International Journal of
eISSN: 2574-8084


Case Report Volume 4 Issue 4
Department of Neurosurgery, University of Hassan, Morocco
Correspondence: Zine el Abidine Ennhaili, Department of Neurosurgery, University of Hassan, Teaching hospital Ibn Rochd, Morocco
Received: October 30, 2017 | Published: November 10, 2017
Citation: Ennhaili ZA, Chellaoui A, Ibahiouine K, et al. Intraventricular meningiomas, a rare location for a common tumor: about 2 cases. Int J Radiol Radiat Ther. 2017;4(4):408-410. DOI: 10.15406/ijrrt.2017.04.00105
Intraventricular meningiomas IVM, make up 0,5-3% of all intracranial meningiomas, and represent one of the most challenging tumors in neurosurgery. Being initially asymptomatic usually attains a large size before detection. we review through 2 cases of IVM managed in our neurosurgery department, the clinical, radiological and evolutionary features of these lesions.
Keywords: meningioma, intraventricular tumor, benign tumor
The intraventricular meningiomas are uncommon lesions. They represent 0,5 to 3% of all intracranial meningiomas,1,2 and observed more frequently at a younger age than meningiomas in other locations.3 They are classically large, because their silent evolution. The development of CT and MRI lastyears, offers to the neurosurgeons the opportunity to make precisely the diagnosis, and guide their surgical approaches. Meticulous and rational planning enable complete removal of these usually benign tumors, offering permanent cure and long term survival. This paper will discuss clinical, radiological findings, and surgical management of this pathological entity, through 2 cases of IVM managed in our neurosurgery department.
First case
A 17years old female, presented with increasing intracranial pressure syndrome, severe headache, vomiting, and papillary oedema grade1. The patient was without any sensory or motor deficit. The CT and MRI shows a huge intraventricular lesion located in the occipital Horne of the right lateral ventricle (Figure 1). The patient underwent a ventricular shunting, and the tumor was excised in a second time. The removal was complete using a temporo parietal approach, and the post operative status was stable, with improvement of the headache. The histological exam indicates a fibroblastic meningioma (Figure 2).
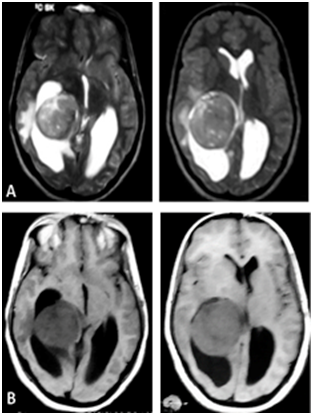
Figure 1 Axial (A) T2-weighted and (B) T1-weighted MRIs showing a right lateral intraventricular meningioma.Notice the regular aspect of the lesion.
Second case
A 15years old girl, consulting for severe headache, with vomiting, and diplopia. The physical examination shows no motor or sensory deficit, and right 6th nerve pulsy, with papillary oedema grade 2. CT and MRI show a very large intraventricular tumor, located at the right lateral ventricle (Figure 3) (Figure 4). The patient underwent ventricular shunting, and the tumor was removed in a second time. The excision was total using a temporo parietal approach, and the post operative status was simple, with improvement of the headache. The histological exam indicates a fibroblastic meningioma too.
The IVM represent only 0,5 to 3% of all intracranial meningiomas.4 They occur at a younger age than meningiomas in other locations. The mean age of our 2 cases is 16years confirming the data in the literature.4,5 The lateral ventricle is the first site of implantation of these tumors, than the third and the fourth ventricles’. Lateral ventricular tumors predominate on the left side, with more than 90% occurring in the region of the trigone.3,6‒8 The principal clinical presentation of the IVM, is the raising intracranial pressure,3,4 concording with our 2 cases. A brutal increase in the intensity of headache associated with postural change due to a pedunculated tumor causing intermittent CSF obstruction is an important sign to search. The progressive cognitive problems and loss of memory can be alarming features to this pathological entity. Visual symptomatology is most often related to the accompanying secondary optic atrophy or hydrocephalus. Rarely hemorrhage may be a revealing sign.9,10
On CT and MRI, IVM have a lobulated regular shape, because the free space to expand for tumor growth. The irregularity of the lobulation signs malignancy. On CT scans, these tumors are hyperdense and may contain calcifications. Meningiomas are or hypointense on T1, iso or hyperintense on T2. Contrast enhancement is important on both CT and MRI.6,11 The histological findings described showed that, these tumors are predominantly fibrous, fibroblastic, or psammomatous and exceptionally malignant.11,12
The surgical excision remain a logical solution and despite the difficulties and the large size, total removal must be the aim.13,14 Several approaches are used for the lateral ventricle: The temporo parietal approach described by Cushing, posterior middle temporal gyrus approach recommended by Dela Torre, and posterior parieto-occipital approach described by Cramer.6,14‒16 The mortality depends on the experience of neurosurgeon, and its knowledge of the anatomy. In literature it variants between 0 and 42%, however, mortality is around 25%, as reported by Fornari et al.4,17 The endoscopic resection seems to be less invasive, and safer, for the smaller IVMs, but not practical for the large, highly vascular ones.18 Radio surgery is also an effective treatment modality, it’s indicated for tumor with a small size not exceeding 3cm.
The IVM are rare. They have prevalence in a much younger age group than intracranial meningiomas at other sites. The increasing cranial pressure is the most common clinical presentation. CT and MRI findings are non specific. The treatment is based on surgical resection.
None.
Author declares that there is no conflict of interest.

©2017 Ennhaili, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.