaemia in children with congenital heart disease under the age of 15 in a tertiary care facility and compare them with cases without congenital heart disease. Study included 60 cases of congenital heart disease and 60 controls without congenital heart disease.
Type of congenital heart disease
Among 60 cases of CHD, 51 (82%) were of acyanotic heart disease and 18% were of cyanotic heart disease. Among acyanotic heart disease, 50% were VSD cases and 40% were ASD cases. Tetralogy of fallot (16%) was the most common cyanotic CHD observed in present study.
According to Singh PK et al.'s study, ventricular septal defect (50.00%) was the most common type of CHD. VSD was observed in 43.6% of the cases in15 's study, but isolated ASD and PDA were observed in 28.2% and 17.9% of the cases, respectively. In a related study, Pongiglione G et al.,16 found that coarctation of the aorta (14.3 %) and ventricular septal defect (23.1 %) was the two most common heart abnormalities. According to Rabiya N et al.,17 35% of patients had a ventricular septal defect and acyanotic CHD was more prevalent (81.3%). 13.7% of patients with cyanotic CHD (18.7%) had tetralogy of fallot.
Demography
Mean age of the study cases was 2.4 years with most of them were between age group of 1 to 5 years (70%) while 26.7% were below 1 year. Overall 53.3% cases of CHD were females and 46.7% were males. No difference was observed between study groups in terms of age and gender (p>0.05). Binh TQ et al.,18 in their study observed majority of cases between 1-5 years with mean age of 2.9 years. Equal gender distribution was noted in the study. Ossei I et al.,19 observed mean age as 2.6 years with 55% females to 45% males. Rabiya N et al.,17 in their study observed mean age of 3.9 years with 49% males to 51% females.
Congenital heart disease & malnutrition
In present study, evaluation of anthropometric indices showed that among CHD cases, 26.7% were underweight, 21.7% were stunted and 15% were wasted as compared to 15%, 10% and 5% controls. Low mid arm circumference was seen in 26.7% cases and 13.3% controls.
In their investigation, Mir AB et al.,20 found that the prevalence of malnutrition overall was 72.5% in CHD patients and 22.5% in controls. In 68.9% of instances, severe malnutrition was found to be present. When comparing the sick group to the control group, all anthropometric parameters that serve as indicators of nutritional status showed a substantial decrease. In their study, Rabiya N et al.,17 found that among CHD patients, 71% were underweight, 49% were stunted, and 82% were wasting cases. The greater frequency may have resulted from the study's location in rural India, where more than half of the population under five suffers from malnutrition.21
Prevalence of iron deficiency anaemia in CHD
Inadequate intra-cardiac communication often results in low blood oxygen saturation in CHD patients. In the majority of these cases, a relative iron shortage was found. An iron-deficiency anaemia-related increase in tissue hypoxia is one of the main effects of cyanosis. To prevent tissue anoxia, these patients' low oxygen saturation levels in their blood lead to an unusually high increase in haemoglobin concentrations as a compensatory measure. Hence, diagnosis of iron deficiency anaemia in these cases should be made on the basis of serum ferritin levels. A threshold of 12 ng/mL was used in the current investigation to diagnose IDA and level less than 50ng/ml to diagnose iron storage depletion.
On analysis, we observed that mean haemoglobin levels (12.76 vs. 13.12 gm %) were comparable between cases and controls while serum ferritin levels were significantly less in cases (21.63 vs. 32.38; p<0.01 ng/ ml). Iron deficiency or storage depletion was seen in 90% cases as compared to 75% controls (p<0.01). Iron deficiency anaemia was seen in 55% cases as compared to 30% controls, the difference was statistically significant (p<0.01).
A related study by Ossei I et al.,19 found that 47% of CHD cases had absolute iron deficit and 72.7% of cases had relative iron shortage. In their investigation, Mir AB et al.,20 found that 47.5% of the CHD population had iron deficiency anaemia (IDA). In contrast to the general population, patients with cyanotic cardiac disease had their iron deficient anaemia evaluated by Sumeet Soni et al.22 In cases of cyanotic heart disease, the mean haemoglobin was 13.39 gm/dl with a 2.38 SD. The mean haemoglobin level in the control group was 9.57 gm/dl with a 1.29 SD.
Prevalence of iron deficiency anaemia in cyanotic and Acynotic heart disease
Erythropoietin levels rise and secondary erythrocytosis occurs when CHD is associated with to hypoxia. The tissue oxygenation deficit may be corrected by the increased erythrocyte mass, which would also create a new equilibrium at higher haematocrit levels. Thus, without corresponding decrease in Hb and RBC, the increased demand on iron stores frequently causes iron insufficiency in infants with cyanotic congenital heart disease. Similar results were observed in present study where mean haemoglobin levels in cyanotic disease was higher as compared to acyanotic heart disease i.e. 14.66 gm% and 12.25 gm% (p-0.09). However, mean serum ferritin levels were significantly less in cyanotic CHD cases (16.46 vs 24.82; p<0.01 ng/ ml). Iron deficiency as defined by s. ferritin< 12 ng/ml was seen in 51% cases of acyanotic CHD as compared to 77.8% in cyanotic CHD (p-0.16).
100 patients with various forms of cyanotic and acyanotic congestive heart failure had their pre-operative charts examined by H Amoozgar et al.12 The mean Hb and MCV of the cyanotic patients were 15.97 ± 17.19 and 73.76 ± 27.26, respectively, while the mean Hb of the acyanotic group was 13.56 ± 9.44 and the MCV was 80.4 ± 12.36... Mir AB et al.,20 observed that haemoglobin and haematocrit levels, RBC count were paradoxically higher in the cyanotic CHD as compared to the controls. However in both the studies, through the iron studies, it was revealed that iron stores were depleted in this group, similar to present study. Sumeet Soni et al.,22 in their study observed IDA in 56.6% of the cases with cyanotic heart disease.
Thus to summarize, present study observed that burden of malnutrition and iron deficiency anaemia among CHD cases was very high. Every second children of CHD is suffering from iron deficiency and four out of five children had iron storage depletion. The prevalence was found to be more in cases with cyanotic heart disease as compared to cases with acyanotic heart disease. We thus conclude that routine screening for iron deficiency should be done for these children and those found to be deficient should be treated.
Present study observed higher prevalence of IDA among cases with CHD as compared to general population of children. Every second children of CHD is suffering from iron deficiency and four out of five children had iron storage depletion. The prevalence was found to be more in cases with cyanotic heart disease as compared to cases with acyanotic heart disease. We also observed one of the most prevalent issues in children with congenital heart disease is malnutrition. We thus conclude that routine screening for iron deficiency should be done for these children and those found to be deficient should be treated.
None.
The Author declared that there is no conflict of interest.

©2023 Vineela, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.