International Journal of
eISSN: 2574-8084


Case Report Volume 3 Issue 3
1Department of Head and Neck Surgery and Pathology, National Cancer Institute, Colombia
2Department of Surgery, National University of Colombia, Colombia
3Department of Head and Neck Surgery and Pathology, Marly Clinic, Colombia
Correspondence: Enrique Cadena, Department of Head and Neck Surgery and Pathology, National Cancer Institute, Bogotá, 1st Street # 9-85, Colombia, Tel 5713341111
Received: May 29, 2017 | Published: June 27, 2017
Citation: Cadena E, Romero-Rojas A. Parathyroid carcinoma presenting as an acute pancreatitis. Int J Radiol Radiat Ther. 2017;3(3):226-228. DOI: 10.15406/ijrrt.2017.03.00061
Parathyroid carcinoma is the cause of only 1% of hyperparathyroidism cases. The incidence of acute pancreatitis in patients with hyperparathyroidism was reported to be only 1.5%. The occurrence of pancreatitis in patients with parathyroid carcinoma is unusual, ranging from 0% to 15%. Here, we report a very rare case of parathyroid carcinoma presenting as an acute pancreatitis in a 45years old woman, who was suspected for hypercalcemia and higher levels of intact parathyroid hormone. The parathyroid carcinoma was verified with ultrasound, CT Scan, and single-photon emission computed tomography. The pathological anatomy report showed a minimally invasive parathyroid carcinoma. Following surgery, the patient was free after almost a 4years follow up.
Keywords: acute necrotizing pancreatitis, hypercalcemia, primary hyperparathyroidism, parathyroid carcinoma
HPT, hyperparathyroidism; PHPT, primary hyperparathyroidism; SPECT, single-photon emission computed tomography; CT, computed tomography; iPTH, intact parathyroid hormone.
Acute pancreatitis is a severe condition with a high mortality rate and it is most commonly caused by Gallstone´s Disease and excessive alcohol use.1,2 Acute pancreatitis caused by hypercalcemia due to primary hyperparathyroidism (PHPT) is very rare.3 The relationship between acute pancreatitis and hypercalcemia was first reported in 1947, but it was not fully appreciated until 10years later when pancreatitis was reported to be a specific clue to diagnose PHPT.4 Primary hyperparathyroidism occurs in 0.2-0.5% of the population.5 A single parathyroid adenoma accounts for 85% of all sporadic primary hyperparathyroidism. Less common causes include parathyroid hyperplasia of all four glands, represented by only 10% of sporadic PHPT, and multiple adenomas, which constitute only 4%.6 Rare causes of pancreatitis include parathyroid cancers and cysts, but is less than 3% of all cases.6 Here, we present a case of acute pancreatitis caused by parathyroid carcinoma in a 45years old female.
A previously healthy 45years old female was admitted to the emergency department with sudden onset abdominal pain of 1-day duration. The pain was localized at the epigastrium and was associated with several vomiting and diarrhea episodes. The patient´s medical history was unremarkable. She was not taking any medications and had no history of drug or alcohol abuse. During the admission process, her vital signs were within normal limits, with a body temperature of 37°C, heart rate 72, and blood pressure 130/80. Physical examination was notable except for a mild tenderness on the upper abdomen. There were no palpable masses or peritoneal irritation. The rest of the physical examination was normal. Lab tests revealed a white blood cell count (11,8K/uL), with normal hemoglobin (12,5g/dl). Blood chemistry revealed a normal glucose level (90mg/dl), elevated amylase (912U/L), high calcium (13,4mg/dl) and low phosphorus (2.5mg/dl) levels. Kidney and liver function tests, albumin and triglyceride levels were all within normal limits. The patient was treated initially with intravenous fluids and H2 blockers, and no oral via. Abdominal sonography showed a diffusely enlarged hypoechoic pancreas surrounded by free fluid. Cholelithiasis was not detected. Enhanced CT demonstrated diffuse pancreatic enlargement and edema. BALTHAZAR grade C (Enlarged pancreas associated with haziness and increased density of peripancreatic fat).7
Based on these clinical, radiographic and laboratory results, the diagnosis of acute pancreatitis was made and the etiology of hypercalcemia was suspected. Further evaluation confirmed the primary hyperparathyroidism diagnosis, with elevated parathyroid hormone levels (iPTH: 462pg/ml, normal range 10-65pg/ml). Ultrasound and Tc-99m-sestamibi SPECT (single-photon emission computed tomography) scan examination demonstrated a solitary mass below the left lobe of the thyroid gland, compatible with lower parathyroid (Figure 1) (Figure 2). A head and neck computed tomography (CT scan) was performed; it showed an enlargement of the left thyroid lobule, but it was not clear if there was a parathyroid tumor (Figure 3). When the abdominal symptoms were completely controlled, the patient underwent surgical neck exploration finding a small left thyroid with a large brown polar nodule, which was sent for frozen section. Analysis confirmed an enlarge parathyroid gland adjacent to the left thyroid lobule, with local invasion of surrounding tissues (Figure 4). The decrease in serum calcium levels and normalization parathyroid hormone levels were confirmed postoperatively. At three and sevenmonths following surgery, the iPTH level was 34pg/ml, then 26pg/ml; calcium level was 8,7mg/dl, then 8,8mg/dl; phosphorus was 3,27mg/dl, then 3,32mg/dl, respectively.

Figure 1 Ultrasound of neck: Showed upper left 8mm thyroid nodule (TIR), and lower left 30mm parathyroid (PT).
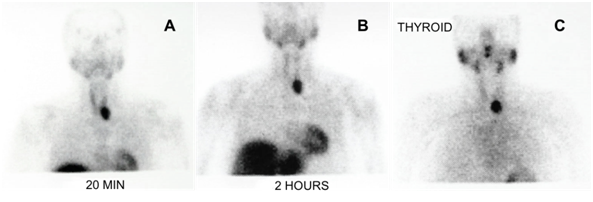
Figure 2 99mTc-Sestamibi SPECT Scan: (A) Early phase (20 minutes post injection) shows thyroid parenchyma with increased focal uptake in the lower left lobule. (B) Late phase (2 hours post injection) shows persistent focal uptake in the lower left lobule of thyroid. (C) Thyroid 99m Tc-sestamibi SPECT scan also shows focal uptake in left thyroid lobule.
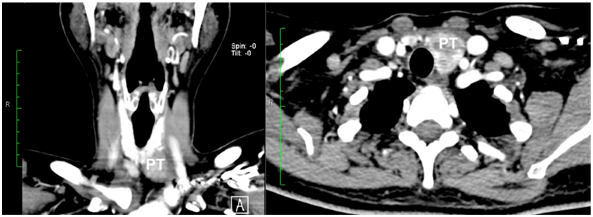
Figure 3 Head and neck CT Scan, showed inferior polar nodule of the left thyroid lobule, finally it was consistently with a parathyroid tumor.
PT: left parathyroid.
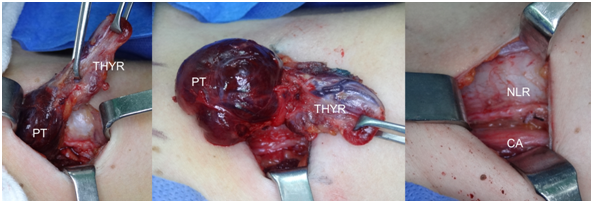
Figure 4 Head and neck exploration showed a large parathyroid gland adjacent to the left thyroid lobule, it was found with local invasion of surrounding tissues.
PT: Lower Left Parathyroid; THYR: Left Thyroid Lobule; CA: Left Carotid Artery. NLR: Recurrent Laryngeal Nerve
The final histopathology study revealed a 3.5cm x 3.2cm hard nodule adjacent to the left thyroid lobe (Figure 5). The lobe was surrounded by a dense, fibrous capsule that adhered tenaciously to adjacent tissues. Histology showed that chief cells, the predominant cell type, were arranged in solid sheets and organoid groups with a trabecular pattern that infiltrates the capsule and extended to the periparathyroidal adipose tissue with perineural invasion (Figure 6). There was mild atypia cellular without mitotic activity. Scattered foci of comedonecrosis occurred at the periphery of the neoplasm. There were no vascular invasion and no metastatic lymph nodes found. The final diagnosis was a parathyroid carcinoma minimally invasive. No radiotherapy or chemotherapy were administrated. After a period of 44months follow up, not recurrence was detected.
Since Cope and colleagues in 1957 described pancreatitis as another manifestation of hyperparathyroidism,4 several publications report that as many as 7%-19% of patients with PHPT have associated pancreatitis.3,8‒10 The mechanism of PHPT-induced pancreatitis is still controversial. Several studies have proposed that calcium-phosphate deposition in the pancreatic ducts, increased permeability pancreatic duct due to hypercalcemia and apparent direct toxic effect of PTH on pancreas.9,11 Parathyroid carcinoma is a rare cause of primary hyperparathyroidism, accounting for less than 1% of cases.2 The major clinical presentations of parathyroid carcinoma are hypercalcemia, neck mass, bone disease, and renal disease.2 But, pancreatitis as a symptom of hyperparathyroidism is rare, and the occurrence in patients with parathyroid carcinoma is unusual, ranging from 0% to 15%.12,13 No single laboratory finding can be use as diagnostic for parathyroid carcinoma, but certain findings may offer clues that should be included as part of the differential diagnosis in patients presenting with primary PHPT. The first, is the mean serum calcium in parathyroid cancer patients is usually reported level greater than 14mg/dl and the second that the intact PTH levels are on average 5-10times upper limit of the normal range; however, no maximum level for malignancy has yet been defined.12 In our patient, the serum calcium was 13,4mg/dl (8,4-10,2mg/dl), intact parathormone was 462pg/ml (10-65pg/ml), TC 99mTc-Sestamibi SPECT Scan and ultrasound of the neck, were consistent with a parathyroid tumor, and therefore, a CT scan was performed. The results of anatomic imaging demonstrated the presence of an infiltrative neck mass over the left inferior thyroid, which is very typical of potencial parathyroid cancer. Although parathyroid carcinomas are slow-growing neoplasms, they have a high propensity to reappear locally and metastasizes through both lymphatic and haematogenous routes.2 Complete en bloc resection of the parathyroid carcinoma including central neck dissection and adjacent thyroid gland at the time of initial surgery provided the best chance for cure and reduced the recurrence of the disease.13 If there should be any evidence of invasion of the strap muscles or other structures, the tissues should olso be removed in continuity with the tumor. In most cases, the recurrent laryngeal nerve can be preserved without exposing its integrity.12 However, if the nerve is involved, it should be removed.2,14 In a previous study, a prophylactic lateral neck dissection was performed previously and but did not improve survival, and instead resulted in increased morbidity.15 After initial surgery, if the calcium and PTH levels are within normal limits and the pathology has no evidence of extensive vascular or capsular invasion, it usually advised to follow the patient closely without an attempt at immediate re-excision. Additionally radiation therapy is not indicated, as this type of tumor is not radiosensitive.12 Due to, the rarity of parathyroid cancer, few investigators have sufficient numbers of patients to allow the execution of a large scale clinical experimental. Attempts to manage the tumor with chemotherapy have not provided positive outcomes.15 In some cases, patients who received adjuvant radiation therapy for microscopic residual disease have been followed for 12-156months without recurrences.16
The hypercalcemia-related acute pancreatitis is uncommon, and primary hyperparathyroidism should be suspected in patients with laboratory results.2 Higher calcium levels greater than 14mg/dl and intact PTH levels on average 5-10times upper limit of the normal range are diagnostic of parathyroid cancer.12 Anatomic imaging including ultrasound, Tc-99m-sestamibi SPECT and TC scan are useful localizing studies, in patients suffering primary hyperparathyroidism.2,6 Block resection of all involved tissue, central neck dissection and lobectomy of thyroid is the appropriate initial surgical treatment in all suspected cases of parathyroid carcinoma.13 There is currently insufficient evidence for postoperative radiotherapy to be routinely administrated in patients with microscopy residual disease.12
None.
Author declares that there is no conflict of interest.

©2017 Cadena, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.