International Journal of
eISSN: 2574-8084


Case Report Volume 4 Issue 3
Hospital Begoa, Spain
Correspondence: Estela Fernadez, Hospital Begoa, AVDA. Pablo Iglesias, Nº 92. 33204, Spain, Tel +34 606 74 24 73
Received: August 01, 2017 | Published: October 10, 2017
Citation: Fernadez E. Breast elastography: present and future. Int J Radiol Radiat Ther. 2017;4(3):379-384. DOI: 10.15406/ijrrt.2017.04.00098
Objective: Make a literature review of breast elastography, an imaging technique not so new today, for many still unknown in diagnostic ultrasound, which emerges in order to characterize complementarily tissues of the breast, contributing to differential diagnosis between benign and malignant lesions.
Review: Today breast cancer is by far the most common cancer in women. Mammography and ultrasound has become an indispensable diagnostic tandem within the breast image, increasing the sensitivity of ultrasound mammography by 15% and both techniques are able to characterize most breast lesions. Using these techniques together we achieve a sensitivity of 85-100% and a specificity of 76-80%, specially in dense breasts where mammography is significantly limited.1
Keywords: breast elastography, imaging, ultrasound mammography, diagnostic, pathologic
SWE, shear-wave elastography; FOV, field of view; ARFI, acoustic radiation force imaging impulse; SD, standard deviation
Gradually, ultrasound equipment have suffered a major technological development, starting with the Doppler log or the introduction of harmonics, until the recent use of intravenous contrast and of course elastography. The first team was launched in 2003, later emerging numerous similar systems have been launched different commercial houses, which have been incorporated to ultrasound equipment progressively.2 The results have been demonstrating that this technique is able to differentiate benign lesions from those with malignant behavior.3‒5 The technique of palpation in which stiffness of tissues is evaluated by squeezing is well known. In many ways, elastography is an advanced version of palpation, providing images and measurements related to stiffness. A variety of elastography techniques have been developed in research laboratories over that last 25years.6,7
Pathologic conditions such as inflammation and tumors can change tissue elasticity. Therefore, in vivo elasticity measurements of various tissues can be valuable noninvasive test for the diagnosis and management of various pathologic conditions. However, only a limited number of studies have been conducted to evaluate the elasticity of various tissues.8,9
Elastography provides different morphological information that is obtained in B-mode. This technique quantifies the elasticity (stiffness) of in vivo and in real time, from the relative displacement of the tissue when subjected to an external compression tissues. Elasticity decreases in those stiffer lesions and this feature can be used as an auxiliary tool in the diagnosis of breast cancer, since as we know that malignant lesions have less elasticity and greater resistance to displacement, relative to benign lesions.1,10‒12 Garra et al.10 were the first to study about elastography,10 in which they demonstrated that this is a good tool to differentiate solid lesions nature.
To understand elastography, it is essential to know how the elasticity of an element is measured, in this case breast tissue. The result of the ratio of the compression performed to a tissue and deformation obtained therefore is what is called elasticity or Young's modulus (Figure 1). This behavior was studied by Thomas Young in the nineteenth century, however the concept was developed in 1727 by Leonard Euler.
We can distinguish two types of elastography
Compression elastography and "shear-wave" elastography (SWE).
Compression elastography (strain) produces an image based on the displacement of the tissue from an external or patient source, and the movement of the tissue shows the direction of US beam propagation. This technique allows a qualitative assessment of the lesion. With real-time ultrasound elastography, the physical properties of soft tissue are revealed through characterization of the differences in stiffness between the region of interest and the surrounding tissue based on mechanically induced deformation (strain) of structures during B-mode scanning.8
Data acquisition and interpretation of elasticity images are largely dependent on the examiner´s experience, and significant interobserver variability has been found.3,4,13,14 The real-time elastogram is displayed with a scale based on the relative strain of the tissues. The technique to obtain the optimal images varies with the algorithm used by the manufacturer of the ultrasound system. Monitoring of the B-mode image to confirm the lesion is only displaced in depth during scanning and otherwise moving in the field of view (FOV) will allow optimal images. With the displacement technique, one cannot be surveying the breast; scanning must be done in one stationary position.
Modern US devices allow combined elasticity and 2D real time assessment of tissues or lesions, using the same probe as conventional ultrasound imaging.15 Sonoelastography demonstrates the elasticity of a lesion related to the elasticity of the surrounding tissue,13 so the final result is based on the comparison between pre and postcompression data,10,15,16 however it´s difficult with this technique to amount of the stress during the compression process.
In contrast to strain elastography, SWE uses an acoustic radiation force impulse created by a focused ultrasound beam, which allows measurement of the propagation speed of shear waves within the tissue to locally quantify its stiffness in kilopascals or m/s. Because the speed of sound through tissues is dependent on the “stiffness” of these tissues, a quantitative value of the stiffness can be obtained, shear wave velocity is proportional to stiffness. This technique has been reported to be highly reproducible for assessing elastographic features of breast lesions within and across observers, in contrast to strain elastography.3,5,17
SWE can be performed in real time; however, to obtain optimal images, remaining in the same plane for several seconds will improve image quality. SW propagation is depth limited, if a lesion is deeper than 3-4cm or is very superficial, one may not obtain a reliable result. Repositioning the patient to make the lesion more accesible can help in some cases.17 Also very fibrous breasts with absence of adipose tissue arround can complicate the results. However, sometimes the compression applied can be excessive and we can see an artificial or artefactual stiffness is seen codified into yellow or red color, generally radiating from the skin surface.18
For the accomplishment of this article I have reviewed several studies that I believe have been determinant for the validation of this ultrasound technique. With SWE, a quantitative measure of the lesion stiffness is obtained either in an FOV or pixel by pixel using a color map. According to a recent study, a value of 50kPa or greater is indicative of a malignant lesion, whereas a value less of 50kPa is indicative of a benign lesion (Figure 2).5,14,19‒21
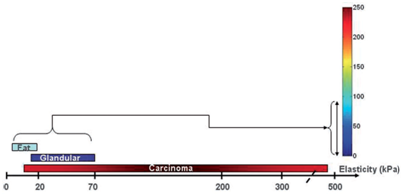
Figure 2 Typical values of tissue elasticity in the breast. Tissues with relatively low elasticity (fat and glandular) are coded in blue using SWE [21].
The different commercial houses have different trade names in this physical basis
Acoustic Radiation Force Imaging Impulse (ARFI), Shear Wave Point Quantification, quantitative elastography ShearWaveTM, etc. Several clinical studies showed that different conditions, such as ageing, inflammation or presence of malignancy22,23 are generally well-correlated with differences in stiffness between surrounding normal and pathological tissues.24,25
First af all, I have to remark that elastography is a technique which characterize a lesion previously detected in B mode-ultrasound, so it´s not a diagnostic method. According to the equipment type, various colors (256hues) or gray shades are superimposed on 2D images. It is useful to evaluate both images, B-mode and elastogram at once on the monitor (B and elastography mode) to keep the anatomical precision reference whose injury decreases in elastosonographic images and to assess real-time changes in elasticity.
I want to highligt that the two main factors in elastographic evaluation are size and stiffness. In strain elastography we can use a grayscale, where the adipose tissue (more elastic than glandular) appears clear while the glandular tissue is darker. In function of hardness tissues will appear darker. In this same grayscale, also harder injuries often show an increase in size compared to images in B mode which responds to a desmoplastic reaction present in a lot of breast tumors. For less severe injuries, the lesional size of the image does not change or decreased significantly compared to the B mode. The cysts have a characteristic pattern which remember a coffee bean with a component bright white and one dark with white center. With respect to the chromatic scale, the colors vary according to the degree of tension or elasticity of the components of the lesion. The colors assigned to the different degrees of elasticity vary depending on the different equipments,12 most equipments display tissue stiffness in a red to green to blue scale, designating hard, intermediate and soft tissue, respectively.
The different elasticity patterns in strain elastography were classified with a five-point scoring system in Ueno classification, (Tsukuba University, Japan)4 (Figure 3) in one of the first clinical trials for the assessment of breast elastography. A large number of authors26‒28 in their studies establish an equivalence between BIRADS classification and the UENO´s scale.
In UENO´s scale there are 5 scores (several examples are shown below obtained with a equipment Applio 500 Platinum, Toshiba Medycal Systems, Japan)
Score 1 (E1): corresponds with a homogeneous strain or elasticity throughout the lesion, which is homogeneously shows green. A variant of this type (1*) is the imaging of cysts: the image in three layers produced by reverberation artifacts (Figure 4). They are classified as benign.
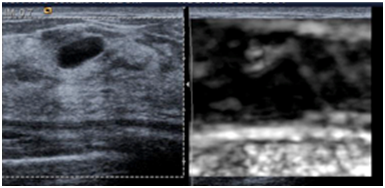
Figure 4 Score 1. Ultrasound B-mode (left) and elastography in grey scale (right)showing typical image with three layers of a benign cyst.
Score 2 (E2): Indicates an essentially elastic lesion with areas of lack of elasticity (mosaic pattern in green and blue).They correspond with benign lesions (usually fibroadenomas) or proliferative lesions without atypia.
Score 3 (E3): Is about elasticity in the periphery of the lesion and absence in the center (center periphery green and blue) (Figure 5) (Figure 6). The most are also benign (fibroadenomas, papillomas, proliferative lesions mainly).
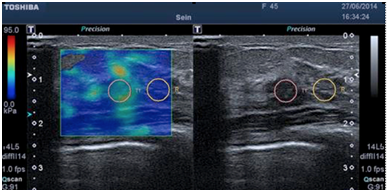
Figure 5 Score 3. Elastography (left) and ultrasound B-mode (right) images of a soft (green) benign breast fibroadenoma.
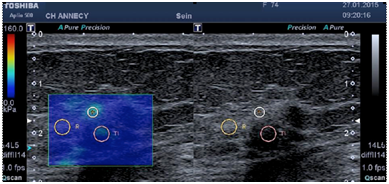
Figure 6 Score 3. Elastography (left) and ultrasound B-mode (right) images of a soft (green) benign fibrocystic changes.
Score 4 (E4): Indicates no elasticity throughout the lesion (the entire lesion is blue).
Score 5 (E5): Corresponds with no elasticity throughout the lesion and the surrounding area (blue area is larger than the lesion itself) (Figure 7). It corresponds to the increase in size described in grayscale model.
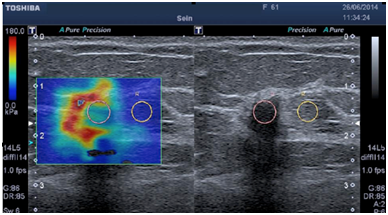
Figure 7 Score 5. Elastography (left) and ultrasound B-mode (right) images of a hard (red predominantly and green) malignant invasive ductal carcinoma.
Injuries that do not vary significantly in size in grayscale, often also correspond benign lesions. However, should correlate findings with B-mode images and if discordance, biopsy the lesions. The Score 4 or 5 are primarily lesions malignant circumscribed, homogeneous, such as carcinoma mucinous tubular (score 4) or malignant lesions that are infiltrating the tissue adjacent or showing component extensive intraductal (score 5). The recommendation in all cases is the biopsy.12
Equivalence with the BI-RADS classification is made considering that the BI-RADS 2 lesions correspond to the scores of elastography 1 and 2 and the rest of the lesions are univocally with scores of elastography.1 The sonographic features for BIRADS 3 lesions having a malignancy rate less than 2% and BIRADS 4 lesions having a malignancy rate between 2% to 95% have been shown to have substantial overlap with each other.29‒31
Therefore biopsy is presently used to define the suspicious lesions, but the rates of cancer detection in biopsies are only 10-30%.32,33 Sonoelastography arises as a non invasive method of imaging to evaluate tissue stiffness, it has been used to improve diagnostic confidence and increased specificity of conventional sonography. Therefore unnecessary short term follow up or biopsies were able to be reduced.34‒36
>On the other hand, SWE measured tissue stiffness by Young´s modulus (as we defined before) which is expressed in pressure units, usually in kilopascals (kPa). In SWE, shear waves created by ultrasound system propagate in tissue at speeds of 1-10mm/sec, equivalent to a 1-300kPa. Young´s modulus or elasticity (E) and shear wave propagation speed (c) are directly linked in the next formula: E=3pc2 , in which p is density of tissues in kg/m3. We know the density of tissues (1,000kg/m3), elasticity of tissue can be studied when shear wave propagation velocity c is measured. In fact, SWE can provide us quantitative information in kPa and also in m/sec.37
Benign tumors tend to be on SWE homogeneusly soft (usually code in blue) and malignant lesions are more heterogeneus (usually code in red). When lesions are harder like cancers, the stiffness area which sorrounds the mass on SWE corresponds in most cases to the echogenic halo identified on B-mode.18,37,38 When it is too hard to propagate the shear wave the central area of the lesion and appears without a color code.17,37
With this technique the normal breast tissue elasticity varies from 1 to 70kPa whereas the elasticity of carcinoma covers a much wider range, from 15 to more tan 500kPa. Breast lesions having a elasticity above 100 or 120kPa are commonly considered to be hard. We have to consider that benign lesions are harder tan normal breast tissue but softer than cancer lesions, however there are exceptions like hyalinized fibroadenomas and fat necrosis also, which can be false positives at US elastography.
SWE mode is able to image fine elastic contrast as well as large elasticity differences. The quantitative estimation of this parameter offer previously unavailable information that could be incorporated into the diagnostic decision making process.21 3 mapping types are available: speed (m/s), elasticity (kPa) and waves propagation (Figure 8). The system calculate mean elasticity measured inside ROI (Ave) and also standard deviation (SD) of these measurements. SD value is an indication of homogeneity of values inside ROI and can be correlate to its reliability. Some examples are shown below Figure 9 & 10.
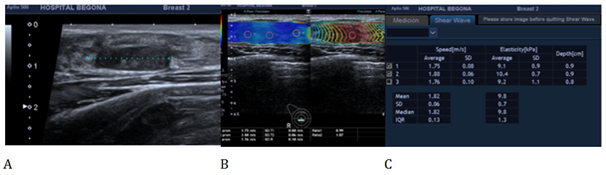
Figure 9 B-mode and shear-wave elastography (SWE) images in a 25 year old woman with a fibroadenoma in right breast. A) B-mode image shows a 18 mm, homogeneus hipoechoic mass, B) SWE image shows a soft nodule with a predominant blue pattern. In C) the mean elastic value of that lesion is 9.8kPa. The mean, median and standard desviation of elasticity values in C) were measured in kPa and m/s by placing the region of interest (ROI) over the stiffnest part of the lesion.
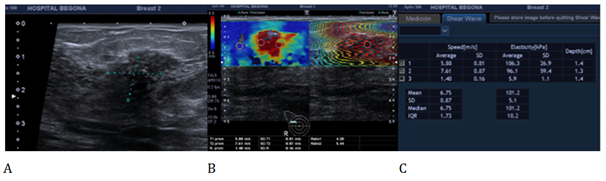
Figure 10 B-mode and shear-wave elastography (SWE) images in a 43 year old woman with a invasive ductal carcinoma in right breast. A) B-mode image shows a 14 mm, heterogeneus mass with microcalcifications inside, B) SWE image shows a heterogeneus and hard lesion with a red pattern. In C) the mean elastic value of that lesion is 101.2 kPa. The mean, median and standard desviation of elasticity values in C) were measured in kPa and m/s by placing the region of interest (ROI) over the stiffnest part of the lesion.
In a multicenter study of 874 breast lesions (614 benign and 260 malignant) Rizzatto et al.,39 found a high specificity in bening lesions with a negative predictive value of 98% related to the entire group of lesions and 100% in lesions ≤5mm.39,40 Tozaki et al.,38 in a recent paper the cut-off set to discriminate bening from malignant breast lesions is 3,59m/s and mean velocity in 76,5% of malignant lesions is higher tan in benign (4,49m/s vs 2,68m/s).38 Berg et al.,19 showed that in SWE the greatest specificity for benign lesions, not influencing sensitivity, is associated with Young modulus value Emax ≤80 Kpa represented with homogeneusly blue color map.19
Benign lesions such as complicated cysts, many fibroadenomas and also fat necrosis and radial scars can often show elastographic multilayered color maps because they are not homogeneous lesions associating in some cases a fibrous reaction simulating malignant lesions. On the other hand malignant lesions are deformed with difficulty and show complex elastic modulus. Sometimes discordant malignant cases show liquefaction necrosis, blood or sarcomatous components can give larger size nodules or on the contrary, in very small size and these factors can affect elasticity.41
Gisuppetti et al.42 show that the histological type is a factor that plays an important role in elastography evaluation. For example, ductal lesions have different patterns of elasticity due to fibrohialine components, while in lobular neoplasms the minimal fibrosis, poor cellular cohesion and moderate desmoplastic reaction also can modify the patterns.42
We can found some limitations in the elastographic study, because of the tissue breast structure and properties of the nodules mainly, and also due to the US technique itself. And adequated and standarized compression is very important which can influence elasticity score.43 An important recommendation is that the US transducer should be in very light contact with skin at the beginning of the exam because pressure and strain are not longer proportional beyond a certain degree of compression.44 Also lesions in a very superficial or a deeper location are more difficult to study, including lesions very close to the nipple.45,46
Shear wave elastography emerges as a promising technique, providing us an important quantitative and reproducible information about breast lesions with diagnostic accuracy at least as good as greyscale ultrasound with BI-RADS classification. I think that the real goal of this technique is to improve classification in the categories BI-RADS 3 and BI-RADS 4, providing valuable structural propierties to better target patients towards clinical follow-up or biopsy, which means a reduction of innecesary biopsies, contributing in a better women breast management.
None.
Author declares that there is no conflict of interest.

©2017 Fernadez. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.