International Journal of
eISSN: 2574-8084


Case Report Volume 4 Issue 1
1Department of Medical imaging, Lebanese Hospital Geitaoui HLG-CHU, Lebanon
2Department of Pathology, Lebanese Hospital Geitaoui HLG-CHU, Lebanon
3Department of General Surgery, Lebanese hospital Geitaoui HLG-CHU, Lebanon
Correspondence: Eliane El Khoury, Department of General Surgery, Lebanese University, Bldg. 21, Str. Tamich no. 1, Deek el Mehdi, North Metn, Mount Lebanon, Lebanon, Tel +961 4 915234
Received: July 18, 2017 | Published: August 21, 2017
Citation: Chalhoub N, Mourad C, Mouaccadieh L, et al. Serous cystadenoma of the pancreas: radio-anatomical correlation. Int J Radiol Radiat Ther. 2017;4(1):326-328. DOI: 10.15406/ijrrt.2017.04.00087
Serous pancreatic cystadenomas account for approximately 16% of pancreatic neoplasms and are -frequently discovered incidentally on abdominal imaging studies. The diagnosis of these benign neoplasms can be challenging, especially when it comes to distinguishing them from the malignant mucinous cystadenomas or intraductal papillary mucinous neoplasms. In this article, we report on a case of giant pancreatic cystadenoma and the correlation between the radiologic and pathologic findings macroscopically and microscopically. The patient underwent pancreaticoduodenectomy and excellent correlation was found between the preoperative imaging studies and the resected specimen. This article sheds the light on a rare case, especially that there are very few reports on similar cases of giant serous cystadenomas of the pancreas in the literature.
Keywords: pancreas, cystic neoplasms, serous cystadenoma
MDCT, multi-detector computed tomography; MRI, magnetic resonance imaging; SCAs, serous cystadenomas; SCNs, serous cystic neoplasms; MCN, mucinous cystic neoplasms; IPMN, intraductal papillary mucinous neoplasm
Pancreatic serous cystic neoplasms are rare lesions accounting for approximately 16% of primary cystic pancreatic neoplasms.1 These lesions are now encountered with greater frequency due to increased availability and use of high-resolution imaging such as multi-detector computed tomography (MDCT), magnetic resonance imaging (MRI) and MR cholangiopancreatography (MRCP), and are often incidental findings.2 3% of serous cystadenomas are characterized as having malignant potential with local infiltration and distant metastases despite the fact that they are considered benign lesions.2 MDCT is the initial imaging modality of choice for evaluation of cystic lesions of the pancreas.3
The characteristic imaging appearance is a honeycomb pattern with central scar or central calcification. However, serous neoplasms can be further classified into microcystic, polycystic, oligocystic, and solid patterns according to their imaging appearance.1,4 In order to characterize pancreatic serous neoplasms accurately, the prime diagnostic approach is to differentiate non-mucinous type cystic tumors such as serous cystadenomas from mucinous types of tumors, including mucinous cystic neoplasms (MCNs) or intraductal papillary mucinous neoplasms (IPMNs).5 The reason is that serous neoplasms should be managed as a benign disease while mucinous lesions are potentially or overtly malignant lesions.5 Curative complete resection of the tumor is restricted to symptomatic patients, is recommended when it increases in size upon follow-up, and when confident non-invasive differentiation from a more aggressive lesion is impossible.2
Microscopically, serous neoplasms are designated as having cysts lined by glycogen-rich, cuboidal cells, filled with clear and thin serous fluid with richly vascular collagenous or hyalinized stroma.2 The aim of this article is to correlate the CT findings of these lesions with the anatomical and histopathological appearance.
This article illustrates the case of a 72year-old-lady, non-smoker, with no special occupational exposure, and no history of personal or familial cancer, presenting for a few-week-history of non-specific abdominal pain, slightly increasing after meals, associated with abdominal distention. She recalled that the pain had been present intermittently for three years. She underwent abdominal ultrasound and was found to have a small pancreatic cyst. The patient was lost to follow-up and presented few years later with distention and steady pain.
Her laboratory data upon admission were within the normal limits. CT scan was performed outside our institution and the report revealed the presence of a 15cm hypodense mass of irregular contours and heterogeneous post contrast enhancement located in the uncinate process of the pancreatic head, containing internal calcification. A biopsy was taken and sent for pathology. Meanwhile, for better characterization of the lesion, an abdominal MRI was done and revealed a large, lobulated, well defined pancreatic mass showing multiloculated cystic appearance with a central stellate scar that enhances in the delayed phase. The mass was displacing the adjacent vascular structures without evidence of invasion.
There were no signs of aggressiveness or local or distant metastases. Histopathological analysis had been performed by a single pathologist. The microscopic appearance of the resected specimens was described and correlated with the radiological finding which is the main purpose of this article (Figure 1). Due to the fact that the patient was symptomatic and the lesion was increasing in size since the last ultrasonography, a pancreaticoduodenectomy (Whipple procedure) was performed. The patient was discharged home on post-op day. She developed a pancreaticocutaneous fistula, from which she recovered with conservative management (Figure 2‒6).
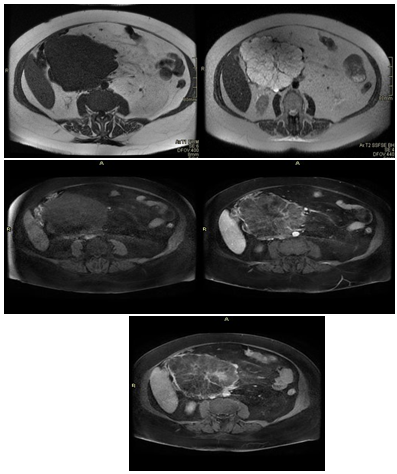
Figure 1 Axial MRI of the abdomen performed in multiple sequences: T1 (top left), T2 (top right) and after gadolinium administration: Pre-contrast (middle left), post-contrast (middle right) and delayed phase (bottom) showing large lobulated and multiloculated cystic pancreatic mass characterized by a central scar that enhances in the delayed images.
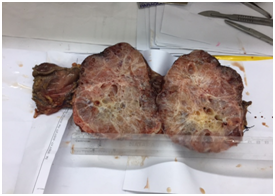
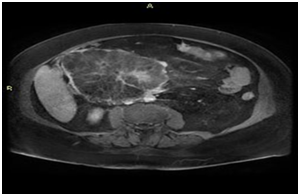
Figure 3 Gross examination shows a pancreatic mass measuring 16x16x9cm. The cut surface shows a honeycomb pattern. On microscopic examination. The top image shows the cut surface of the specimen with an irregular, central yellowish area and a multicystic pattern.
The main challenge posed by cystic tumors of the pancreas is to establish an accurate diagnosis in order to avoid extensive resections and morbid procedures for benign disease especially that the typical patient is an elderly woman6 – a patient population who frequently have multiple comorbidities placing them at high operative risk. The central scar seen on our patient’s CT-scan is pathognomonic for serous cystadenoma.7 However, it has never been reported in giant serous cystadenomas in the literature.7,8 Giant serous cystadenomas are defined as measuring 10cm or more,7 just like the case we describe here.
The radiologic properties of our patient’s tumor – namely the central scar, internal calcifications, irregular borders and the absence of aggressive features – are typical of serous cystadenomas.1 Correlation between the radiologic and pathologic findings reported in the literature is variable. A study by Johnson et al. in 1988 reported that 47% of serous cystadenomas and 50% of mucinous cystadenomas were originally labeled as atypical by the radiologists who evaluated them.7 These findings were similar to those of the study by Curry et al.,9 who concluded that CT-scan was not a sensitive tool for differentiating cystic tumors of the pancreas due to the high variability in their radiologic appearance.9 This still applies nowadays despite all the ongoing research in this field, making the differentiation between serous and mucinous cystadenomas one of the most difficult tasks for the radiologist: while typical radiologic characteristics allow diagnosis in 60% of the cases, imaging studies favor one diagnosis over the others in atypical cases, where definitive diagnosis still requires resection.11 However, some recent studies showed a better correlation between preoperative radiologic findings and postoperative diagnosis on the resected specimens,10 probably owing to the improved resolution of modern CT-scanners and increasing radiologist expertise with these tumors and the development of radiologic criteria to aid in the diagnosis.
CT-scan or MRI allow to delineate the relationship to adjacent organs and vascular structures in order to determine resectability and allow operative planning (en bloc resection of involved adjacent organs, vascular resection and reconstruction, palliative surgery for non resectable tumors or poor operative candidates).7 In our case, the tumor was seen displacing the adjacent vascular structures without invading them, but no mention was made on the fact that it was hypervascularized, which led to significant blood loss intra-operatively, requiring blood transfusions.
Despite the certainty that our patient had a serous cystadenoma, she underwent pancreaticoduodenectomy since her tumor was symptomatic and large (>4cm).1 To note that no study proved the correlation between tumor size and the risk of malignancy, even though it can be postulated that malignant potential increases with the extent of tumor growth.7 The preoperative radiologic findings correlated well with the macroscopic and microscopic appearance of the specimen, which contained a central scar and multiple cysts (Figures 3‒5).
The importance of an accurate preoperative diagnosis becomes crucial in cases where conservative management can be contemplated. In these patients, the possibility of a malignant tumor must be ruled out with high certainty. This may require additional diagnostic tests including endoscopic ultrasound, fine needle aspiration biopsy and cyst fluid mucin, amylase and tumor marker levels.1,6 If the cyst fluid contains mucin, atypical cells or elevated CEA (>192ng/mL) or CA19-9 levels, the tumor is a mucinous cystadenoma, which must be treated as a malignant tumor.1,6 Cyst fluid amylase levels <250 IU/L rule out pancreatic pseudo cysts.1 If the diagnosis remains uncertain, despite all these investigations, resection becomes mandatory.1
In our case of giant serous cystadenoma, the postoperative findings on the specimen were correlated to the radiologic features seen on preoperative CT-scan and MRI. However, this is not always the case, given that most studies still report high rates of uncertain diagnoses. Currently, no imaging modality alone allows to obtain an accurate diagnosis. In fact, the combination of clinical history, physical findings, laboratory results, imaging studies and data from invasive procedures like fine needle aspiration biopsy and endoscopic ultrasound permits the diagnosis. However, with the continuous development of imaging techniques and improvements in imaging protocols, and with the ongoing research on this challenging topic, we can hope for the elaboration of imaging modalities that allow an accurate diagnosis without resorting to invasive procedures or even resections in doubtful cases.
None.
Author declares that there is no conflict of interest.

©2017 Chalhoub, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.