eISSN: 2471-0016


Research Article Volume 2 Issue 4
1Centre for Bioinformatics and Systems Biology, University of Khartoum, Sudan
1Centre for Bioinformatics and Systems Biology, University of Khartoum, Sudan
Correspondence: Faisal M. Fadlelmola, Centre for Bioinformatics and Systems Biology, Faculty of Science, University of Khartoum, University Avenue, P.O. Box 321, Khartoum, Sudan
Received: January 01, 1971 | Published: June 27, 2016
Citation: Fadlelmola FM. Cancer registries and cancer genomics research in east africa: challenges and lessons learned. Int Clin Pathol J. 2016;2(4):67–76. DOI: 10.15406/icpjl.2016.02.00045
Policy makers and governments often pay little attention to support cancer registries and cancer research in Africa and mainly in East Africa. This paper demonstrates that an updated cancer registry data could be one of the main factors to control and treat cancer cases. The approach of the paper is situated in the broader studies of cancer registry and epidemiology and its effects on cancer control and treatment. The paper also shows why the findings of this study are significant. The paper makes recommendations that will hopefully help policy makers in understanding the problems and obstacles facing cancer registries and cancer genomics research in East Africa. The current study conducted a field research survey to assess the cancer registries, cancer epidemiology and cancer genomics research capabilities in five East African countries including Ethiopia, Eritrea, Sudan, Uganda and Kenya. Uganda and Kenya were included as cancer registry controls in order to compare the best practices and lessons learnt from the existing cancer registries. This will facilitate the formulation of appropriate policies and recommendations for improved cancer care and prevention in this region. The current study provided the baseline information for conducting cancer genome analyses in the near future in this region. The study also addressed the challenges facing these countries to have up-to-date cancer registries. The study adopted questionnaire and interviewing approach to conduct the field research survey. The questionnaire assessed the cancer registries, cancer epidemiology and cancer genomics research capabilities in these countries.
Keywords: cancer, registry, epidemiology, genomics, polymorphism, germ line mutation, genetic, HPV, HIV, Human immunodeficiency virus, HBV, Hepatitis B viruses, Human papillomavirus
HPV, human papillomavirus; HBV, hepatitis B viruses; HIV, human immunodeficiency virus; HHV8, human herpesvirus-8; IARC, international agency for research on cancer; KCR, kampala cancer registry; EARN, east african registry; INCTR, international network for cancer treatment and research; UICC, international union against cancer; NIH, national institutes of health; NCI, national cancer institute; KNH, kenyatta national hospital; WHO, world health organization; HMIS, health management information system
Cancer is one of the leading causes of morbidity and mortality worldwide, with an estimated 12.7million new cases and 7.6million deaths in 2008.1 With over 7million new cases- often detected at a later stage- and 4.8million deaths, the developing world is bearing over half of this burden but is the least equipped to cope with this situation. Due to the increase in the global population and as an effect of ageing, it is predicted that by 2030 the number of new cancer cases will increase to more than 21million, and deaths to 13million.1 In the absence of cancer planning and control interventions, around 70% of the global cancer burden will arise in the developing world.1
The non-communicable diseases, such as cancers, are emerging health problems that need to be dealt with appropriately to sustain public health advances that have already been achieved. Increases in the prevalence of tobacco consumption and immune-suppression induced by the human immunodeficiency virus (HIV), coupled with such existing risk factors for cancer as alcohol; the high prevalence of cancer-associated infectious agents like human papillomavirus (HPV), hepatitis B viruses (HBV), and human herpesvirus-8 (HHV8); and environmental exposure to toxins, such as aflatoxins, will have an important impact on future cancer patterns and incidence.2 Even despite declining overall life expectancy as a result of the HIV epidemic, Africans will continue to age, which will contribute to cancer's becoming an increased burden on health services, both in relative and absolute terms.
In the past, studies have suggested that some sections of the population may have been underrepresented in hospital statistics, particularly older women and young men, both of whom were more likely to return to their rural homes to seek care.3 However, currently, this underrepresentation is probably rather rare in contemporary urban Africa. Most cancer patients will, eventually, seek medical assistance, although often at an advanced stage of disease. The situation in rural areas may be quite different, but almost all the present-day cancer registries are located in urban centers. From an epidemiological point of view, one must guess at how well the cancer profile from the urban areas reflects that in the country as a whole, given what is known of urban–rural differences in cancer patterns in other areas of the world. The International Agency for Research on Cancer (IARC) has published the available data on cancer incidence and other cancer data from a variety of sources.4 Such data have also been used to prepare a set of estimates of incidence and mortality at the national level for the year 2002.5
Data on cancer patterns in Africa are sparse, but the considerable effort which has gone into fostering the development of population-based cancer registration in the continent is now bearing fruit. It will only be possible for a minority of African registries to achieve publication in Cancer Incidence in Five Continents due to the circumstances in which they work, with poor medical infrastructure and limited access to diagnostic services, medical and vital records and population denominators. Nonetheless, the information they were producing gives a unique insight into cancer patterns on the continent. It was decided to prepare a publication at IARC to include results from the cancer registries, published case-series or incidence data from the literature, and a comprehensive review of cancer occurrence for selected sites and for the different regions in Africa. Mokhtar Hamdi-Chérif (Algeria), Freddy Sitas (South Africa) and Henry Wabinga (Uganda), Ebrima Bah (The Gambia) are representing cancer registries in the North, South, East and West of the Africa continent among the editors. Data from over 20 cancer registries in Africa were analyzed and tables of incidence or relative frequency prepared. A recent Cancer Incidence in Five Continents, Volume IX was published in 2007.6 The nine volumes of Cancer Incidence in Five Continents now cover a period of approximately forty years. With the rapidly rising cancer burden in low-income and medium-income countries, more high-quality incidence data are needed from regions and countries in such settings.
This paper will discuss the current state of cancer registries in Eastern Africa. We also propose how cancer registries, cancer epidemiology and genomics problems could be addressed in the region by focusing on specific critical points. The paper is organized as follows: The section following this introduction addresses the research objectives. This followed by the research methodology. The section that follows situates the paper in the broader literature review and studies on cancer registration and research. The next section focuses on findings of the current research, explaining why the findings of this research are significant. This is followed by a discussion of cancer treatment and research, human resources and cancer genomics research capacity. The next section explains the policy implication of the research findings. The paper closes with the conclusions drawn from the research and includes recommendations that will aid policy makers in understanding the current problems and obstacles facing cancer registration and research in the East Africa. The findings will assist them in developing policies to address the problem in a sustainable way. The research was conducted as part of the Africa Initiative within the Centre for International Governance Innovation.
A field research survey was conducted to assess the cancer registries, cancer epidemiology and cancer genomics capabilities in three East African countries (Ethiopia, Eritrea, and Sudan). Two countries from the same region, Uganda and Kenya, were included to be used as controls in order to compare the best practices and lessons learnt from the existing cancer registries. The objectives of the current study were as follow: (1) to conduct a field research to assess the cancer registries in five East African countries (Ethiopia, Eritrea, Sudan, Uganda and Kenya); (2) to conduct a field research to assess the cancer epidemiology in urban areas of these five countries; (3) to conduct a field research to assess the cancer genomics research capabilities in these five countries; and (4) to write a research completion report in the form of: (a) discussion paper of key findings of the research; (b) policy brief outlining recommendations that the decision makers in these countries shall follow to improve and enhance cancer registry, cancer epidemiology and cancer genomics research in these countries.
The research sites were the capital cities of the five studied countries: Addis Ababa, Kampala, Kenya, Asmara and Khartoum. The duration of the entire field research was 40days. In addition, data analysis and report writing and dissemination need took roughly between 2-3months. The overall duration of the study was five months.
Research methodology
The current study adopted questionnaire and in-depth interviewing approach to conduct the field research. In-depth interviewing, also known as unstructured interviewing, is a type of interview which the author used to elicit information in order to achieve a holistic understanding of the interviewee’s point of view about cancer registry in his/her country; it can also be used to explore interesting areas for further investigation. This type of interview involves asking informants open-ended questions, and probing wherever necessary to obtain data deemed useful by the author. As in-depth interviewing often involves qualitative data, it is also called qualitative interviewing.
A cancer registry and cancer epidemiology questionnaire was sent to the Ministry of Health and/or to the directors of cancer registries in these countries. The author proposed to start the field visit after 4-5weeks from sending the questionnaire, but this method was found impossible because in most cases nobody responded unless you physically visited the responsible key personnel at the Ministries of Health and the existing cancer registrars in their countries. The objective of the field visit was to further assess the situation on the ground as well as to meet and interview key personnel at the Ministry of Health and the existing cancer registrars, cancer epidemiologists and molecular geneticists. The author spent 10-18days in each of the five countries. The questionnaire also assessed cancer genomics capacity of each country through requesting information about availability of molecular laboratory facilities and qualified staff to carry out cancer genome analyses.
A review of relevant policy and literature
There are few cancer registries in sub-Saharan Africa and most of them are hospital-based. Data from these registries indicate some consistency in the pattern of malignant diseases in most countries within the region with slight local variation.7 Carcinoma of the prostate, liver, Non-Hodgkin’s lymphoma and colon and rectal tumours are the top malignant diseases in the Ibadan cancer registry while Kaposi’s sarcoma, liver and oesophageal cancers are the most common in some registries in East Africa.7 At both the national and community level, cancer registration schemes are central to research into the nature and causation of cancer, to the planning of health service resources and cancer control programs, and to the assessment of their efficacy. Cancer registration is thus part of a modern health information system in the developed countries. Other sources of data available to measure levels of cancer in a community include hospital registry data as well as special patient series based on, for example, pathology records and autopsies. While interesting information on cancer patterns has been derived from such data collections, they are necessarily incomplete and may represent a selective and biased sample of the patient population.8 An accurate picture of the cancer burden depends on the creation of a population-based cancer registry (PBCR). The role of the cancer registry in developing countries must not be underestimated. Many developing countries have very young populations, with over 40% of the total under 15years old and less than 5% aged 65years or more.9
Cancer has, in the past, been neglected as a cause of death and disability. However, with increasing numbers of elderly people, and declining relative importance of infectious diseases, this situation is likely to change. The cancer registry represents an effective and relatively economic method of providing information for the planning of cancer control measures. Cancer registration may be defined as the process of continuing, systematic collection of data on the occurrence and characteristics of reportable neoplasm with the purpose of helping to assess and control the impact of malignancies on the community. The cancer registry is the office or institution which attempts to collect, store, analyze and interpret data on persons with cancer. The synonym 'tumor registry' is often used, in particular in the United States of America, and this term may often be more appropriate, since most cancer registries include the registration of a number of benign tumors or conditions, e.g., urinary tract papilloma and brain tumors. The term cancer register denotes the file or index in which the cancer registry holds its tumor cases. Although the means of recording cases may to a large extent be identical, a distinction must be made between the population-based cancer registry and the hospital registry. The population-based cancer registry records all new cases in a defined population, most frequently a geographical area, with the emphasis on epidemiology and public health. The hospital-based cancer registry records all cases in a given hospital, usually without knowledge of the background population; the emphasis is on clinical care and hospital administration. The hospital registry may form the nucleus for a population-based cancer registration scheme.
A population-based cancer registry tissue repository can be used to measure the allele frequency of a genetic polymorphism or germ line mutation, such as BRCA1, in cancers diagnosed in a particular ethnic group or community.10 Novel genes or protein targets that will be used for therapeutic or diagnostic purposes need to be validated in large, population-based tissue samples.11 Investigators can be more assured that the frequency of the characteristic under study is unbiased and provides a truer picture of the prevalence of a risk factor or biologic marker in the cancer population. These data are critical to determining the predictive value of a genetic test or the use of a biologic marker as a diagnostic tool. To establish an objective measure of a laboratory or cancer screening test, the validity and reproducibility of the test must be evaluated and definitively established.
Cancer registry history in the studied countries
The Kampala cancer registry (KCR) was established in 1954 as a population-based cancer registry at the department of pathology, Makerere University Medical School (Table 1). Nairobi Cancer Registry (NCR) was established in the year 2001 as a population-based cancer registry (Table 2). In Sudan, Cancer Registry was established in 1960s and for unknown reasons it was stopped in late 1980s. In 2009 an initiative was made to re-establish the National Cancer Registry in Khartoum as a population-based cancer registry. The Gezira Cancer Registry in Sudan was established in July 2007 to cover the Gezira Province (Table 2). The Addis Ababa Cancer Registry was established in 2011. Currently there is no cancer registry in Eritrea. As shown in Table 2, only KCR and NCR are members of East African Registry Network (EARN) and International Association for Cancer Registries (IACR). In addition, both KCR and NCR established international partnership and cooperation in cancer research with the following: International Network for Cancer Treatment and Research (INCTR), International Agency for Research on Cancer (IARC), National Cancer Institute/National Institutes of Health (NCI/NIH), and the International Union Against Cancer (UICC). On the other hand, Sudan, Ethiopia and Eritrea need to establish a solid network and collaborations with EARN and IACR as well as other relevant regional and international partners working to fight and treat cancer.
Country |
Population (Million)* |
Area(Square Kilometers) |
Annual Population Growth Rate (%) |
Health Expenditures (% of GDP)* |
Uganda |
33.61 |
236,580 |
3.58 |
8.2 |
Kenya |
41.07 |
580,367 |
2.46 |
12.2 |
Ethiopia |
90.87 |
1,104,300 |
3.19 |
3.6 |
Eritrea |
5.93 |
117,600 |
2.47 |
7 |
Sudan |
33.4 |
1,881000** |
2.48 |
7.3 |
Table 1 Basic Demographic Information.
*(Central Intelligence Agency (US) 2009).
**This is the area of Sudan after the South Sudan cessation in July 2011.
Country |
Cancer Registry |
Date of Establishment |
Hospital or Population Based Cancer Registry |
Member of EARN** |
Member of IACR*** |
Ethiopia |
Yes |
2011 |
Population-based |
Yes |
No |
Eritrea |
No |
NA |
NA |
No |
No |
Kenya |
Yes |
2001 |
Population-based |
Yes |
Yes |
Sudan |
Yes |
2009 (1994; 2007)* |
Population-based |
No |
No |
Uganda |
Yes |
1954 |
Population-based |
Yes |
Yes |
Table 2 Cancer Registry History in the five studied countries.
Screening cancer programs
There are no population-based large scale cancer screening programs running in the five studied countries as shown in Table 3. However, cluster screening study of cervical cancer was carried out in Eritrea with support of Italian donors. In Kenya a satellite-based cervical screening cancer was conducted with financial support from donors, individuals and private sector. In Uganda, there is an effort to undertake screening programs for cancer of cervix and breast. In Sudan, breast cancer screening was done in a limited area of Gezira state (Table 3).
Country |
Cancer screening |
Type of cancer Screening |
Funding sources |
Ethiopia |
No |
NA |
NA |
Eritrea |
Cluster |
Cervical cancer |
Italian donors |
Kenya |
Satellite-based |
Cervical cancer |
Donors, Individuals & private Sector |
Sudan |
Limited area of Gezira state |
Breast Cancer |
NA |
Uganda |
No |
NA |
NA |
Table 3 Screening programs in the current studied countries.
An overview of cancer registries in the studied East African countries
Cancer registries are usually involved in calculating incidence rates for entire populations, and the denominator for such rates cannot be derived from knowledge of each individual's contribution to the population at risk. This is therefore generally approximated by the mid-year population (or the average of the population at the beginning and end of the year or period), which is obtained from a census department. The variance of the estimate of the incidence rate is determined by the number of cases used in the numerator of the rate; for this reason it is usual to accumulate several years of observation, and to calculate the average annual rate. The denominator in such cases is again estimated as person-years, ideally by summing up the mid-year population estimates for each of the years under consideration. When these are unavailable, the less accurate solution of using the population size from one or two points during the time period to estimate person-years has to be used, an approximation that is likely to be reasonable providing no rapid or irregular changes in population structure are taking place. Conventionally, incidence rates of cancer are expressed as cases per 100 000 person-years, since this avoids the use of small decimals. For childhood cancers, the incidence rate is often expressed per million.
Kampala cancer registry
The Kampala cancer registry was established in 1954 as a population-based cancer registry at the department of pathology, Makerere University Medical School, to obtain information on cancer occurrence in Kyadondo County.12 It contributed data to the quinquennial IARC publication Cancer Incidence in Five Continents in volumes I, VII and VIII13 and cancer survival data for Kampala had been published.5 Cancer is not a notifiable disease, and registration of cases is done by active methods. The principal sources of data are medical records in the hospitals in the government and non-government sectors, pathology laboratories and hospice. The registry caters to a population of about 1.1 million in 1995 with a sex ratio of 1029 females to 1000 males. The average annual age-standardized incidence rate is 162 per 100 000 among males and 171 per 100 000 among females in 1993-1997. The top-ranking cancers among males are Kaposi sarcoma, cancer of the prostate and non-Hodgkin lymphoma. Among females, the order is Kaposi sarcoma, cervix and breast in 1993-1997.
The registry contributed data on survival from 15 cancer sites or types for the first time in this volume of the IARC publication on Cancer Survival in Africa, Asia, the Caribbean and Central America. For Kaposi sarcoma, only a random sample of the total incident cases (431 out of 1376 cases; 31%) was available for this survival study. There is evidence that the cancer burden and pattern in Uganda may be different in different parts of the country as exemplified by Templeton (1973) who found stomach cancer more common in Nkole while Burkitt lymphoma was more common in West Nile. More recently Wabinga (2002) found stomach cancer the second commonest male cancer in Mbarara region while in Kyaddondo County it is the fifth commonest cancer.
Procedure for establishing regional cancer registries: The health delivery system of Uganda consists of village health committees; Health Centers II, III and IV plus district, regional and two National Referral Hospitals. Health Centre IV has a laboratory and in most cases is managed by a medical doctor. District hospitals undertake operational procedures in addition to follow up of cancer patients. Regional hospitals have consultants including Histopathologist where confirmation of cancer is made. It is anticipated that patients with cancer will at least seek assistance from Health Centre IV and above where cancer will be diagnosed. It has also been found that patients with cancer residing around the regional hospital will more likely seek treatment from these health units that those residing far from these facilities. It is for this reason that PBCR should be established around these regional hospitals. The ideal population to be covered by a PBCR is estimated to be around 1-5 million people and therefore if three more registries are established this will be covering an approximate 2/3 of the entire population. It is therefore expected that for the following regional registries the coverage should be as follows: (1) Mbarara Cancer Registry covering the whole of Mbarara, Bushenyi and Ntungamo region; (2) Gulu Cancer Registry should cover the districts of Gulu and Amuru; (3) Mbale Cancer Registry should cover the districts of Mbale, Kumi, Butaleja, Tororo and Manafwa.
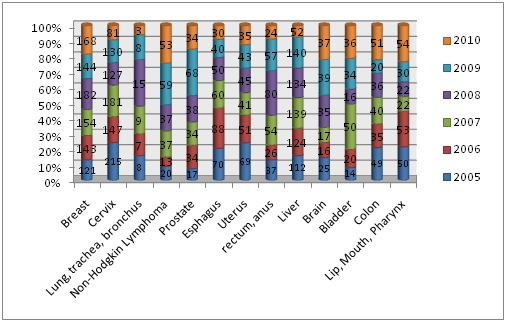
Limitations and challenges: There has been a general upward trend in cancer incidence in Uganda since the establishment of a cancer registry in Uganda (1954) with some cancers such as breast and prostate cancer trebling in incidence rate. There are other cancers such as liver which have remained stable over years while some cancers such as Kaposi’s sarcoma and non-Hodgkin’s Lymphoma suddenly increased in incidence in the era of HIV/AIDS pandemic. There are a few cancers such as penile and urinary bladder cancer on a downward trend. The data on cancer shown in this paper (Figures 1-3) is obtained from Kampala Cancer Registry, a population-based cancer registry, covering only 10% of Ugandan population. The challenge is that these data may not exactly represent the remaining 90% of the population. Therefore, there is an urgent need to establish regional cancer registries. Another challenge is the diagnostic capabilities of diagnosing cancer in terms of human resource and equipment since with current management of cancer there is need to invest in molecular techniques of diagnosing various types of cancer. There is also a challenge in establishing cancer prevention and control policies and programs. Currently there are no established screening programs for common cancer in Uganda and therefore patients present late in health units.
The Director of Kampala Cancer Registry anticipates cancer to be one of the major causes of morbidity and mortality in the Ugandan population in the future, and therefore determining the trends and monitoring cancer control programs is the major task to be undertaken and PBCR is one of the tools available for that purpose.12
Nairobi Cancer Registry: Nairobi Cancer Registry (NCR) was established in the year 2001 after consultations between the National Cancer Institute (NCI), Office of International Affairs, and International Agency for Research on Cancer (IARC), Ministry of Health (MOH) and Kenya Medical Research Institute (KEMRI). It is situated at the Centre for Clinical Research (CCR), KEMRI Headquarters, in Nairobi. The registry started with a skeleton staff comprising Dr. Mutuma G.Z., a consultant pathologist assisted by Mrs. Ann Korir as the supervisor and Mrs. Catherine Ogeto as data entry clerk. Staff from various institutions were later recruited and trained as cancer registrars to carry out cancer case abstraction and registration. Their primary duty in the registry work is to abstract cases from various sources and submits them to the cancer registry office at KEMRI. The cancer registrars were selected from staff already working in medical records service, laboratory and clinical services. The registrars were recruited from KEMRI, MOH, Kenyatta National Hospital (KNH), and University of Nairobi and from a few private hospitals in Nairobi. Training of the registrars was done by KEMRI in collaboration with IARC, World Health Organization (WHO), MOH and the National Cancer Institute (NCI) of the United States of America (USA). The trained registrars started collecting data on all newly diagnosed cancer cases from the year 2000 in their respective hospitals, laboratories and radiotherapy units. The data was submitted to the registry supervisor for verification and subsequent entry into a computer. The use of CanReg4 software, has allowed for checks on accuracy, duplication and satisfactory completion of the submitted cancer abstract forms.
The mission and vision of the NCR is to meet the highest attainable international standards in cancer registration, surveillance and control. The main objectives of NCR are: (1) to establish and maintain, a population based cancer registry for Nairobi cosmopolitan; (2) to develop a National Cancer Registry through the establishment of regional registries; (3) to determine the burden and trends of cancer occurrence in Kenya using Nairobi as a representative; (4) to disseminate information on patterns of cancer occurrence in Kenya and participate in National Cancer Control Programs; (5) to provide quality and reliable cancer data to the Ministry of Health and other health-care providers, educators and planners for effective service delivery; (6) to avail cancer data for research in epidemiological studies, clinical management, prevention and other related programs; (7) to liaise with other local and international cancer organizations on cancer research, prevention, control and surveillance; and (8) to advocate for policy frameworks that provide support and contribute to effective cancer control and prevention programs.
Members of staff of the NCR have benefited from various trainings relevant to the registration and reporting of cancer cases. This has been made possible through training sessions both locally and internationally. During the 2000-2002 periods, breast cancer was the most frequent cancer among females, closely followed by cancer of the cervix uteri (Figure 4). On the other hand, cancers of the head & neck followed by esophagus and prostate, lead in frequency among males (Figure 4). The pattern of most common cancers varied slightly when one compares single years in the report period. However it is worth noting that cancers of the breast and cervix uteri comprise a large proportion (43.3%) of all reported cases (Figure 4). Given the magnitude of incomplete cases and the issue of residence, NCR has not calculated incidence rates. Cases mentioned in Figure 4 in this paper are relative frequencies or percentages.
Cancer of the esophagus (10.0 %) was first in single organ cancers among males. This was closely followed by cancer of the prostate (9.4%), stomach (7.1%), Kaposi’s sarcoma (6.9%), and liver (5.7%). The other major cancers reported among men in Nairobi were non-Hodgkin’s Lymphoma (4.2%), skin (3.7%) and colon 3.4% (Figure 4). Head and Neck group of cancers made up large proportion comprising 14.8% of male cancers (Figure 4). This trend is reflected in the single years for the same period. The most common cancer reported among women was breast (23.3%), followed by cervix uteri (20.0%), esophagus (4.4%) and stomach (3.8%). The other major cancers registered among women were ovary (3.3%), skin (2.6%), Kaposi’s sarcoma (2.4%), Non-Hodgkin’s Lymphoma (2.4%), mouth (2.3%) and rectum (2.2%). Head and neck group of cancers accounted for 7.2% of all cancers in women
Limitations and challenges
The Nairobi Cancer Registry records instances from the Nairobi region. It was established in 2001. The government does not provide funding to the registry and the registry. It relies entirely on donor funding. Sustainability is a big challenge. Resources, both human and financial, are key issues that affect the registry. There is high turnover of staff since no salary is provided to them except transport allowances. Nairobi is the capital city with a population of 3.2 million people yet Kenya has 41 million. The burden of cancer in the wider country is not known since there is no National Cancer Registry. To overcome these problems, the following are possible solutions: there is need to support the cancer registry by providing financial support for that goal; training of cancer registrars, statisticians and epidemiologists would boost registry work in Africa. Cancer is a burden in Kenya. Cervical cancer is one of the most preventable cancers yet women die of it every day. Organized screening programs and education of communities to curb barriers associated with cultural beliefs are required. Commitment by government is needed for all these issues. The registry uses the International Classification of Diseases for Oncology (ICDO) third edition, for coding the primary site, histology, behavior, and grade of cancer. Demographic data is captured using a format, which was prepared for coding residence, place of birth, ethnic group (tribe), hospital/facility of diagnosis along with the other common socio-demographic variables.
Large parts of the data from NCR have been presented in Tables. These show both cumulative and single year figures for the three year period of males and females, cancer site occurrence, age distribution and percentages of the most common cancers as well as all registered cases. The ICD-10 format of presentation has been adopted, as this is the standard format that will facilitate comparisons with results from most registries in Africa and other parts of the world. In-situ tumors have been excluded from this report. During the three-year period under review, a total of 3310 cases were registered in NCR, consisting of 1511 (45.6%) male and 1799 (54.3%) female. 213 (6.4%) of these cases were children aged 0 to 14 years.
Addis Ababa cancer registry
Prior to the establishment of a cancer registry in Ethiopia in 2011, extrapolation from clinical records from Tikur Anbessa Radiotherapy Center estimates that there are 120,500 new cancer cases per year; although Globocan estimates are much lower (51,000 per year). Most patients present with advanced disease, and there is a high rate of abandonment of treatment. The top 10 cancers are: Cervix, Breast, Head & Neck, Sarcoma, Leukemia/Lymphoma, Colorectal, Kaposi Sarcoma, Skin, Bladder, and Esophagus.
The efforts to establish the Addis Ababa Cancer Registry started during the period of 2009-2011. The East African Cancer Registry Network,14 part of INCTR's Cancer Registry Program, organized a three-weeks training course for staff of two new cancer registries: Addis Ababa (Ethiopia) and Dar es Salaam (Tanzania) in Kampala, along with Nairobi Cancer Registry during September/October 2011. The course included the basics of tumor pathology, classification and coding, and the principles of cancer registration (case finding, abstracting, coding and data entry). The participants also received an introduction to the cancer registry software (CANREG-5) which will be installed in their registries. The faculty members were Professor Henry Wabinga and Ms Sarah Nambooze (Kampala), Ms. Anne Korir (Nairobi) and Ms Cecile Ingabire (Rwanda), assisted by junior registry staff in Kampala and Nairobi.15
Asmara cancer registry
Currently there is no cancer registry in Eritrea. Efforts to establish a working group for the formation of cancer prevention and control policy guideline started in May 2011. To date there is no comprehensive study about cancer epidemiology in Eritrea. The information concerning cancer available is from hospital registries and Health Management Information System (HMIS), and probably the information from these resources is not representative of real magnitude of the problem. The problems and challenges of cancer profile epidemiology in Eritrea are: (1) there has been no nationwide study, mainly due to shortage of resources; (2) since there are other life-threatening diseases that have higher prevalence than cancer, it is not a top priority; and (3) lack of adequate trained staff to carry out the task. These challenges could be solved by increasing awareness and highlighting the importance of cancer prevention programs by the Eritrean government. In addition, support of partners could help in training of the human resources required for this task: to improve the awareness about cancer in schools, universities and local communities with the help of non-governmental civil organizations and the media so that it can be considered as a disease and to be given top priority especially by policy makers, because it is far easier and more cost effective to prevent and control cancer than to treat.
The immediate priority for the Eritrean health system is to train 4-6 staff on the principles and methods of cancer registration as soon as possible with the financial support of international donors and then to ensure that adequate finding, abstraction and coding of the cancer cases in the country are recorded and a mechanism of follow-up is established. Figure 5 shows the current reported cancer cases in the Eritrean Health care facilities from year 2005 to 2010 for both sexes and all ages. Data cannot yet be presented by sex and age groups, although in the relevant files the author witnessed at the central pathology laboratory, all these data are almost there, they just need to be abstracted, coded and entered into program to be analyzed. The second priority is to launch nationwide surveys of different cancer types in order to study the magnitude, prevalence, incidence, morbidity and mortality. This can be phased in by firstly establishing a cancer registry at the capital Asmara which could be called the Asmara Cancer Registry and then expanding it nationwide.
Cancer Registry in Sudan
National cancer registry: In 2009, the Sudanese Federal Ministry of Health established a population-based cancer registry, the Sudan National Cancer Registry.16 The incidence of cancer in Sudan seems to be on rise. After the establishment of the cancer registry, the number of cancer cases detected doubled by active and passive case finding, from 5000 in 2008 hospital-based registry to 10,000 in 2009 National Population-based Cancer Registry data. The increase may be due to an increase in reporting or due to increased awareness to presentation to hospital in Khartoum. In the few coming years the reason will be clear if the cancer registration expands and includes all other states. The problem in Sudan is that all the diagnostic laboratory and cancer treatment centers were located in the capital and central, but many cases cannot reach these centers due to the lack of affordability, stigma and distance from the capital. Furthermore, most of the activities for the prevention of the disease (by Universities and some civil society organizations) take place in the capital, Khartoum State, leading to lack of cancer awareness and importance of early presentation to hospital elsewhere. Moreover, cancer registration seems to be not an important issue for medical oncologists.
Data collection is active and passive case finding, software for data entry is CANREG5 and data analysis is done using Excel, GIS, and SPSS software. Data are firstly checked for completeness and accuracy before entered into the system. The most efficient solutions for the above-mentioned problems could be through the following means: (1) establishment of regional diagnostics labs. and treatment centers in three regions of the Sudan (East, West, and North); (2) expansion in the training in the field of oncology nursing and medical oncology; (3) functioning control programs; (4) expansion in cancer registration in other states; (5) notification by law of the new cancer cases; (6) expansion in the training in cancer epidemiology; (7) funds for cancer data collection.
Gezira Cancer Registry
The National Cancer Institute, University of Gezira (NCI-UG), is a special center established in 1994 by the University of Gezira (UG) in Wad Medani, Sudan. UG is a community oriented University established in 1975, with a main objective of rural development. UG is located in the center of Sudan in Gezira state, the most densely populated state, which harbors the Blue Nile-irrigated Gezira Scheme. NCI-UG was established to meet the community’s needs in the fields of Oncology, Nuclear Medicine, Medical Imaging and Molecular Biology, integrating activities of research, service and training. The uniqueness of the approach of NCI-UG in implementing these complementary functions made the institute’s environment quite satisfactory in providing medical services, good quality research, and training programs.17 NCI-UG with the support of the International Agency for Research on Cancer (IARC), established in 2006 the Gezira Cancer Registry, the first population-based cancer registry in the country. The Gezira Cancer Registry, located at the NCI-UG in Wad Medani, the capital city of Gezira State, covers only Gezira State (Central Sudan, 26,075 km2), serving about four million people (10% of the total Sudanese population). Figures 6-8 detail the most common male, female and pediatric cancers in Central Sudan respectively.
Resources to manage the significant burden of cancer are limited in East Africa. For example, in Kenya there are six Medical Oncologists and 15 Cancer Pathologists and most likely they are concentrated around the capital Nairobi (Table 4). In Sudan, there is one cancer epidemiologist, 25 Medical Oncologists; 40 Cancer Pathologists, four cancer genomics and genetics experts, one Bioinformatician and two Cancer Biostatisticians (Table 4). In Uganda there is one cancer epidemiologist, two Medical Oncologists; 13 Cancer Pathologists and two Cancer Biostatisticians. As shown in Table 4, in Eritrea there is only one radiation oncologist who just returned from training in Italy, whereas no data are available for Ethiopia because they didn’t fill out the questionnaire. These human resources are extremely limited compared to actual need. For perspective, in Canada, a radiation oncologist would typically see 250 new patients per year.18
Fields |
Eritrea |
Ethiopia |
Kenya |
Sudan |
Uganda |
Cancer Epidemiology |
NIL |
NA |
NA |
1 |
1 |
Medical Oncology |
1 (radiation oncologist) |
NA |
6 |
25 |
2 |
Cancer Pathology |
NIL |
NA |
15 |
40 |
13 |
Cancer Genomics/ Genetics |
NIL |
NA |
NIL |
4 |
NIL |
Cancer Biostatistics |
NIL |
NA |
NA |
2 |
3 |
Bioinformatics |
NIL |
NA |
NA |
1 |
NIL |
Genomics/Genetics (not cancer related) |
NIL |
NA |
NA |
9 |
1 |
Table 4 Number of experts in cancer treatment & research in the studied countries.
NIL=0; NA= no data
Only Kenya and Sudan have full capacity for conducting cancer genomics research. Both countries have research institutions that are equipped with the state-of-art laboratories. The Biosciences Eastern and Central Africa (BecA) Hub Genomics and Bioinformatics Platforms in Kenya is equipped with both capillary (ABI 3130xl, ABI 3730xl and ABI 3500xl) and second-generation sequencing facilities (one 454 GSFLX™ Titanium pyrosequencer) platform, which will allow East African researchers to perform low, medium and high throughput sequencing (for partial genomes, full genomes and metagenomes) and genotyping activities. BecA maintains the latest copies of all major sequence databases that can be accessed.
Research is a key factor in promoting health, fighting disease, reducing disability and improving quality of care. Cancer research is an essential component in the development, implementation and evaluation of a national cancer control program. A scientific basis for identifying the causes of cancer and for specifying effective strategies for the prevention, treatment and control of cancer, as well as for evaluating overall program, depend on cancer research. The scope of cancer research should be wide, extending over a number of key areas such: (1) epidemiological research and the distribution and determinants of cancer in different materials; (2) prevention research, which encompasses research into health promotion and education, screening and other early detection methods; (3) laboratory research, cell and molecular biology, genomics of cancer research; (4) translational research, which is concerned with the integration of bench and clinical research for the benefits of cancer patients and those at risk of cancer; (5) clinical research, the study of natural history of the cancer process and the assessment of efficacy and toxicity of treatment; (6) health services research, which is a wide-ranging, multidisciplinary field that the structure, processes and effects of health care services for cancer. Universities and training institutions should have a role in supervision and executing the above-mentioned scope of cancer research.
Policy Implications of findings
Cancer is the leading cause of death in developed countries and the second leading cause of death in developing countries.19 The burden of cancer is increasing in developing countries as a result of population aging and growth as well as, increasingly, an adoption of cancer-associated lifestyle choices including smoking, physical inactivity, and ‘‘westernized’’ diets. Incidence data, the number of newly diagnosed cases each year, are derived from population-based cancer registries, which may cover entire national populations but more often cover smaller, sub national areas, and, particularly in developing countries, only urban environments, such as major cities. Although the quality of information from most of the developing countries might be considered, in relative terms, of limited quality, it often remains the only source of information available on the profile of cancer and as such provides valuable information. The total numbers of cancer deaths by country are collected annually and are made available by the WHO.20
The incidence of malignant diseases is increasing globally, particularly in the developing countries as shown by recent cancer statistics from the World Health Organization Reports. It is anticipated that with increase in life expectancy consequent upon improved standard of living and increasing industrialization, the burden of cancer in sub-Saharan Africa is likely to increase in the new millennium. Cancer registries routinely provide quality data on the incidence and prevalence of cancer in a population, on the common types of cancer reported and their trends. This allows for effective planning of prevention measures, which include screening programs and cost effective cancer management. Cancer registry data collected from a given population can also be used in research programs and for comparisons with other populations in different regions of the world. The burden of cervical cancer in East Africa is extremely high, where the costs of nationwide organized cytology screening have been a significant limitation. The use of Pap testing for cytology-based screening has been highly effective in preventing cervical cancer in developed countries and will most likely be effective in countries where screening is limited or nonexistent.21 Hence, the use of alternative screening modalities, such as visual inspection of the cervix aided by acetic acid (VIA) with or without magnification, is currently under evaluation in the region. In addition, prophylactic human papillomavirus (HPV) vaccination for the prevention of infection and related disease is being considered as an additional cervical cancer control strategy. A concern against HPV vaccination is the issue that it could promote or encourage unsafe sexual behavior among adolescents.22 However the predominant reason for non-acceptance of the vaccine is its current high cost.
The need for expert cancer pathologists is rapidly growing, in parallel with the increasing incidence of cancer in Africa. According to the African-Oxford Consortium and World Health Organization, 15million new cases of cancer worldwide are projected by 2020, and 70% of these will be in developing countries.22 with special problems in Africa (Morris 2003).16 The main problems that need to be addressed in the East Africa region are the shortage of dedicated resources, the extremely low number of cancer registries and pathology departments, the geographic distances involved, the poor case abstraction, and the need for data collection from peripheral hospitals to centralized pathology laboratories. Obviously, these problems cannot be addressed only by international donors, or by single cancer registrars with good will. Government investments are needed to create the backbone on which projects for the development of cancer registries can be built. Almost all the histopathology laboratories in East Africa have no written standard operative procedures (SOPs) covering quality control and quality assurance policies, and no strict measures against biologic risk for technologists and pathologists.23 According to UICC (http://www. uicc.org/national-cancer-control-planning-nccp), cancer control plans are designed around five key questions: what is our country’s cancer picture? Who can help us develop and implement a cancer plan? What will be in our plan? How do we communicate and implement our plan? and how will we know if we are successful? Cancer registries would be best placed to take the central role in the first and the last question. For better planning, countries may also consider having a representative from their registries as members of any other steering committee or advisory group of the Health Authority.24
A set of cancer policy indicators should be developed by examination of current national and international approaches and an assessment of the evidence supporting cancer indicators. These indicators will help in monitoring specific policy recommendations and strategies. A report on policy indicators should then be presented each year to the Ministry of Health in each country. Indicators should be tracked such as percentage of the population who are smokers or overweight, alcohol consumption, incidence of cancer, uptake of screening, stage of presentation of common cancers, use of national, multidisciplinary guidelines, trends in outcome of cancer patients, waiting times from diagnosis to treatment. It is also recommended that all countries should establish core surveillance and information systems that allow them to monitor and evaluate epidemiological and programmatic data, and to use these data as a basis for appropriate decision making. Cancer surveillance is centered upon the population-based cancer registry as a core component of the cancer control strategy.25,26
Since in East Africa population-based screening has not taken root, early detection of cancer through any means must be a key element of an overall National Cancer Strategy. Early detection should encourage vigilance for signs and symptoms that may be indicative of early disease. It is based on the premise that it is easier to treat and cure the cancer if it is detected early. This is the best strategy for reducing cancer deaths. Early detection through breast awareness, prostate examination and skin inspection should be taught. An important component of early detection should be educating the public about the importance of recognizing symptoms, performing self-examination, and early presentation with any suspicious symptoms. Such initiatives should also include warning signs of cancer in children.
The author gratefully acknowledges the financial support of the Centre for International Governance Innovation (CIGI) and Africa Initiative (AI). The Author would also like to thank the staff at the Kampala Cancer Registry, Nairobi Cancer Registry, Gezira Cancer Registry and Sudan National Cancer Registry and the Eritrean Ministry of Health for sharing their experiences and helping by filling out the questionnaire.
The author declares no conflict of interest.

©2016 Fadlelmola. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.