International Journal of
eISSN: 2574-9889


Research Article Volume 3 Issue 4
Department of Obstetrics and Gynecology, Faculty of Medicine, Tanta University, Egypt
Correspondence: Ayman Shehata Aboelazm Dawood, Department of Obstetrics and Gynecology, Faculty of Medicine, Tanta University, Tanta, Egypt
Received: November 16, 2017 | Published: December 27, 2017
Citation: El-Halwagy AS, Dawood AS. Second trimester pregnancy termination in previous cesarean section patients with unfavorable cervix: a randomized controlled clinical trial comparing 3 different methods. Int J Pregn & Chi Birth. 2017;3(4):289-293. DOI: 10.15406/ipcb.2017.03.00070
Background: Vaginal termination of second trimester pregnancy is usually performed when complications occur. In this study, we com-pared 3methods of vaginal termination regarding time to effacement and delivery in addition to delivery success rate.
Methods: The study was carried at Tanta University starting from April 2016 for a duration of 6 months. In all, 90 patients with previous cesarean section having different indications for second trimester vaginal termination of pregnancy were enrolled in the study. We compared 3methods: vaginal dinoprostone (PGE2), intracervical Foley’s catheter, and intracervical injection of hyaluronidase enzyme (Hyal). The 90 patients were randomly distributed into 3 groups, 30 patients in each group. Time to effacement, time to delivery, and success rate of induc-tion were the outcome measures of the study.
Results: Time to effacement was 9.2±3.3hours in the Hyal group, 10.3±1.5hours in the PGE2 group, and 15.4±4.5hours in the Foley’s catheter group (P< .001). Time to delivery was 14.2±3.5hours in the PGE2 group, followed by the Hyal group (15.7±1.7hours) and the Foleys’ group (20.12±4.8hours) (P<.001). Success rate was 96.7% in the Hyal group, 90.0% in the PGE2 group, and 80.0% in the Foley’s group.
Conclusion: The “Hyal” technique has the shortest time of effacement and better rate of success than the other 2 methods, but it does not give the shortest time to delivery.
Keywords: cesarean section, induction of labor, intrauterine fetal death, termination of pregnancy, time to effacement, vaginal termination
Induction of labor (IOL) in previous cesarean section (SC) patients with unripe cervix represents a major challenge for obstetricians to avoid fetal and maternal complications which may be catastrophic. Termination of pregnancy (TOP) in sec-ond trimester by IOL is usually performed when complications occur, such as severe preeclampsia and ruptured membranes. The other common medical indications include uncontrolled hypertension, impaired renal functions, and malignancy any-where requiring immediate management.1
Women with previous CS had an increased risk of uterine rupture than patients with unscarred uterus, so IOL in these patients should be done after thorough and detailed counseling with both patient and their relatives.2
Many studies evaluated different methods of labor induc-tion when the cervix is unfavorable, including misoprostol, transcervical insertion of Foley’s catheter, double-balloon cath-eter, laminaria tents, and oxytocin intravenous drip. These methods were classified roughly into either pharmacological or mechanical methods.3,4
Although misoprostol (PGE1) is widely used for labor induction, it has a high incidence of uterine hyperstimulation and subsequent rupture uterus which is a nightmare for mis-oprostol users, especially in women with CS, so misoprostol is not recommended in those patients.5,6 On the contrary, vaginal dinoprostone is safer and had less uterine hyperstimulation and less fetal distress, but is less effective than misoprostol and somewhat expensive.7
Foley’s catheter is another procedure used for mechanical IOL, which involves transcervical insertion of Foley’s catheter. Foley’s catheter induces labor by both mechanical dilatation and stimulating endogenous release of prostaglandins.8,9
Another new method for labor induction was tested at a low scale of populations, which is the intracervical injection of hyaluronidase. Hyaluronidase is an enzyme that increases hydrolysis of hyaluronic acid, decreases the tensile strength of cervical collagen, and hence promotes cervical softening and effacement.10
Mechanical methods apply pressure on the internal cervical os, stretch the lower uterine segment, and increase local pro-duction of prostaglandin. There is a lack of compelling evi-dence suggesting increased risk of uterine rupture because mechanical devices can also be readily removed when needed and are stable at room temperature. Regarding the question of which IOL method is suitable in women with prior CS, a recent Cochrane review stated that there was insufficient infor-mation available to conclude on the optimal method.4
In this study, we compared 3 methods for second trimester cervical ripening and termination of pregnancy in previous CS patients with unripe cervix, which are vaginal dinoprostone, intracervical Foley’s catheter, and intracervical injection of hya-luronidase enzyme. We also compared time with delivery and success rate between the 3 methodologies.
This study was conducted in the Department of Obstetrics and Gynecology, Tanta University, on patients attending both out-patient and inpatient units. Study protocol was approved by the Human Research Ethics Committee, Faculty of Medicine, Tanta University, before the study began. The study was held in the period from April 1 to October 1, 2016. A total of 115 patients signed informed consent (IC) and were screened for the study; 25 of them were excluded due to reasons shown in Figure 1. In all, 90 patients were enrolled in the study (Figure 1).
All women were thoroughly informed about the study aims and discussion about the procedure, associated benefits and risks, and assigned written consent.
Inclusion criteria
Inclusion criteria were women with 1 lower transverse cesarean scar, singleton pregnancy, second trimester (16 to 28 weeks), scar thickness 5mm measured by transabdominal ultrasound, normally situated placenta, unfavorable cervix (Bishop score <5), and intact fetal membranes (Table 1).
Variable |
Group I: PGE2 |
Group II: Foley’s |
Group III: Hyal |
P Value |
Age |
27.5 ± 5.4 (17–40) |
28.9 ± 5.9 (18–40) |
29.1 ± 3.7 (19–35) |
0.407 |
BMI |
26.7 ± 3.4 (19–34) |
27.2 ± 3.9 (20–40) |
27.5 ± 4.5 (19–35) |
0.739 |
Table 1 Demographic data in the 3 groups
Abbreviations: BMI, body mass index; Foley’s, Intracervical Foley’s Catheter; Hyal, Intracervical injection of Hyaluronidase enzyme; PGE2, Vaginal Dinoprostone
Exclusion criteria
Exclusion criteria were women with 2 or more previous CS, classical CS, and previous uterine scar for gynecological con-ditions, eg, myomectomy, hysterotomy, congenital uterine abnormality, previous rupture uterus, uterine fibroids, pla-centa previa, premature rupture of membranes, and suspected chorioamnionitis (Table 2).
Variable |
Group I: PGE2 |
Group II: Foley’s |
Group III: Hyal |
Time to Effacement, h |
|||
Base |
27 |
24 |
26 |
10.4 ± 1.5 (7.5–14.1) |
15.4 ± 4.7 (8.1–26.1) |
9.2 ± 3.4 (6.4–22.3) |
|
Time to Delivery, h |
|||
Base |
27 |
24 |
26 |
14.2 ± 3.6 (11.2–27.2) |
20.1 ± 4.8 (12.9–29.5) |
15.8 ± 1.8 (12.6–19.2) |
|
Success (Delivery) |
|||
Base |
30 |
30 |
30 |
Success number |
27 |
24 |
29 |
Success percent |
90 |
80 |
96.7 |
Table 2 Time to effacement, time to delivery, and success rate in the 3 groups
Abbreviations: Foley’s: Intracervical Foley’s Catheter; Hyal: Intracervical Injection of Hyaluronidase Enzyme; PGE2: Vaginal Dinoprostone Side effect was reported only in 1 case in group 1; no serious adverse events were reported
All patients were assessed by history taking and clinical examinations and were investigated by routine investigation to check for general condition. Abdominal ultrasound was done to check for fetal presentation, number of fetuses, scar thickness, placental location, and uterine anomalies or fibroids.
The 90 patients included in the study were randomized into 3 study groups according to sequence of computer-generated block-random numbers.
Each group included 30 patients. These groups were as follows:
Group I: vaginal dinoprostone, referred hereafter as “PGE2”;
Group II: intracervical Foley’s catheter, referred hereafter as “Foley’s”;
Group III: intracervical injection of hyaluronidase enzyme, referred hereafter as “Hyal.”
Intervention
In Group I, PGE2 3 mg tablet was applied every 12 hours as a prostaglandin type to enhance cervical ripening and vaginal termination of pregnancy. If spontaneous contractions occurred every 2 minutes or if cervical score reached 9 or more, the next dose was not administered. If there were no effective uterine contractions after cervical score reaches 9, amniotomy with oxytocin IV infusion was commenced at a rate of 1 mU/min, and the infusion rate was doubled every 30 minutes until the uterine contractions become regular at 3-minute interval. If 48 hours passed without labor, it was considered method fail-ure, and in this situation, CS was offered for the patient.
In Group II, Foley’s catheter no. 22 was inserted through the cervix under aseptic technique and pushed by uterine sound under ultrasound guide. The balloon was inflated by 30 mL normal saline, traction was applied to the catheter, and then it was fixed by adhesive tape to the medial side of the thigh. If it got loose, more traction was applied. The catheter was kept for 48 hours if spontaneous expulsion did not occur. The catheter was removed earlier if there was spontaneous rupture of mem-branes, excessive vaginal bleeding, scar tenderness, or patient intolerance. After Foley’s catheter expulsion, amniotomy with oxytocin IV infusion was commenced at a rate of 1 mU/min and the infusion rate was doubled every 30 minutes until the uterine contractions become regular at 3-minute interval. If catheter did not enhance effacement of cervix or induce labor after 48 hours, it was removed and considered method failure, and under this condition, we shift to CS.
In Group III, hyaluronidase enzyme (Hylagan; Fidia Farmaceutica SpA, Italy) was used, imported by Egyptian Promoters Center for Pharmaceuticals, Cairo, which is sup-plied in prefilled syringe in 20 mg/2 mL solution. [AQ: 2] A dose of 0.5 mm was injected intracervically at 12 o’clock or at 6 o’clock position using 18G Disposable Spinal Needle. The pro-cedure was repeated every 12 hours for 48 hours. If labor occurred during the procedure or if a cervical score of 9 was reached, the next dose was not given and amniotomy with oxy-tocin IV infusion was done, but if labor did not occur after 48 hours, it was considered method failure and CS was done.
Labor was managed by the attending obstetrician and resi-dents. Uterine activity and progress of labor were monitored by cardiotocography. The outcome parameters of the study were duration of time until effacement is reached (cervical score 9), induction to delivery interval, and rate of successful vaginal delivery.
There were no significant difference
Cohort studies suggest that for women who have had a pre-vious cesarean birth and require IOL in a subsequent preg-nancy, there are potential benefits and harms associated with the IOL. These benefits and harms may vary considerably with the method used to induce labor. Few studies addressed the hyaluronidase enzyme injection cervical ripening and termination of pregnancy. One of these studies, which had been done on 168 women comparing placebo with hyaluro-nidase enzyme injection, showed that IOL was achieved in 82% of patients treated with hyaluronidase enzyme com-pared with 51% in placebo.11 From another perspective, we tried to investigate the safety of different vaginal termination of pregnancy methods in patients with previous 1 cesarean section scar in the second trimester
In our study, we tried to compare the hyaluronidase enzyme injection (Hyal group), which is a method with limited data in the literature, with the other 2 standard methods for cervical ripening and termination of pregnancy. The primary objective of this study was to compare “time of effacement” between hyaluronidase enzyme injections and the other 2 well-known methods. “Time to delivery,” “success rate,” and “adverse events” were considered in the study as secondary objectives.
Time to effacement was 9.2 ± 3.3 hours in the Hyal group compared with 10.3 ± 1.5 hours in the PGE2 Group. The dif-ference was statistically significant (P < .001) as shown in Figure 2. In addition, time to effacement was shorter than that of the Foley’s group (15.4 ± 4.5 hours). The difference was sta-tistically significant (P < .001) as shown in Figure 3. Time to effacement was shorter in PGE2 than Foley’s group. The dif-ference was statistically significant (P < .001).
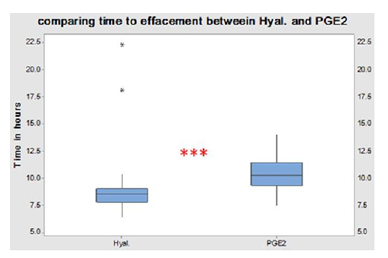
Figure 2 Comparing time to effacement between the Hyal and PGE2 groups. Hyal indicates intracervical injection of hyaluronidase enzyme; PGE2, vaginal dinoprostone.
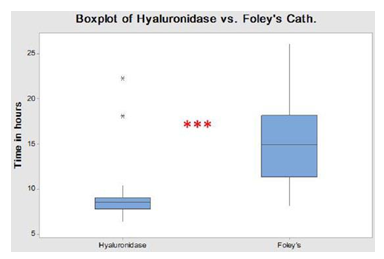
Figure 3 Comparing time to effacement between the Hyal and Foley’s groups. Foley’s indicates intracervical Foley’s catheter; Hyal, intracervical injection of hyaluronidase enzyme.
Looking at “time to delivery,” it was found that the PGE2 group has shorter time (14.2 ± 3.5 hours) than the Hyal group (15.7 ± 1.7 hours), which is explained by the effect of PGE2 on uterine contractility plus its cervical ripening effect. The differ-ence was statistically significant (P < .001) as shown in Figure 4.
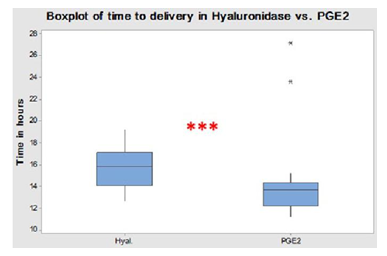
Figure 4 Comparing time of delivery between the Hyal and PGE2 groups. Hyal indicates intracervical injection of hyaluronidase enzyme; PGE2, vaginal dinoprostone.
“Time to delivery” was shorter with the Hyal Group than the Foley’s group (20.12 ± 4.8 hours). The difference was statisti-cally significant (P < .001) as shown in Figure 5.
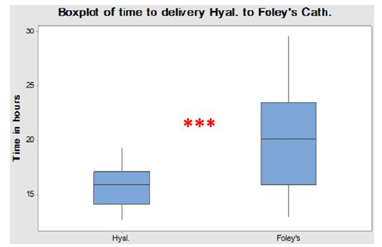
Figure 5 Comparing time of delivery between the Hyal and Foley’s groups. Foley’s indicates intracervical Foley’s catheter; Hyal, intracervical injection of hyaluronidase enzyme.
Success rate was 96.7% (29 of 30) in the Hyal group, 90.0% in the PGE2 group, and 80.0% in the Foley’s group (Figure 6). There was no statistical difference between the PGE2 group and both the Hyal and Foley’s groups (P < .05).
Adverse events were minimal; only 1 case in the PGE2 group (3.3%) had hyperstimulation, which was controlled by CS. No side effects were reported in the other 2 groups. No serious adverse events were reported.
We conclude that it is safe to go for vaginal termination of second trimester pregnancy in patients with previous 1 cesarean section scar with high success rate and minimal risk. The shortest “time to cervical effacement” and saving the patient from CS are achieved by applying the “Hyal” technique than the other 2 slandered methods: “PGE2” and “Foley’s.” However, applying the “Hyal” technique does not give the shortest time to delivery.
None.
Author declares that there is no conflict of interest.

©2017 El-Halwagy, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.